Clinical Presentation
Normally the head is centered over the pelvis in both the sagittal and coronal planes. Clinical examination of the cervical deformity patient should include a visual assessment of global spinal alignment (▶ Fig. 9.1). This analysis of clinical global balance and assessment of deformity location can prove invaluable in selecting the correct spinal levels for surgery. This has been emphasized by Riew 1 who reported that persistence of an imbalance after correction can lead to failure.
Cervical malalignment can be evaluated clinically through assessment of the chin–sternum distance and chin–brow vertical angle (CBVA), which quantifies horizontal gaze. Clinical assessment of the anterior or posterior projection of the head can be correlated with the tilt angle (measured on lateral radiographs). Vital et al 2 defined this projection as “protraction or retraction.”
Flexibility of the cervical deformity can be invaluable for surgical planning. In the standing position, the patient is examined with passive and active extension to assess the extent to which cervical kyphosis can be corrected. In the supine position, the distance between the examination table and the occiput is measured; however, some flexibility may exist above and below the deformity. Koller 3 has described three types of “flexibility” (▶ Fig. 9.2). Clinical examination can be correlated with radiographic measurements of the C2–C7 Cobb angle changes on lateral flexion and extension views. In fused or rigid deformity, there is minimal or no change (<2 degrees). Semirigid deformities have partial correction, while flexible deformities have correction to cervical lordosis.
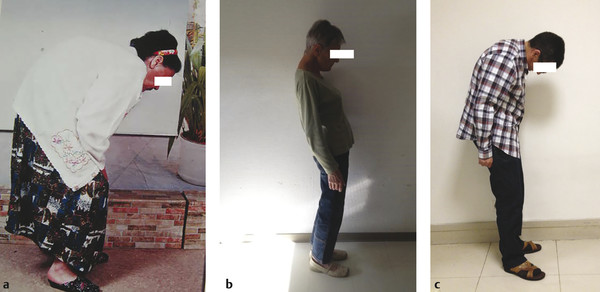
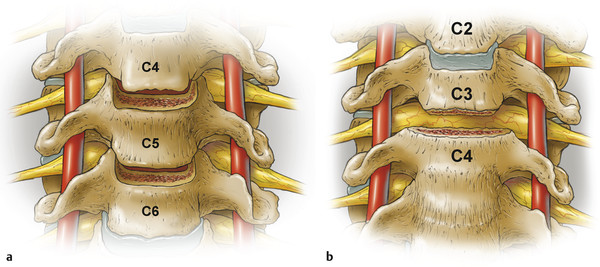
Fig. 9.1 Example of cervical deformities associated with different types of global balance.
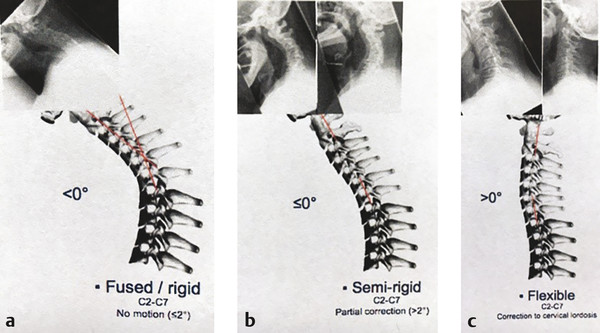
Fig. 9.2 The “three types of cervical flexibility.”
Overall mobility of the cervical spine is linked to segmental motion across each of the disc spaces and the facets. Pathological processes may induce stiffness. In ankylosing spondylitis, all elements (anterior and posterior) are fused, and the deformity tends to be rigid. In drop head, discs and posterior facets often remain mobile, and these deformities are typically flexible. In semirigid deformities, the disc spaces and uncinates and/or posterior facets may be partially fused, and some correction may be possible in extension.
A thorough neurological examination is also important. This should include an assessment for sensory changes, motor examination in upper and lower extremities, as well as an assessment for evidence of myelopathy.
9.3 Imaging
Full-length standing spine radiographs, including anteroposterior (AP) and lateral views, are necessary to measure the global alignment. AP and lateral cervical incidence can be used to determine the extent of kyphosis and vertebral levels involved and permit measurement of important radiographic parameters, including C2–C7 lordosis, C2–C7 sagittal vertical axis, thoracic kyphosis, lumbar lordosis, pelvic incidence, and pelvic tilt.
Lateral radiographs in maximum flexion and extension can be used to determine rigidity and residual flexibility of the spine above and below the deformity. These radiographs can also be helpful in localizing the area to be treated; EOS imaging, which minimizes radiation exposure and allows a full-body view, can be particularly useful for global deformity assessment. Magnetic resonance imaging (MRI) should be obtained if possible for the assessment of spinal cord and nerve root compression. Alternatively, a CT myelogram can provide similar information if MRI cannot be obtained. CT imaging is important for surgical planning, particularly to analyze whether disc spaces are open (i.e., not fused), presence of osteophytes, and evidence of ossification of the posterior longitudinal ligament. CT is also useful in assessing fusion of the uncus and facets.
The vertebral arteries (VA) can have aberrant anatomy or pathways and may have areas of adhesions, particularly in cases of inflammatory diseases (e.g., rheumatoid arthritis or infection) or in the setting of previous surgery. Surgeons should maintain a low threshold for obtaining angiography (e.g., CT angiogram) to characterize the anatomy and pathways of the VAs, as well as to assess the patency and for evidence of dominant anatomy.
Otolaryngologist’s evaluation is indicated particularly if the patient is planned for an anterior cervical approach and especially if the patient has had previous anterior surgery. In the series of Lee and colleagues, 4 previous anterior surgery or multilevel fusions had increased risk for dysphagia and dysphonia. If vocal cord function is normal bilaterally, then a left or right anterior approach can be considered. In the case of previous surgery, some surgeons prefer to avoid scar tissue. However, in the presence of vocal cord paralysis, the approach must be through the scar to avoid injury to the contralateral vocal cord.
9.4 Preoperative Planning
The decision of whether to pursue surgical treatment should include consideration of response to nonsurgical treatments, deformity progression, clinical symptoms, quality-of-life consequences, and patient’s preferences. The presence of myelopathy should favor surgical treatment, especially in cases in which it is severe or demonstrates significant progression. The surgery plan requires localization of the levels of deformity and its extent, measurement of the degree of deformity and prediction of the amount of correction needed, and assessment of the rigidity of the deformity, including the surrounding flexibility of the cervical segments above and below. The plan should also account for the potential need to address neurological compromise, including that resulting from direct compression, instability, or from spinal stretch over kyphotic segments.
9.5 Surgical Technique
Semirigid deformity can be corrected by either anterior or posterior osteotomies. The anterior approach is the preferred technique if preoperative assessment demonstrates isolated anterior fusion. Multilevel anterior cervical discectomy and fusion (ACDF) or corporectomy may ultimately be performed; however, here we will follow, step by step, the uncovertebral joint osteotomy, defined as an osteotomy through the uncovertebral joints and extending next to the transverse foramen bilaterally, as well described by Tan and Riew. 5
Cervical osteotomy techniques have been described and classified by Ames and colleagues. 6 Their classification of osteotomies and soft-tissue releases includes seven anatomical grades of resection that represent progressively greater degrees of bony removal and potential destabilization. Since the surgical procedure for a given case may involve combinations of resection types, the highest grade of osteotomy is designated as the “major osteotomy,” while lower grades of osteotomy are designated as “minor osteotomies.” In this classification, complete resection of the uncovertebral joints is classified as a Grade 4 osteotomy (▶ Fig. 9.3).
Prior to surgery, the patient can be placed in halo-traction at bedside with the addition of muscle relaxants, in order to try to reduce the deformity. Lateral radiographs can demonstrate the amount of reduction obtained. We more frequently use a halo than Gardner-Wells tongs, since this technique allows us to manipulate the head more easily during surgery. Surgery is done under general anesthesia. Depending on the deformity, sometime intubation orally is impossible, and can only be done through nasal passage (▶ Fig. 9.4). The patient is placed in a supine position, but in the setting of rigid kyphosis the head may not rest on the table and may require pillows for support.
Under anesthesia, we measure the distance between the occipital protuberance and the table, as well as the chin–sternum distance, and assess spinal alignment with lateral views under fluoroscopy. Sometimes partial reduction of the deformity is obtained, when the patient relaxes under general anesthesia. Cervical traction is applied (2–3 kg) through the halo, and arterial pressure is maintained around 80 mm Hg (particularly in the case of spinal cord compression). The neck is prepared and draped in the usual sterile fashion, and a Smith–Robinson approach is used, for which we prefer a vertical incision for deformity correction. A right or left approach may be used depending on the deformity, history of previous surgery, vocal cord function, and surgeon’s preference. In the case of a coronal deformity (scoliosis), we prefer to approach on the convex side, allowing for more space and easier correction.
An anterior approach for significant cervical can be challenging and demanding. Application of traction during surgery and even for several days prior to surgery for semirigid curves can help partially reduce the deformity and provide improved operating access. In this chapter, we discuss osteotomies for two situations, semirigid and rigid deformities of the subaxial cervical spine generally based on the technique of Tan and Riew. 5
The anterior cervical spine is exposed, and the longus colli muscles are detached and retracted bilaterally. This dissection may create bleeding, for which we use cautery and surgical wax. A major step is to localize the uncinate, which can be achieved through blunt dissection close to the bone, using a 2- or 4-mm spatula, lateral to the uncinate. The costal process (anterior ring of the foramen transversarium) is used as a landmark to identify the fused disc space, since the disc space and uncinate are just medial to the cranial border of the costal process (▶ Fig. 9.5).
The spatula remains in place during resection, identifying the lateral border of the uncinate, protecting the VA, and guiding the lateral bony resection. In case of concern regarding VA anomalies and in difficult case, we use the VA dissection technique of George. 7, 8 Gradually, the anterior ring of the foramen transversarium is fully exposed, then by a blunt dissection close to the bone, the foramen is penetrated above and below the ring. Using a small Kerrisson punch, we resect the anterior ring. The VA is identified and can be safely excluded from the resection area (▶ Fig. 9.6). The VA can be surrounded by a venous complex, which can be addressed with bipolar cautery to avoid bleeding.
At this point, the fused uncinates are exposed and the VAs are excluded. Next, we do not use Caspar pins, as described by Riew, as we find that they overload the operative field due to their convergence, and they tend to impede the passage of the surgeon’s hands when releasing the opposite side. Furthermore, Riew used these pins for deformity correction, which we consider potentially risky, particularly in older and osteoporotic patients. In contrast, we implant very laterally, perpendicular to the vertebral body, two 15/10 pins, which increase retraction of the muscles and soft tissue (▶ Fig. 9.7). These pins make an angle which we measure at the beginning of the osteotomy, and the new angle after the osteotomy provides an estimate of the amount of expected correction achieved. Discectomy is then completed down to the longitudinal ligament, after which the uncinates are totally exposed medially and laterally (▶ Fig. 9.8).
The osteotomy is then initiated with a high-speed surgical drill (▶ Fig. 9.9). In the case of a purely kyphotic deformity, bony resection must be absolutely perpendicular to the cervical spine and in the same space as the disc. Any asymmetric resection can induce iatrogenic coronal deformity. Conversely, the resection should be asymmetric, in the case of a mixed coronal and kyphotic deformity. Bony resection is performed down to the posterior longitudinal ligament. Dural lesion must be avoided during this stage.
Resection of the uncus is initially partial. If the uncinates are not totally fused, total resection is not necessary. If the uncinates are fused, an attempt can be made using a Cobb elevator which may be rotated in the disc space, close to the residual uncinate, to produce some “breakage,” in order to avoid the need for total resection of the uncinate. The same maneuver can also be done with a vertebral body spreader.
If “mobility” is not obtained, total uncinate resection must be achieved. Importantly, the burr never passes the lateral border of the uncinate. When there remains only a very thin shell of bone, the residual bone can be removed by a very small Kerrisson or curette. Since correction of local kyphosis, by opening the anterior disc space, may induce stenosis of the foramen, a foraminotomy is recommended to avoid root entrapment.
Once both sides are sufficiently released or totally resected, correction of the kyphosis can be realized. The pillows under the head are removed, and the surgeon applies controlled pressure on the anterior ring of the halo. A Cobb retractor and spreader can help at the same time by opening and distracting the disc space (▶ Fig. 9.10). We do not like to use the two Caspar pins as a means of correction, since the force applied is not biomechanically satisfying, and in old patients these may risk vertebral body fracture. The new angle of the pins will reflect the local amount of correction. If the posterior facet joints are not fused and have residual mobility, this will allow easier correction. Even if the facet joints are partially fused, correction can be obtained, thanks to the anterior long lever arm.
At this stage, the risk is not overcorrection (the rest of the spine is flexible) but rather hypocorrection. It is necessary to try to assess the new sagittal alignment. The head must now touch the operative table, and the chin–sternum distance must return to a normal value. Radiographs are done to measure the new Cobb angle. Lordosis is stabilized by increasing the halo traction weight to 9 kg.
If the osteotomies have been realized at multiple levels, large cages can be used. If all corrections have been achieved at a single level, leaving a big gap, we prefer to use iliac crest bone graft, which will be easier to shape and to better adapt to the space. It is important to provide the largest surface area between the graft and the endplate support to avoid pseudarthrosis and subsidence. An anterior plate, bent in lordosis, is applied. Screws are implanted at the upper and lower part of the construct. In old patients with osteoporotic bone, we add a posterior fusion and fixation to help ensure postoperative stability.
If correction is inadequate, the facets are fused, the spine is already fixed posteriorly, or there is a posterior mass of fusion, a second-stage surgery may be necessary to increase correction. In this case, only graft material is placed in the anterior part of the osteotomy in order to leave freedom when additional lordosis is created from the posterior approach. A buttress plate is fixed with only screws above or below just to avoid graft extrusion. Additional lordosis from the posterior approach will induce compression on the posterior part of the anterior graft permitting fusion. Posterior osteotomies can be achieved as described by Ames et al 6 at one or multiple levels with fixation and fusion.
Closure is done with drainage. Theoretically, no external immobilization is needed. Early mobilization and physical therapy are recommended (▶ Fig. 9.11)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree