Chapter 10 Sympathetic Nerve Block and Neurolysis
Preoperative preparation
 The operator must have a full understanding of the relevant anatomy and the pathophysiology of the underlying condition, because the complications of sympathetic blocks can be very serious.
The operator must have a full understanding of the relevant anatomy and the pathophysiology of the underlying condition, because the complications of sympathetic blocks can be very serious. Secure venous access is essential for all patients, and facilities for the treatment of hypotension must be available. An intravenous fluid preload with crystalloid solution is usually given for all blocks (e.g., splanchnic, celiac, lumbar sympathetic, or superior hypogastric plexus block).
Secure venous access is essential for all patients, and facilities for the treatment of hypotension must be available. An intravenous fluid preload with crystalloid solution is usually given for all blocks (e.g., splanchnic, celiac, lumbar sympathetic, or superior hypogastric plexus block).Instrumentation
For sympathetic nerve block, the following equipment is required:
Also, 99% alcohol is needed for chemical neurolysis.
The instrumentation required for radiofrequency lesioning is described in Chapter 8 (Figs. 8-14 to 8-16).
Contraindications
 Coagulopathy (International Normalized Ratio (INR) value > 1.5 or platelet count < 50,000/mm3) or prescribed anticoagulant therapy. There is significant risk of vessel injury in a patient with either condition, because the sympathetic trunks are deeply placed and close to major blood vessels. A large hematoma may be produced if the patient has a coagulation disorder. Aspirin or antiplatelet agents should be stopped 7 days, and warfarin 5 days, before injection is performed.
Coagulopathy (International Normalized Ratio (INR) value > 1.5 or platelet count < 50,000/mm3) or prescribed anticoagulant therapy. There is significant risk of vessel injury in a patient with either condition, because the sympathetic trunks are deeply placed and close to major blood vessels. A large hematoma may be produced if the patient has a coagulation disorder. Aspirin or antiplatelet agents should be stopped 7 days, and warfarin 5 days, before injection is performed. Local infection or neoplasm at the needle trajectory: There is a risk of spreading the infection to deeper structures.
Local infection or neoplasm at the needle trajectory: There is a risk of spreading the infection to deeper structures. Anatomical or vascular anomalies: Anatomical distortion, such as pressure from a neoplasm or spinal scoliosis, may make the block more difficult and reduce the chance of success. Anomalous vessels increase the risk of accidental needle puncture.
Anatomical or vascular anomalies: Anatomical distortion, such as pressure from a neoplasm or spinal scoliosis, may make the block more difficult and reduce the chance of success. Anomalous vessels increase the risk of accidental needle puncture. Uncorrected severe hypovolemia: Splanchnic, celiac, and lumbar sympathetic blocks can precipitate marked hypotension, especially when performed bilaterally.
Uncorrected severe hypovolemia: Splanchnic, celiac, and lumbar sympathetic blocks can precipitate marked hypotension, especially when performed bilaterally.Procedures
Stellate Ganglion
Anatomy
The stellate ganglion, which is formed by the fusion of the inferior cervical and T1 sympathetic ganglia, lies anterior to the transverse processes of C7 and T1 and to the neck of the first rib (Fig. 10-1).
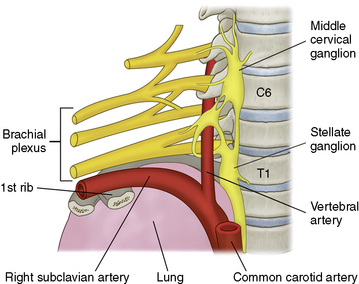
Figure 10–1 Position of the stellate ganglion. C6, sixth cervical vertebra; T1, first thoracic vertebra.
(Modified from Justins DM: Pain and autonomic nerve block. In Wildsmith JAW, Armitage EN, McClure JH [eds]: Principles and Practice of Regional Anaesthesia, 3rd ed. Edinburgh, Churchill Livingstone, 2002, pp 291-309.)
Temperature measurements in both hands (Fig. 10-2) are required to evaluate successful upper extremity block [1]. Digital infrared thermal imaging is helpful (refer to Fig. 15-29) [2]. Horner syndrome does not guarantee success of ipsilateral upper extremity sympathetic block.
Technique
Stellate ganglion block
Pulsed radiofrequency lesioning or radiofrequency thermocoagulation of the stellate ganglion
The stellate ganglion formed by the fusion of the inferior cervical and the first thoracic ganglion as they meet anterior to the vertebral levels of the C7 and T1 vertebra. The ganglion lies on the longus colli at the vertebral level covered by prevertebral fascia and is surrounded by important structures, such as common carotid artery, internal jugular vein, thyroid, vagus nerve, phrenic nerve, and brachial plexus. The distance from the junction of the transverse process and the vertebral body to the stellate ganglion may show individual differences according to the individual shape and volume of longus colli. We, therefore, cannot estimate where the ganglion is on the lateral image of C-arm. In addition, the location of the ganglion is also highly variable. We, also cannot estimate where the ganglion is on the AP image of C-arm. When we use the radiofrequency lesioning techniques (Fig. 8-16) we should remember how and where the lesion is made. If radiofrequency needle tip rests at the junction of the transverse process and the vertebral body, where the radiofrequency lesion is made? These are the reason why we do not perform the procedure under the guidance of fluoroscope.
Thoracic Sympathetic Ganglion
Anatomy
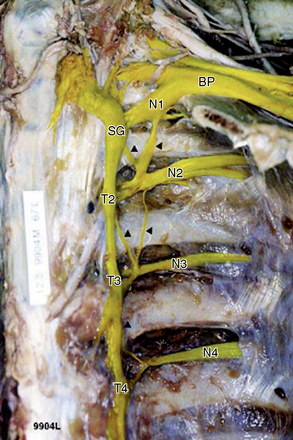
The upper thoracic sympathetic ganglia are located around the heads of the ribs and are covered by the pleura. The lower two or three ganglia are on the sides of the vertebral bodies. The thoracic sympathetic trunk runs between the ganglia and just in front of the somatic nerves (Fig. 10-4) [1].
Techniques
Thoracic sympathetic block
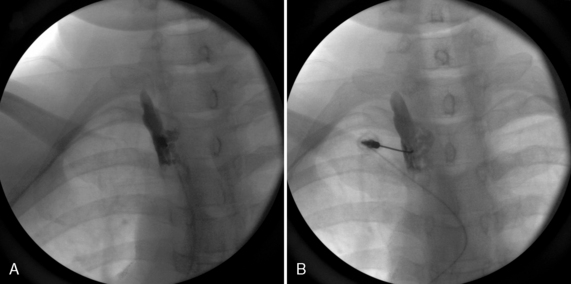
The following procedure is used for thoracic sympathetic block:
Splanchnic Nerve
Anatomy
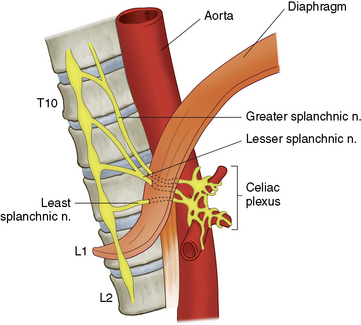
As shown in Figure 10-6, the greater (T5 through T10), lesser (T10 and T11), and least (T11 and T12) splanchnic nerves cross the lateral side of the body of T12 as they sweep forward to penetrate the diaphragm and form the celiac plexus. The pleura are attached posteriorly to the vertebral bodies and create a well-defined compartment.
Techniques
Splanchnic nerve block
The procedure for splanchnic nerve block is as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree