T1 Hyperintense Suprasellar Mass
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Pituitary Macroadenoma
Craniopharyngioma
Less Common
Saccular Aneurysm (Thrombosed)
Rathke Cleft Cyst
Ectopic Neurohypophysis
Lipoma
Dermoid Cyst
Rare but Important
Pituitary Apoplexy
Pilomyxoid Astrocytoma
Cavernous Malformation
Meningioma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Most common cause for ↑ T1 is subacute hemorrhage
T2* (GRE or SWI) useful
Age helpful in common diagnoses
Children = craniopharyngioma
Adults = pituitary macroadenoma, thrombosed aneurysm
Helpful Clues for Common Diagnoses
Pituitary Macroadenoma
Hemorrhage, sometimes cystic change
Craniopharyngioma
90% Ca++, 90% cystic, 90% enhance
“Crankcase” oily content → T1 hyperintensity
Helpful Clues for Less Common Diagnoses
Saccular Aneurysm (Thrombosed)
Usually eccentrically located, not directly suprasellar
Subacute/chronic mural thrombus
Rathke Cleft Cyst
May have very short T1 if high protein content or hemorrhage from cyst apoplexy
Look for intracystic nodule
Look for “claw” of enhancing pituitary gland wrapped around cyst
Ectopic Neurohypophysis
Pituitary stalk tiny or nonexistent
“Bright spot” on hypothalamus
Does not saturate with fat suppression
Lipoma
Suppresses with fat saturation
Dermoid Cyst
Fat droplets in sulci, cisterns (ruptured)
Helpful Clues for Rare Diagnoses
Pituitary Apoplexy
Subacute hemorrhage has short T1
Rim enhancement typical
Pilomyxoid Astrocytoma
May hemorrhage
Cavernous Malformation
“Popcorn” appearance
Meningioma
↓ T1 (psammomatous Ca++; hemorrhage, lipomatous transformation rare)
Image Gallery
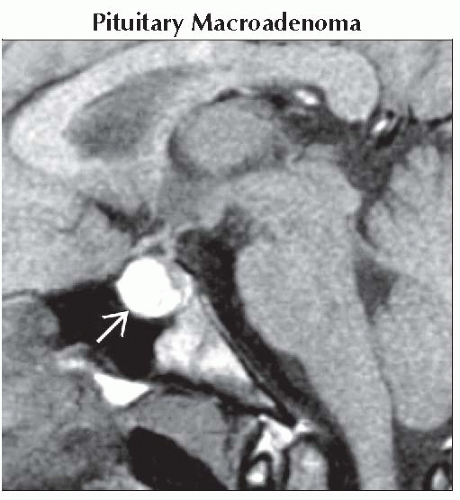 Sagittal T1WI MR shows a hemorrhagic intra- and suprasellar mass
 in a patient who presented with pituitary apoplexy. The diagnosis was macroadenoma with subacute hemorrhage. in a patient who presented with pituitary apoplexy. The diagnosis was macroadenoma with subacute hemorrhage.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|