Fig. 46.1
Corticosteroid therapy for lymphoma. Initial FLAIR (a) and post-contrast T1-weighted (b) MR images show patchy edema and enhancement within the left midbrain (arrows). Follow-up FLAIR (c) and post-contrast T1-weighted (d) MR images obtained after corticosteroid administration show considerable interval decrease in the edema and abnormal enhancement (arrows)
Epidural Lipomatosis. Epidural lipomatosis is characterized by pathologic overgrowth of normal fat in the epidural space and is problematic when it causes spinal stenosis and/or cord compression. Glucocorticoids increase hydrolysis of circulating triglycerides, thereby increasing the amount of fatty acids in circulation and available for ectopic fat distribution. Glucocorticoids also increase de novo lipid production in the liver and in adipocytes and promote adipocyte maturation. No minimum glucocorticoid dose or minimum period of usage has been determined for disease onset, and time to symptom onset ranges from several months to many years after initiation of steroid therapy. Patients typically present with gradually worsening low back pain, radiculopathy, and even cauda equina symptoms. Epidural lipomatosis displays fat signal characteristics on all MRI sequences and can be confirmed by fat suppression techniques (Fig. 46.2).
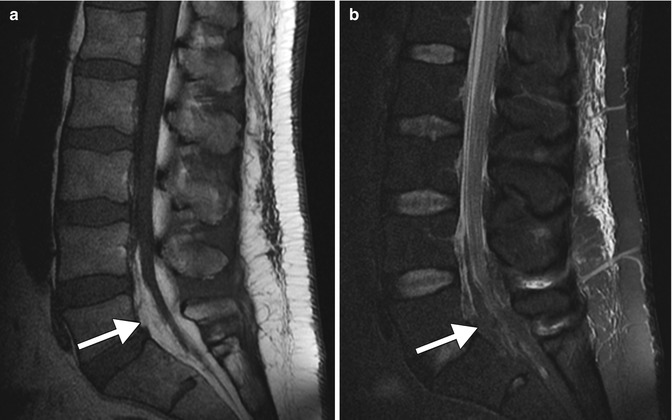
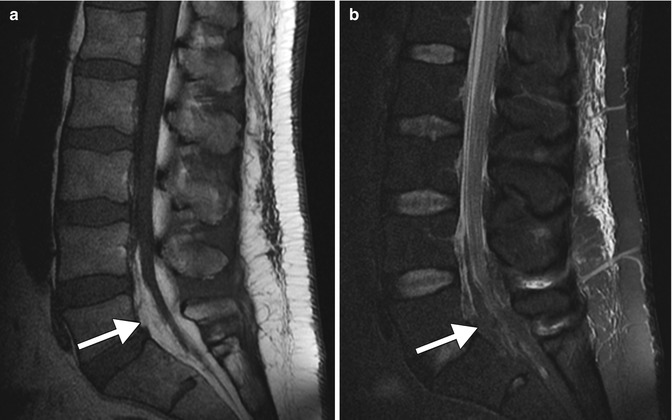
Fig. 46.2
Steroid-induced epidural lipomatosis. Sagittal T1 MRI (a) shows prominent T1 hyperintensity in the lumbosacral epidural space (arrow). The corresponding sagittal STIR MRI (b) shows suppression of signal in the epidural space, consistent with fat (arrow)
Dorsocervical Fat. Dorsocervical fat (buffalo hump) is a lipodystrophy that represents a manifestation of the cushingoid features associated with chronic glucocorticoid use. The fat has a propensity to accumulate in the posterior lower neck and upper back and is continuous with the adjacent subcutaneous fat. On CT, this process is readily recognized by fat attenuation and on MRI by the fat signal characteristics on all sequences (Fig. 46.3). The appearance of iatrogenic dorsocervical fat is identical to a buffalo hump that results from endogenous Cushing’s syndrome.


Fig. 46.3
Dorsocervical fat. Sagittal T1 MRI shows disproportionate increased thickness of subcutaneous fat in the posterior lower neck and upper back (arrow)
Osteoporosis and Insufficiency Fractures. Glucocorticoids directly inhibit bone formation and promote bone resorption. Glucocorticoids also decrease calcium absorption from the intestine and increase renal excretion. Osteoporosis occurs in at least 50 % of persons who require long-term glucocorticoid therapy. Glucocorticoids inhibit osteoblast function, preventing the formation of new bone in normal bone turnover. Osteoporosis can be diagnosed by DEXA scan or by relative subjective visual assessment of radiographs or CT. Insufficiency fracture should be suspected in an osteoporotic individual who presents with severe focal pain. MRI provides more sensitive and early diagnosis, in which the edema associated with acute fractures appears as hyperintensity on T2 and STIR sequences (Fig. 46.4).
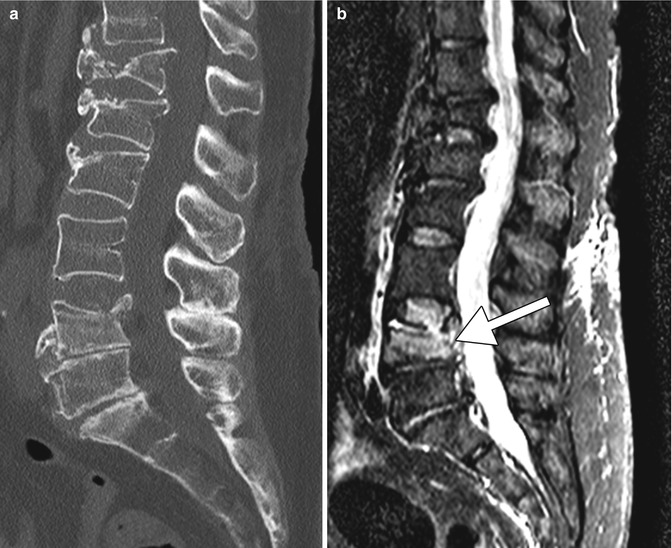
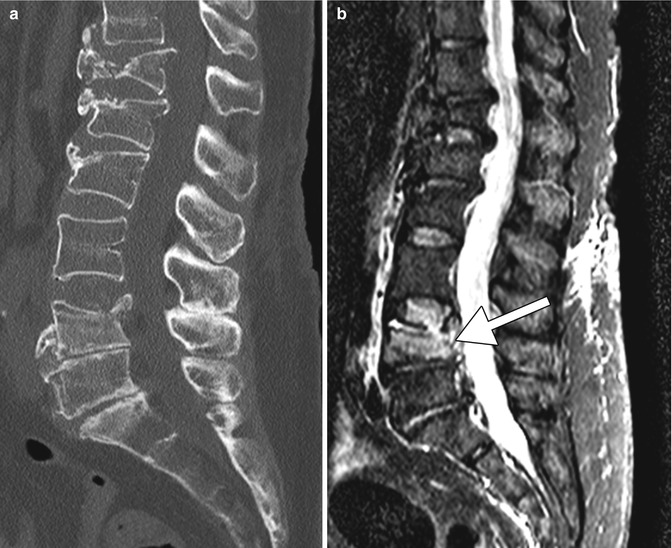
Fig. 46.4
Steroid-induced osteopenia and compression fractures. Sagittal CT (a) shows diffuse osteopenia and multiple compression fractures. The corresponding sagittal STIR MRI (b) shows edema in the L4 vertebral body (arrow), indicating an acute fracture, while the other compression fractures are chronic
Steroid-Associated Infections. Patients receiving chronic steroids have an increased susceptibility to many different types of infections. The risk of infection is related to the dose of steroid and the duration of therapy. Although pyogenic bacteria are the most common pathogens, chronic steroid use increases the risk of infection with intracellular pathogens such as Listeria, various fungi, herpes viruses, and certain parasites. On MRI, CNS pyogenic abscesses typically appear as ring enhancing lesions with restricted diffusion centrally. On the other hand, atypical infections can form abscesses without associated central diffusion restriction (Fig. 46.5).
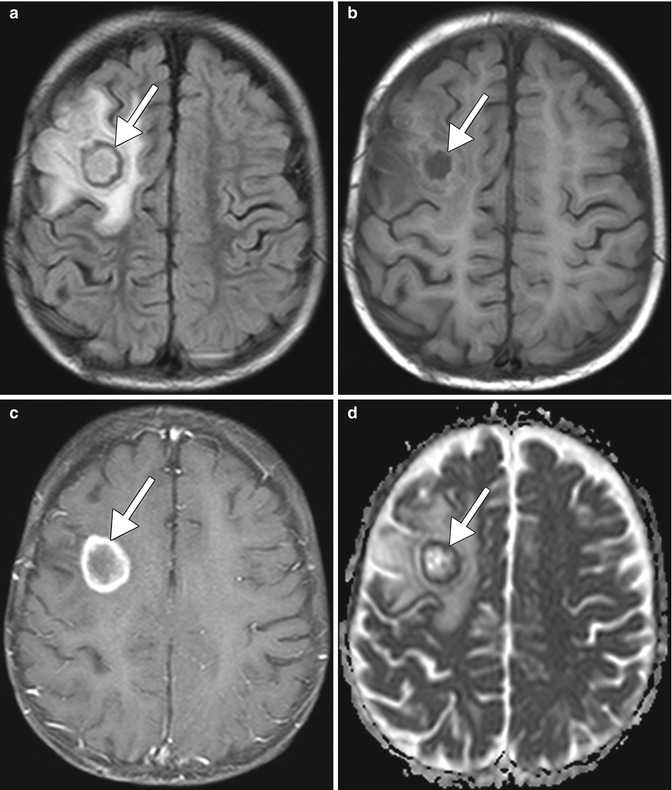
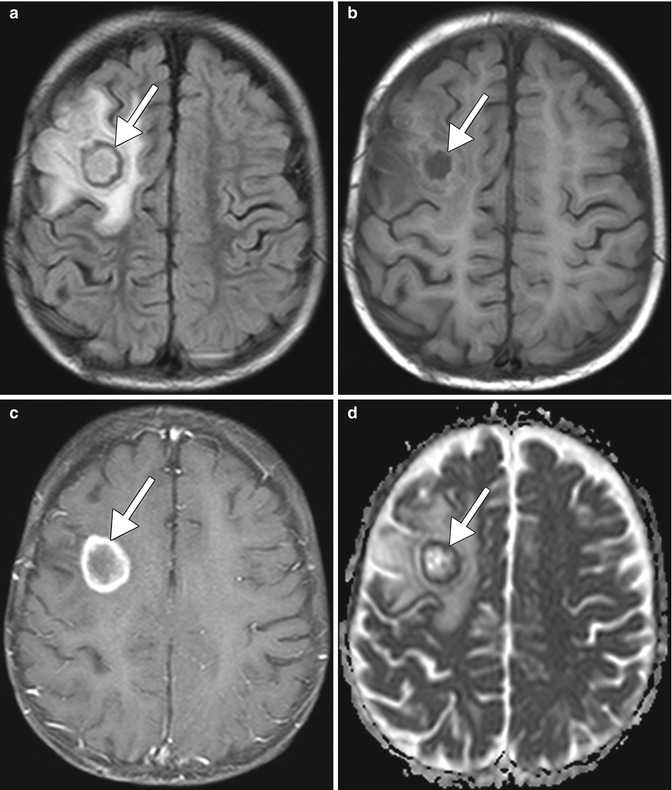
Fig. 46.5




Steroid-associated infection. This transplant recipient was on steroid therapy for immunosuppression and developed a Nocardia brain abscess. Axial FLAIR (a), T1-weighted (b), post-contrast T1-weighted (c), and ADC map (d) show a ring enhancing lesion with surrounding edema, but no restricted diffusion of the contents, in the right frontal lobe (arrows)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








