♦ Preoperative
Operative Planning
- Review imaging (computed tomography, magnetic resonance imaging, angiogram)
- Epilepsy surgery (see Chapter 57, Temporal Lobectomy and Selective Amygdalohippocampectomy)
- Tumor (see Chapter 44, Temporal Glioma)
- Vascular malformation (see Chapter 28, Surgical Treatment of Cortical Arteriovenous Malformations); cavernous malformation (see Chapter 31, Supratentorial Cavernous Malformations)
- Biopsy
- Extradural hemorrhage (EDH; see Chapter 66, Epidural Hematoma Evacuation)
Equipment
- Major set-up unless biopsy or EDH
- High-speed drill
- Operating microscope (not necessary for biopsy or EDH)
- Leyla bar
- Greenberg retractors (not necessary for biopsy or EDH)
- Device for wrist support (not necessary for biopsy or EDH)
Operating Room Set-up
- Always position head to same side of room
- Anesthesiologist to left, scrub nurse to right
- Viewer scope to the right
Anesthetic Issues
- Room should be cool for mild hypothermia
- Intravenous (IV) antibiotics with skin flora coverage (cefazolin 2 g) should be given 30 minutes prior to incision
- Dexamethasone 10 mg IV prior to incision
- Mannitol (0.5 to 1 mg/kg) for brain relaxation/protection; given prior to turning bone flap to avoid tearing dura
- Fosphenytoin load 1 g IV (or levetiracetam IV, if available) if patient is not on anticonvulsants
- If epilepsy case, just continue prior anticonvulsants
- Not necessary for biopsy
- Should discontinue after 1 week in trauma (and possibly tumor) cases with no seizures
- Degree of intracranial pressure (ICP) elevation should be communicated to anesthesiologist
- Rapid intubation for EDH, or high ICP
- Mannitol (0.5 to 1 mg/kg) for brain relaxation/protection; given prior to turning bone flap to avoid tearing dura
♦ Intraoperative
Positioning
- Foley catheter
- Spinal drain placed if extra brain relaxation desired (usually unnecessary)
- Roll or 5-lb weight under ipsilateral shoulder
- Mayfield head holder (unless biopsy or EDH); two pins on occiput, one frontally, just above widow’s peak
- Head turned 90 degrees to opposite side, parallel to floor (assess neck flexibility before surgery); 60 degrees to opposite side for medial temporal resection surgery to see down the length of hippocampus
- Slight neck extension; malar eminence should be highest point
- Eyes taped closed
Minimal Shave
- Use disposable razor
- Leave 1-cm margin beyond skin incision
Sterile Scrub and Prep
- Betadine detergent scrub and sterile gloves for 5 minutes
- Wipe with alcohol swab
- Paint with Betadine
- Gown and glove
- Pat Betadine dry
- Four blue towels, Steri-Drape (3M), and drape
Mark Incisions
- Question mark (right) or reverse question mark (left)
- Started at zygoma, 1 cm in front of tragus
- Curved posteriorly hugging superior aspect of pinna (closer to floor of middle fossa)
- Posterior margin behind pinna, then curved anteriorly
- Started at zygoma, 1 cm in front of tragus
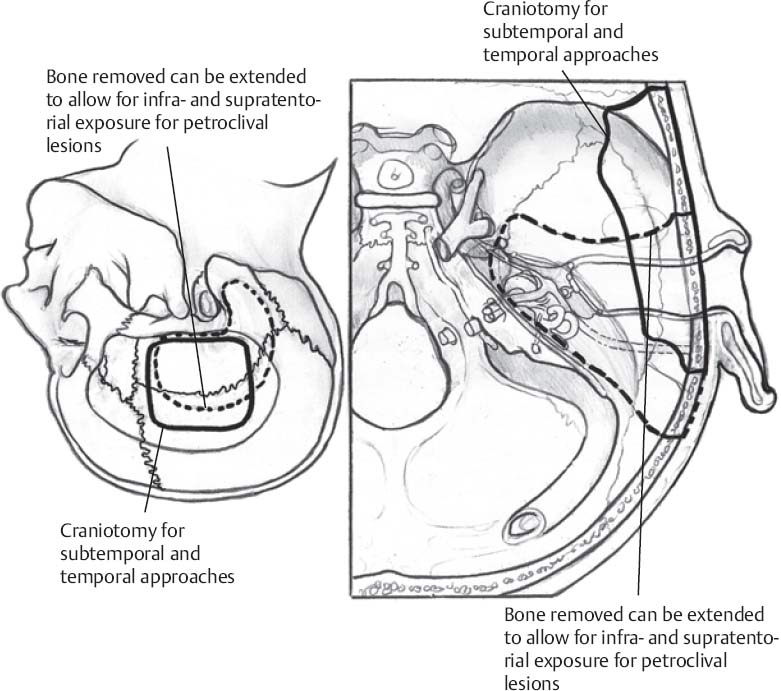
- Anterior extent of incision to limit of hairline just below insertion of temporalis; or, if limited hair this region, extended above widow’s peak (Fig. 12.1)
- Linear incision (for biopsy, EDH, or selective amygdalohippocampectomy)
- Start at zygoma, 1 cm in front of tragus
- Extend superiorly ~6 cm to superior temporal line
- Linear incision (for biopsy, EDH, or selective amygdalohippocampectomy)
Scalp and Muscle Incision
- Scalp only
- Major bleeders cauterized with bipolar
- Raney clips applied unless linear incision, since self retaining retractors will stop bleeding
- Weck clips (Teleflex Medical, Research Triangle Park, NC) on superficial temporal artery prior to cutting it with knife
- Major bleeders cauterized with bipolar
- Temporalis fascia incised with knife and extended with Metzenbaum scissors; if question mark, muscle incised at limits of skin incision to maximize exposure but cuff left for closure
- Muscle incised with monopolar or no. 10 blade
Only gold members can continue reading. Log In or Register to continue








