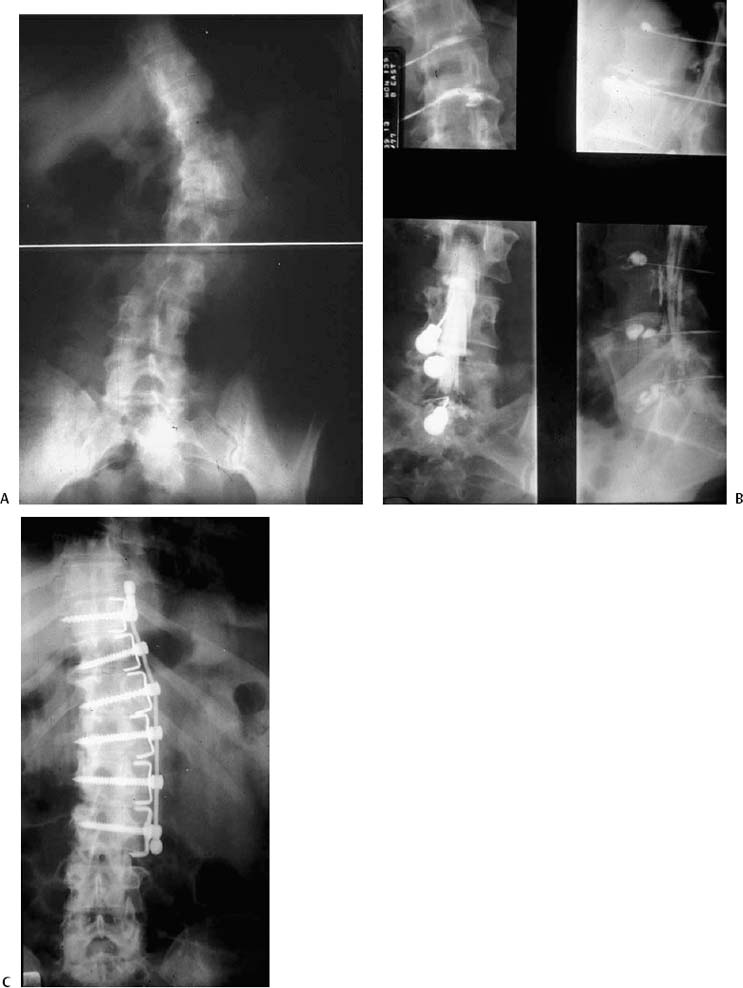
Chapter 21 Adult scoliosis may be defined as a lateral curvature of the spine in a skeletally mature individual. Adult scoliosis can further be subdivided into curves that began prior to skeletal maturity including idiopathic, congenital, and paralytic curves and those that arise de novo after skeletal maturity including those secondary to degenerative disease, iatrogenic causes, post-tramatic causes, and osteoporotic/osteomalacic curves. The largest proportion of patients seeking treatment by a spinal specialist will have curves that began as adolescent idiopathic scoliosis or those due to degenerative scoliosis. Although idiopathic scoliosis rarely leads to significant symptoms in the child, adults more commonly experience pain, changes in sagittal balance, and curve progression as the result of degenerative changes in the spine. Many investigators have shown that idiopathic curves have the potential to progress after skeletal maturity, which may lead to clinical symptoms.1–5 In addition to the symptoms of increasing back pain and truncal imbalance, older adults commonly experience symptoms related to osteoporosis and spinal stenosis. Some patients present for management of complications resulting from a prior operation to treat their spinal deformity, such as an iatrogenic flat back, pseudarthrosis, or a degenerated adjacent spinal segment. In the past, conservative measures were the mainstay of treatment recommendations for adult deformities because surgical correction for major spinal deformity presented substantial risks. In 1968, Nachemson estimated the risks related to adult deformity correction to include a 5% risk of death, 6% risk of a major neurologic deficit, 20% risk of significant correction loss, 10% risk of a deep infection, and a 40% risk of a major medical complication.6 Fortunately, the techniques for achieving and maintaining correction of spinal deformities have improved significantly since that time as have the perioperative management strategies. However, correction of a major spinal deformity in an older adult remains one of the most challenging procedures in the field of surgery. The history of modern surgical techniques for spinal deformities began with the advent of Harrington rods7,8 and included many pioneers such as Dwyer,9 Luque,10–12 Zielke,13 and Cotrel-Dubousset14,15 who played a role in the development of spinal instrumentation systems and in providing an ever-improving understanding of the treatment for spinal deformities. Although the Harrington system worked reasonably well for a simple thoracic deformity, fusions of the lumbosacral region often resulted in loss of lordosis or pseudarthrosis. In 1978, a review undertaken on behalf of the Scoliosis Research Society demonstrated significant loss of lumbar lordosis in 4% of scoliosis fusions, a problem that often led to poor clinical outcomes. After the recognition in the late 1970s that posterior distraction of the lumbosacral spine using Harrington rods commonly led to a flat-back deformity, posterior segmental fixation systems and pedicle screws with contoured rods were developed and have significantly reduced the incidence of this problem. Parallel to the improvements in surgical technique have been improvements in anesthesia techniques, spinal cord monitoring, and perioperative medical management and postoperative care, which have dramatically increased the sophistication and safety of modern spinal deformity correction. The modern approach to adult deformities involves a team of specialists including the reconstructive spinal surgeon, anesthesiologist, intensive care specialist, physical therapist, nutritionist, rehabilitation physician, and orthotist. In this chapter, we will discuss the scope and approach to the adult with a spinal deformity. Shands and Eisberg studied 194,060 chest radiographs in the state of Delaware in 1953 (82.2% of the entire state population over the age of 14) and found a spinal curve in 1.9% including 1.4% with mild curves (10 to 19 degrees), 0.3% with moderate curves (20 to 29 degrees), and only 0.2% with curves greater than 30 degrees.16 Kostuik and Bentivoglio reported a 3.9% prevalence of structural curves in the adult thoracolumbar and lumbar spine during a review of 5000 intravenous pyelograms.17 The risk of curve progression after skeletal maturity for idiopathic scoliosis has been studied by Weinstein and Ponsetti18 who followed a cohort of 102 patients with idiopathic scoliosis an average of 40.5 years and reported that 68% of curves progressed in adulthood. Although curves less than 30 degrees tended not to progress, curves between 50 and 75 degrees had a high risk of progression over the follow-up period. Risk factors for curve progression included a lumbar curve, a curve involving a poorly seated fifth lumbar vertebra, and apical vertebral rotation of more than 33%. Other risk factors for progression include significant trunk imbalance, sharp angular curves in the lumbar spine, and curves emanating from the lumbosacral junction. Because these patterns often present the greatest technical difficulty for correction in later adult life, they are best treated surgically at an earlier age, if possible. Fowles and Drummond19 studied the effected of untreated scoliosis on quality of life in adults and concluded that the presence of a severe spinal deformity could be disabling. Although most patients experienced some back pain, up to one quarter of the patients in their study experienced disabling symptoms as a result of their deformity. In addition, many adults with spinal deformities reported embarrassment as a result of their spinal deformity, and women, in particular, were less likely to marry. The authors also noted socioeconomic consequences in adults with scoliosis. In contrast, Weinstein et al.,20 Nachemson,6,21 and Nilsonne and Lundgren22 believed that disabling pain was rarely a significant clinical problem in the adult with scoliosis. In one study, the overall prevalence of pain in adults with idiopathic lumbar and thoracolumbar scoliosis was found to be 60%, a rate similar to age-matched controls.17 However, the prevalence and severity of pain complaints increased significantly for curves that were greater than 45 degrees and for curves involving the lumbar spine. In contrast, thoracic curves were much less likely to be the source of significant pain symptoms but led to significant pulmonary dysfunction when associated with thoracic lordosis. The highest incidence of pain complaints is normally observed between the fifth and seventh decades of life in the scoliotic population. Although the majority of patients with scoliosis are able to carry out productive lives, the adult deformity population is less likely to function well in highly physically demanding forms of work and is more likely to miss work or become disabled due to back problems compared with the general population. Guigui studied factors affecting the function of adults with scoliosis and identified three anatomic elements associated with a declining function. These included the development of thoracolumbar kyphosis, increased rotatory translation of lumbar vertebral segments, and degenerative changes in the lumbosacral area.23 In a similar study, Schwab et al. found that lateral vertebral olisthesis, L4 end-plate obliquity, poor lumbar lordosis, and thoracolumbar kyphosis significantly correlated with symptoms of pain.24 Engsberg et al. found that gait was affected in adults with scoliosis leading to lower walking velocities for patients with lumbar deformities compared with age-matched controls.25 Deviren et al. found that curve magnitude and age were the greatest predictors of curve stiffness and pain symptoms. Curves greater than 40 degrees demonstrated decreased flexibility with every 10-degree increase in coronal deformity resulting in diminished flexibility by 10%. Similarly, each decade of life diminished curve flexibility by 5% in the major curve and 10% in the lumbosacral fractional curves.26 During the history, the physician must gain a thorough understanding of the location and severity of any symptoms and should assess the effectiveness of prior treatments for the condition. It is important to understand how the deformity affects the patient’s life including the effect on activities of daily living, occupation, social function, recreation, and sexual functioning. Some patients will have significant concerns about the aesthetics of the deformity, and these issues should be discussed. A family history of progressive deformity should be sought, and the onset and progression of the patient’s deformity should be defined. Clinical clues to deformity progression can include changes in height, clothing fit, or body shape (rib hump or altered waistline). Ideally, a more precise documentation of curve progression should be obtained from serial radiographs if available. The visual analogue scale can be used to quantify pain symptoms. Pain drawings are useful in eliciting the location and radiation of symptoms. Pain at the apex of the curve should be differentiated from pain at a remote site. Often, a radicular or referred component to the pain will be present in older adults. When assessing leg symptoms, scleratomal referred pain should be differentiated from a true radiculopathy, which generally indicates neural element compression. Patients with severe thoracic or thoracolumbar curves may present with intercostal neuralgia due to the associated deformities of the rib cage. Bladder or bowel dysfunction may occasionally be present in the setting of severe spinal stenosis. The general impact of the spinal condition on a patient’s health and mental functioning may be assessed using validated outcome measures. Schwab et al. analyzed SF-36 scores in adult scoliosis patients and found lower scores in seven of eight categories including physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotion, and mental health compared with the general U.S. population.24 Patients with lumbar deformities and loss of lordosis demonstrated particularly poor values in the social function, role emotion, and overall general health categories. In another study, Berven et al. analyzed the modified Scoliosis Research Society outcomes instrument (SRS-22) and the SF-36 in adults with scoliosis and found significantly lower scores compared with unaffected controls in every domain of these scales.27 Physical examination should include a broad assessment of the musculoskeletal and neurologic systems. The three-dimensional characteristics the spine such as the magnitude and location of the spinal curves, the sagittal plane balance (e.g., kyphosis or lordosis relative to normal), the rib hump, the degree of decompensation, curve flexibility, pelvic obliquity and hip mobility should be determined. Older adults with severe deformities may complain of pain from abutment of the rib cage against the iliac wing, which can be determined by physical examination. The neurologic examination should be thorough and include a search for subtle neurologic abnormalities associated with spinal cord dysfunction. Example of significant findings may include a left thoracic curve, mild clawing of the toes, asymmetry of the abdominal reflexes, or subtle balance/gait difficulties, which could indicate a syringomyelia, tethered cord, or neuromuscular syndrome. Body habitus is important to assess and can affect the treatments offered. Obese patients often benefit from weight loss, which may improve the symptom of axial pain. Poor nutrition is commonly seen in the elderly spinal deformity population and should be corrected prior to any planned surgical intervention to diminish the odds of infection and other peri-operative complications. The initial radiographic studies include 36 in., standing posterior/anterior (PA), and lateral radiographs. It is important to ensure that the patient straightens their knees during the lateral radiograph to allow the detection of sagittal imbalance. Focal or coned views of specific regions of the spine are helpful to evaluate facet arthritis, congenital anomalies, and disk-space narrowing. Oblique radiographs using Stagnara views are useful to assess kyphosis in the setting of severe rotational deformities.28,29 Lateral bending radiographs may be used to predict a curve’s flexibility but do not necessarily predict the degree of surgical correction obtained at surgery. Flexion and extension views are useful in assessing the flexibility of a sagittal plane deformity and may reveal levels with abnormal motion or instability. Traction films, push-prone films, and supine films taken with a bolster under the apex of a kyphosis can be used to assess flexibility or response to a corrective maneuver. If radicular pain or neurologic findings are present, an advance three-dimensional imaging should be performed. In the setting of a major spinal deformity, we prefer CT/myelography over MRI because the latter test is frequently difficult to interpret due to the nonorthogonal nature of the deformed spine. It is particularly important to assess sites of actual or potential cord compression prior to surgery when corrective maneuvers are planned that might compromise the neural elements. Adults with spinal deformities involving the lumbar spine often benefit from MRI of this region to assess the health or degeneration status of the lower lumbar disks. Unfortunately, there is a poor correlation between the appearance of the lower lumbar disks on imaging studies and the presence of pain, and therefore provocative diskography has been useful in our hands to assess the lumbosacral region if fusion to this area is contemplated. The senior author experienced a 30 to 35% rate of persistent pain even after attaining a solid fusion in adult deformity patients in his early years of practice. However, in recent years, the number of adult deformity patients with persistent pain has declined. One reason for this change is believed to be the use of diskography to assess for painful segments that should be included in the fusion.30–32 Specifically, the L3-L4, L4-L5, and L5-S1 levels are generally assessed with diskography and the information gained is used to help in planning the distal fusion level (Figs. 21–1A, 21–1B, and 21–1C). Facet blocks are also occasionally employed to assist in defining painful segments (especially L5-S1) that should be included in the fusion. At the lumbosacral junction, the sacrum is included in the fusion if diskography produces significant pain and facet blocks relieve the pain. However, a degenerated segment that is not painful with diskography or relieved with facet blocks is not incorporated into the fusion. The basic approach to nonoperative care for adult deformity patients is similar to the treatment of nondeformity patients. Useful modalities include exercise, patient education, nonsteroidal anti-inflammatory drugs (NSAIDs), and activity modifications. It is important for the patient to understand that conservative care will not prevent curve progression but may improve function, stamina, and quality of life. In particular, low-impact aerobics, cycling, and swimming are useful in older adults with painful spinal deformities. Active exercises also help to prevent osteoporosis, a condition that serves to worsen an existing spinal deformity. Patients at risk for osteoporosis should be screened with bone densiometry and started on pharmacologic treatment when low bone density is documented. Although there is no evidence to suggest that bracing will prevent curve progression in adults, the use of orthotics may occasionally be helpful. Orthotic choices range from soft corsets to rigid, underarm braces carefully fitted to the patient’s deformity. Unfortunately, patient tolerance with rigid bracing is generally poor. The general indications for surgery in the adult deformity patient include (a) persistent pain, unresponsive to conservative measures; (b) significant deformity progression; or (c) neurologic involvement. A lesser concern that may be considered is the perception of very poor cosmetic appearance on the part of the patient. Figure 21–1 (A) A 38-year-old female with increasing low back pain and deformity. (B) Provocative diskography revealed normal L5-S1, L4-L5, and L3-L4 disks (no pain on injection) but abnormal morphology and pain reproduction at the L2-L3, L1-L2, and T12-L1 levels. (C) Anterior fusion of T10-L3 was performed using Dwyer instrumentation. The patient became asymptomatic and continues to do well at 30-year follow-up. Pain is the most common indication for surgical intervention in adults and is the major factor for which surgery is considered in 85% of adult deformity surgical cases. Unfortunately, determining the exact sources of pain and predicting pain relief after surgery is a great challenge. As with other painful conditions of the spine, the more certain a surgeon can be as to the cause of pain, the more likely surgical intervention is to be successful.
Surgery for Adult Spinal Deformity
♦ Adult Scoliosis
Definition and Features
Incidence and Function
♦ Patient Evaluation
History
Physical Examination
Imaging Studies
Ancillary Tests Including Diskography and Facet Blocks
♦ Nonoperative Treatment
♦ Surgical Treatment
Indications for Surgical Treatment
General
Pain
Progressing Deformity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree