Syncope
Mark S. Quigg
Thomas P. Bleck
Introduction
The term syncope, from the Greek for “cutting short,” refers to an abrupt and transient loss of consciousness accompanied by loss of muscular tone. It is usually caused by a sudden, global reduction in cerebral perfusion, and clinical recovery occurs with restoration of normal cerebral blood flow. The very transience of this syndrome and the variety of medical disorders that can cause or mimic it are at the core of the diagnostic problems that the neurologist faces.
Definitions
Patients and physicians alike use a variety of terms to describe an occurrence of syncope. The term fainting is often used synonymously with syncope and captures the essential criteria— loss of consciousness and muscle tone. If the symptoms differ only in degree, so that there is partial loss of consciousness with a near fall, the term presyncope is often used. Less specific terms, such as passing out, blackout, or dizziness, need further clarification to become diagnostically useful. Some clinicians restrict the meaning of drop attacks to episodes of transient loss of tone with preservation of consciousness, a definition that carries a different burden of etiologies than does syncope.
Incidence and Prognosis
When measured in studies of consecutive emergency room visits, syncope prompts about 3% of emergency room evaluations, a proportion that has changed little over the last 25 years.9,14,56 Multicenter surveys estimate that of 865 million emergency room visits between 1992 and 2000, 6.7 million (0.77%) were related to syncope.78
Although no age is spared, the incidence of syncope is highest among the elderly. A study of 711 elderly patients revealed a 10-year prevalence of 23% and a yearly incidence of 7%.52 Of those who are admitted to hospital, 59.9% are age 70 years or older.79 In addition to increasing age, other factors leading to higher rates of hospitalization are female gender and white race.78
The incidence of syncope among children and adolescents is 1.25%, peaking in the 15- to 19-year-old group.20 Young athletes at a mean age of 16 years report that 6.2% had syncope within the last 5 years.10
Diagnosis is important because the mortality of syncope varies widely with the underlying etiology. Kapoor determined the 5-year outcome of 433 patients evaluated for syncope.41 Mortality is >50% in patients with a cardiac cause of syncope, compared to 30% in patients with a noncardiac cause and 22% with an unknown cause.
Data from the Framingham Heart Study emphasize that syncope from cardiac causes is often a harbinger of significant coronary disease.76 In this study, 822/7,814 (10.5%) individuals reported syncope over a 24-year period, for an overall incidence of first report of syncope of 6.2/1,000 person-yr. The relative hazard rate experienced by those with syncope from any cause compared to those without syncope is 1.31. Cardiac syncope has the highest relative risk of death than any other cause of syncope at 2.01 and an especially high risk of death related to coronary artery disease (relative risk 2.66). The Framingham study also emphasizes that those whose etiology of syncope remains unknown do not necessarily experience a benign course, having a relative risk of death from any cause of 1.32.
Older age appears to increase the risk of mortality in cardiac syncope. Another study by Kapoor that compared mortality rates of patients <60 and >60 years of age found that although the 2-year mortality rate was 27% in the older and 8% in the younger group, cardiovascular causes remained the most significant risk factor for mortality in either.43 In the elderly, syncope carries a greater mortality despite etiology. In elderly patients hospitalized for syncope, the 4-year mortality was 41%, with the relative risk of cardiac syncope not varying significantly from that of noncardiac syncope.30
Morbidity associated with trauma from syncopal falls also contributes to the costs related to syncope. Between 16% and 36% of patients presenting with syncope experience a range of injuries from minor lacerations and bruises to fractures of the hip, face, or limbs.14,41
The morbidity of syncope goes beyond the physical. Assessments of the functional status of patients with chronic syncope show degrees of psychosocial impairment similar to those experienced by patients suffering from other disabling diseases such as rheumatoid arthritis or low back pain.51
The frequency of recurrence of syncope is not especially helpful in characterizing patients by etiology or prognosis,41 although each syncopal episode increases the probability of serious injury. In Kapoor’s study of 433 syncopal patients followed for 5 years, 153 had one or more recurrences, and the mean number of recurrences was greater than six.41 Whether the diagnosis was cardiac, noncardiac, or unknown, recurrences were common in every category.
The 2000 Healthcare and Utilization Project estimates the annual cost of syncope-related hospital admissions in the United States at $2.4 billion, placing syncope on par with asthma ($2.8 billion) and human immunodeficiency virus ($2.2 billion).78 The estimated cost per patient is $5,400. The high cost reflects the difficulties in establishing a diagnosis of a syndrome having both a wide range of possible etiologies and a high rate of studies returning nondiagnostic results. These problems have led to the publication of guidelines on evaluation and hospitalization of syncope, the adherence to which, some report, leads to higher yields in diagnostic accuracy but to no clear reductions in cost.16,26 Other clinicians, however, report success in cost reduction, test reduction, and health benefits in the use of specialized syncope units and protocols of risk stratification and evaluation.45,74
Clinical Description
Classic Symptoms
The prodromal symptoms of classic syncope are familiar to most physicians and consist of nausea, “clammy” sweating, visual blurring and “graying out,” tinnitus, lightheadedness, and dizziness. The patient appears ashen or pale and becomes diaphoretic. Mydriasis may occur with tachypnea and bradycardia. Witnesses frequently note that the victim’s “eyes rolled back into the head,” reflecting fading extraocular muscle tone. The patient becomes diffusely weak and hypotonic and, as consciousness is lost, falls to the ground with lack of protective reflexes if unsupported. Within seconds to minutes, once the patient is horizontal, color, pulse, and consciousness return. During the anoxic phase, before the patient recovers consciousness, a few myoclonic jerks or even more rhythmic, clonic movements may appear. Such a syncopal convulsion is common and often leads to erroneous reports of epileptic seizures. Sequelae include continued nausea and generalized malaise, but drowsiness, confusion, and amnesia are limited.
Syncopal Myoclonus
These common clinical features have been confirmed by video analysis of syncope induced in healthy volunteers through ocular pressure, hyperventilation, and Valsalva maneuver.49 Typical prodromal symptoms were blurred vision, dizziness, vertigo, and nausea. Average duration of loss of consciousness was about 12 seconds, and myoclonic activity (syncopal convulsions) occurred in 38/42 syncopal episodes. Automatisms were observed in nearly 80%. Opened eyes and upward eye deviation were also common. Auditory and visual hallucinations, not usually elicited in previous studies, were reported in 60%. Postictally, transient amnesia occurred in 1 of 42 individuals, but cognitive sequelae were otherwise unremarkable. In none of these normal individuals nor in other studies of induced syncopal convulsions in patients did incontinence occur.2,34,49
Of the manifestations of syncope, convulsive movements are potentially the most confounding because they raise the question of epileptic seizures. Studies of syncopal convulsions induced in patients during cardiac electrophysiology studies,2 positive tilt-table studies,34 and in healthy volunteers49 describe a prevalence of 45% to 90%.
Myoclonic activity during a syncopal convulsion is usually multifocal and arrhythmic, but generalized, rhythmic myoclonus is also common.36,49 In our experience, biased by patients admitted for diagnosis in epilepsy monitoring units, dystonic posturing similar to that of a complex partial seizure is not unusual and adds further difficulty in the purely visual distinction between syncopal and epileptic motor activity. This opinion is supported by a large study (694 individuals) of symptoms provoked by tilt-table testing; 8% of participants with positive results (n = 222) had “neurologic events” consistent with the clinical behaviors of tonic–clonic seizures, focal seizures, or dysarthria or aphasia.63
Electroencephalographic Appearance
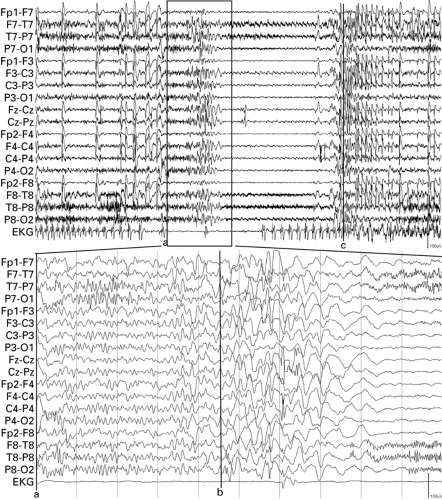
Electroencephalographic recordings document the electrophysiologic correlates of syncopal convulsions. In patients with vasovagal syncope who have attacks induced by tilt-table, the electroencephalogram (EEG) demonstrates gradual development of high-amplitude 3- to 5-Hz slowing during prodromal symptoms. Slow-wave frequency decreases to 1- to 3-Hz activity with loss of consciousness.36 In recordings of cardiac syncope caused by ventricular arrhythmias,2 electrographic findings are more variable and sometimes feature marked attenuation of cortical activity with loss of consciousness, although in most cases, rhythmic slowing occurs before voltage attenuation. The changes in EEG occur about 10 to 15 seconds after development of arrhythmia. It is of interest that brain-slice preparations deprived of oxygen show a time of onset to isoelectric activity of about 7 minutes,64 which implies that corticothalamic activity comprising scalp EEG is more susceptible to hypoxia than individual cortical neurons. Normal background activity returns quickly with restoration of circulation and return of consciousness. Myoclonic activity has no consistent relationship with the EEG changes, and could occur either before or after EEG attenuation.2 In neither study were epileptiform or ictal discharges observed.2,36 Both the duration of loss of consciousness and postsyncopal confusion are linearly related to the duration of cardiac dysfunction.2 Figures 1 and 2 demonstrate typical EEG accompaniments in syncope induced by cardiac asystole and in reflex bradycardia induced by breath-holding.
Differential Diagnosis
Because neurologists and epileptologists can be expected to see a more selected patient group than cardiologists, general practitioners, and emergency room physicians, the bulk of this discussion focuses on the separation of neurologic causes of syncope from other etiologies. However, because neurologic causes are relatively infrequent, a discussion of the differential diagnosis of syncope is undertaken first.
As Table 1 shows, even a brief listing of causes of syncope can be daunting. A more concise method is to group the myriad causes onto five main categories: (a) disorders of orthostatic intolerance; (b) primary cardiac dysfunction; (c) transient neurologic dysfunction; (d) metabolic derangement; and (e) psychiatric syndromes. The relative frequency of these diagnostic groups as they present in emergency rooms and other primary care facilities is shown in Table 2.
Disorders of Orthostatic Intolerance
Disorders of the homeostatic mechanisms of blood pressure maintenance comprise a large portion of syncope seen by physicians. In these disorders, the unifying pathophysiology is the abnormal or insufficient response of the peripheral vascular system and in reflex cardiac mechanisms to internal or external stimuli.
To briefly review, on standing, about 300 to 800 mL (about 25% of total blood volume) is displaced downward from the thorax. Reduced pressure is detected by receptors in the carotid sinus and aortic arch and within cardiac and pulmonary tissues. Tonic central sympathetic inhibition decreases, which allows an increase in peripheral vascular resistance and an increase in heart rate as mediated by medullary cardiovascular control centers.81 Defects in this regulatory system lead to orthostatic hypotension, which can be due to degeneration of the autonomic nervous system either centrally, as in Shy-Drager syndrome, or peripherally as the result of acquired or hereditary neuropathies. An intact autonomic nervous system, on the other hand, may be unable to compensate for conditions causing hypovolemia, such as anemia or dehydration. Elderly patients have particular problems with compensatory cardiovascular regulation and are vulnerable to orthostasis whatever the cause.43
One of the more important causes of syncope in older people is orthostatic hypotension induced by drugs. In a study of elderly, institutionalized patients, hypotensive adverse effects
of drugs caused 8 of 32 cases of noncardiogenic syncope.52 Nitrates, levodopa, and thioridazine were cited this study, but any new medication, especially one that antagonizes the alpha-1 receptor such as amitriptyline or chlorpromazine, should be suspect in any elderly patient with syncope.
of drugs caused 8 of 32 cases of noncardiogenic syncope.52 Nitrates, levodopa, and thioridazine were cited this study, but any new medication, especially one that antagonizes the alpha-1 receptor such as amitriptyline or chlorpromazine, should be suspect in any elderly patient with syncope.
Current consensus divides disorders of orthostatic intolerance into three groups, as follows.3
Reflex Syncope
Reflex syncope is a group of disorders that occur because of a sudden failure of the cardioregulatory system to maintain adequate vascular tone during orthostatic stress, resulting in hypotension that is frequently associated with bradycardia.
Neurocardiogenic syncope (or vasovagal syncope) is a reflex syncope believed to result from an inappropriately hypercontractile response of the heart to abrupt venous pooling. The resulting state mimics hypertension and causes a compensatory but pathologic bradycardia, initiating syncope.35 In susceptible individuals, neurocardiogenic syncope is triggered by strong emotions such as fear or follows painful stimuli such as venipuncture, dental procedures,22 or prostate exams.5 Sometimes the precipitating event is merely a prolonged upright stance, as is frequently required of soldiers standing at attention. In this situation, there is also the confounding variable of venous pooling in the legs because gastrocnemius and soleus muscle contraction ceases. Soldiers who are taught to keep their knees slightly flexed and to intermittently contract their leg muscles are at much lower risk of syncope.
Hypersensitivity of peripheral visceral afferents, whether idiopathic or the result of trauma or tumor, is another mechanism of reflex syncope. Asystole after carotid massage is the hallmark of carotid sinus hypersensitivity. Neuralgic syncope is associated with tumors or other pathology of the
glossopharyngeal nerve, and there are rare cases of syncope associated with trigeminal neuralgia well.40
glossopharyngeal nerve, and there are rare cases of syncope associated with trigeminal neuralgia well.40
A variety of seemingly prosaic activities such as coughing, micturition, defecation, and breath-holding are all subsumed under the term situational syncope. Each stimulus, as in the Valsalva maneuver, leads to syncope through neurally mediated vasodepression analogous to vasovagal syncope. Micturition syncope may in addition reflect the relief of pressure exerted by the bladder on the inferior vena cava producing a transient decrease in venous return.
Autonomic Failure
Autonomic failure, either from primary degeneration of the autonomic nervous system, as in Shy-Drager syndrome (multiple-system atrophy) or that secondary to peripheral neuropathies, is the second major category of disorders of orthostatic intolerance.
Pure autonomic failure syndrome27 is a chronic, insidious-onset disease with syncope as one major symptom accompanied by other failures of the autonomic nervous system (anhydrosis, impotence, etc.) that, unlike multiple-system atrophy, is not accompanied by a movement disorder or cognitive deficits.27
Other autonomic failure syndromes are usually attributable to small-fiber peripheral neuropathies resulting from such diseases as diabetes mellitus or paraneoplastic syndromes. In the case of diabetes mellitus, autonomic neuropathies can present quite early and severely coincident with other evidence of the disease.72
Postural Orthostatic Tachycardia Syndrome
Postural orthostatic tachycardia syndrome (POTS) is the third major category of orthostatic intolerance and consists of excessive increases in heart rate in the upright position.35 The
partial dysautonomic form is believed to be due to insufficient increases in peripheral vascular resistance on standing and may be a precursor to more severe primary autonomic failure. The second form consists of an initially appropriate tachycardic response to standing that does not “turn off,” thus causing symptoms of presyncope and palpitations along with postural hypertension and tachycardia. The latter is often called beta-hypersensitivity syndrome because isoproterenol infusion causes a marked increase in heart rate. Investigation is underway to confirm a genetically mediated basis for these disorders.73
partial dysautonomic form is believed to be due to insufficient increases in peripheral vascular resistance on standing and may be a precursor to more severe primary autonomic failure. The second form consists of an initially appropriate tachycardic response to standing that does not “turn off,” thus causing symptoms of presyncope and palpitations along with postural hypertension and tachycardia. The latter is often called beta-hypersensitivity syndrome because isoproterenol infusion causes a marked increase in heart rate. Investigation is underway to confirm a genetically mediated basis for these disorders.73
Primary Cardiac Dysfunction
Cardiac causes comprise disorders of pump failure caused by obstructed outflow, impaired cardiac filling, shunting, myocardial ischemia, or arrhythmias. The large but not all-inclusive list shown in Table 1 includes typical primary and secondary causes of episodic pump failure. Most of these disorders are distinguished from epilepsy by standard and invasive electrophysiologic tests or by specific aspects of the history or physical examination.41
The long-QT syndrome of Romano-Ward is an autosomal-dominant disorder of cardiac repolarization that results in ventricular tachycardias leading to palpitations, syncope, and sudden death. It is a channelopathy of cardiac hERG potassium or voltage-gated sodium channels71 that is easily confused with epilepsy because patients are often young and usually have had unprovoked syncopal convulsions and the family history reveals similarly affected relatives. Other genetic long-QT syndromes, such as the Jervell-Lange-Nielsen syndrome, have different modes of inheritance and different channel abnormalities.1 The electrocardiogram (ECG) is diagnostic, demonstrating a long, corrected QT interval. A large number of drugs and other precipitants have more recently been associated with acquired prolonged-QT syndromes.69 These latter patients may not have prolongation of repolarization at
baseline. One should also consider the Brugada syndrome, an autosomal-dominant disorder consisting of syncope, sudden death, ECG with ST-segment elevation, and an appearance similar to a right-bundle-branch block in the anterior leads.80
baseline. One should also consider the Brugada syndrome, an autosomal-dominant disorder consisting of syncope, sudden death, ECG with ST-segment elevation, and an appearance similar to a right-bundle-branch block in the anterior leads.80
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree