Suprasellar Cystic Mass
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Enlarged Third Ventricle
Obstructive Hydrocephalus
Aqueductal Stenosis
Arachnoid Cyst
Craniopharyngioma
Neurocysticercosis (NCC)
Less Common
Rathke Cleft Cyst
Dermoid Cyst
Epidermoid Cyst
Enlarged Perivascular Spaces (PVSs)
Rare but Important
Pituitary Macroadenoma
Pituitary Apoplexy
Astrocytoma
Pilocytic Astrocytoma
Pilomyxoid Astrocytoma
Ependymal Cyst
Saccular Aneurysm
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Where does the mass originate?
Third ventricle: Think hydrocephalus > intraventricular cystic mass (ependymal cyst, craniopharyngioma)
Suprasellar cistern: Arachnoid, other congenital/infectious cysts
Pituitary gland/sella turcica: Necrotic/cystic neoplasm
Brain parenchyma: Enlarged perivascular spaces, cystic/low density neoplasm
Helpful Clues for Common Diagnoses
Enlarged Third Ventricle
CSF density/signal intensity
No enhancement (unless infection, neoplasm)
Obstructive Hydrocephalus
Can be intra- or extra-ventricular (noncommunicating or communicating)
If acute, periventricular “halo” of transependymal CSF
“Cystic mass” = dilated 3rd ventricle
Aqueductal Stenosis
↑ Lateral, 3rd ventricles
Normal 4th ventricle
Usually longstanding, “compensated” so no transependymal CSF
Arachnoid Cyst
10% of ACs suprasellar (SSAC)
Sharply marginated CSF density/signal intensity mass
Suppresses on FLAIR
Does not restrict on DWI
3rd ventricle elevated, displaced over AC
Displaces temporal lobes laterally
Displaces midbrain, pons posteriorly
Infundibular stalk typically displaced anteriorly
“Mickey mouse ears” on coronal = cyst + lateral ventricles
If large, may also cause obstructive hydrocephalus
Craniopharyngioma
90% of childhood craniopharyngiomas cystic
Cyst fluid hyperdense/intense to CSF
90% have some Ca++ (globular or rim)
90% enhance (rim, nodular)
Suprasellar cistern > > within 3rd ventricle
Neurocysticercosis (NCC)
Look for “clusters” of cysts in subarachnoid cisterns (“racemose” NCC)
Look for cyst + scolex
FLAIR best sequence to detect (cyst fluid doesn’t suppress completely)
Helpful Clues for Less Common Diagnoses
Rathke Cleft Cyst
60% purely suprasellar or intrasellar with suprasellar extension
Variable density/signal intensity
Usually ↑ compared to CSF
10% calcify (curvilinear, in cyst wall)
Look for
Intracystic nodule (45%)
“Claw” of compressed, enhancing pituitary displaced around cyst
Dermoid Cyst
Most common site = sellar/parasellar, frontonasal
Fat density/signal intensity
20% have capsular Ca++
Look for evidence of rupture
Fat droplets in subarachnoid spaces
Fat-fluid levels in ventricles
Chemical shift artifact in frequency encoding direction
Epidermoid Cyst
Rare in suprasellar cistern
Lobulated, insinuating growth pattern
> 95% hypodense (similar to CSF)
FLAIR, DWI best to distinguish epidermoid from AC, enlarged 3rd ventricle
Epidermoid doesn’t suppress completely, restricts on DWI
Enlarged Perivascular Spaces (PVSs)
Usually variable-sized “clusters”
Off-midline (basal ganglia)
Round or ovoid (basal ganglia), linear (white matter)
Like CSF on all sequences (contain interstitial fluid)
Suppresses completely on FLAIR
Does not restrict on DWI
Helpful Clues for Rare Diagnoses
Pituitary Macroadenoma
Solid ± intra- or extratumoral cysts
Extratumoral cysts may be trapped/enlarged PVSs or arachnoid cysts
Cysts often hyperdense/intense compared to CSF
Solid > rim enhancement
Pituitary Apoplexy
Rare; may be life-threatening (severe panhypopituitarism)
Necrotic pituitary with little/no enhancement (may show rim)
Hemorrhage may bloom on T2* (GRE, SWI)
Compression/edema of hypothalamus, optic chiasm/tracts may cause hyperintensity on T2WI
Restricts on DWI
Markedly hypointense on ADC
Astrocytoma
Pilocytic > > pilomyxoid astrocytoma
Most suprasellar astrocytomas are solid, not grossly cystic
Ependymal Cyst
Rare; 3rd ventricle least common site
Round/ovoid; CSF-like
Saccular Aneurysm
Aneurysms may be associated with true perianeurysmal cysts
Obstructed perivascular spaces posited as etiology
Partly or completely thrombosed may have “cystic”-appearing foci within clot
Rare
Acute thrombosis can present with panhypopituitarism, SAH
Imaging can mimic necrotic adenoma
Hypodense center, iso-/hyperintense rim on T1WI
Look for mixed age laminated clot
“Blooms” on GRE
Rim may enhance
Image Gallery
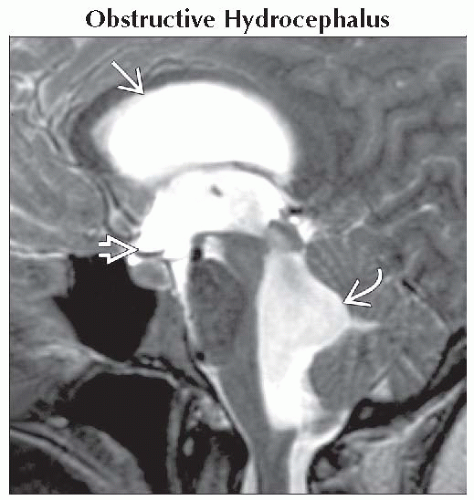 Sagittal T2WI MR shows EVOH with markedly enlarged lateral
 , 3rd , 3rd  , and 4th , and 4th  ventricles. A CSF suprasellar mass caused by an enlarged 3rd ventricle was diagnosed. ventricles. A CSF suprasellar mass caused by an enlarged 3rd ventricle was diagnosed.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|