The ABCs of Neurologic Emergencies
James D. Fleck
José Biller
This chapter is designed to be a very brief reference for common neurologic emergencies. In general, we presume an accurate diagnosis has been made and mainly concentrate on acute therapy. Although not comprehensive, this guide should allow you to care for a patient with the following problems for the first few hours.
I. ELEVATED INTRACRANIAL PRESSURE
A. Thirty degrees head-up neutral position.
B. Correction of factors exacerbating intracranial pressure (ICP).
1. Hypercarbia.
2. Hypoxia.
3. Hyperthermia.
4. Acidemia.
5. Hypotension.
6. Hypervolemia.
C. Avoid hypotonic solutions.
D. If ICP monitor has been placed, maintain cerebral perfusion pressure at 70 mm Hg.
E. Goal is euvolemia with elevation of osmolality.
F. Mannitol (20% solution) 1.0 g per kg intravenous (IV) as a bolus followed by 0.25 to 0.5 g per kg every 4 to 6 hours, depending on clinical status, serum osmolality (target 310 to 320 mOsm per kg), volume status, and ICP measurements.
G. Consider hypertonic saline 3% solution or 23.4% solution (0.5 to 2.0 cc per kg) through a central line in therapy-resistant elevation of ICP (target serum sodium of 145 to 155 mEq per L).
H. Dexamethasone (if vasogenic edema).
I. Hyperventilation to PaCO2 of 30 to 35 mm Hg (temporizing measure).
1. Typically, it loses effectiveness in 24 to 48 hours.
2. Four percent change in cerebral blood flow for every 1 mm Hg change in PaCO2.
J. Sedation and paralysis if necessary.
K. CSF drainage if necessary.
L. Barbiturates.
M. Hypothermia.
N. Surgical decompression (see Chapter 36).
II. COMA
A. Thorough general and neurologic examination.
B. ABCs: airway, breathing, and circulation.
C. IV fluids: normal saline.
D. Manage hypoglycemia with 50 ml of 50% glucose IV. Consider thiamine 100 mg IV before glucose.
E. Consider naloxone 0.4 to 2.0 mg IV for opioid overdose.
F. Consider flumazenil 0.2 mg IV for benzodiazepine overdose.
G. Arterial blood gases, glucose, electrolytes, calcium, magnesium, phosphorus, blood urea nitrogen, creatinine, liver enzymes, ammonia, CBC, urinalysis, blood and urine toxicology screens, and TSH.
H. If focal neurologic signs, or history of head trauma, consider therapy for elevated ICP with hyperventilation and osmotherapy.
I. Emergency brain imaging: typically unenhanced head CT.
J. Consider lumbar puncture (LP) if suspected CNS infection or suspected subarachnoid hemorrhage (SAH) with normal findings on head CT. K. EEG.
III. STATUS EPILEPTICUS (GENERALIZED TONIC-CLONIC STATUS EPILEPTICUS)
A. ABCs: airway, breathing, and circulation.
B. IV line with normal saline.
C. Reduce temperatures >39°C with cooling blankets.
D. Consider 100 mg thiamine IV.
E. Consider 50 ml of 50% glucose IV.
F. Lorazepam 0.1 mg per kg IV at 2 mg per minute, maximum of 8 mg in adults or diazepam 0.2 mg per kg IV at 5 mg per minute up to a total dose of 20 mg.
G. Phenytoin 20 mg per kg IV (at <150 mg per minute in adults) or fosphenytoin 20 mg per kg IV (up to 150 mg phenytoin equivalent per minute).
H. If seizures continue, give additional bolus of phenytoin 10 mg per kg or fosphenytoin 10 mg per kg (to a maximum of 30 mg per kg).
I. Intubation, airway protection, and possibly ventilatory support.
J. If seizures persist, administer one of the following IV:
1. Midazolam (Load 0.2 mg per kg; repeat 0.2 to 0.4 mg per kg boluses every 5 minutes until seizure stops. Maximum loading dose 2 mg per kg.)
2. Propofol (Load 1 mg per kg; repeat 1 to 2 mg per kg boluses every 3 to 5 minute until seizures stop. Maximum loading dose 10 mg per kg.)
3. Valproate (Load 40 mg per kg over 10 minute. If seizures persist, 20 mg per kg over 5 minute.)
4. Phenobarbital (load 20 mg per kg, at 50 to 100 mg per minute).
K. If seizures still continue, use IV pentobarbital.
1. Loading with 5 to 10 mg per kg IV. Rate 50 mg per minute. Maintenance 1 to 3 mg/kg/hour.
2. Goal is burst-suppression pattern on EEG.
L. Management of intercurrent medical complications.
IV. BACTERIAL MENINGITIS
A. Treat within 30 minutes of arrival for medical care.
B. Manage elevated ICP.
C. Control seizures.
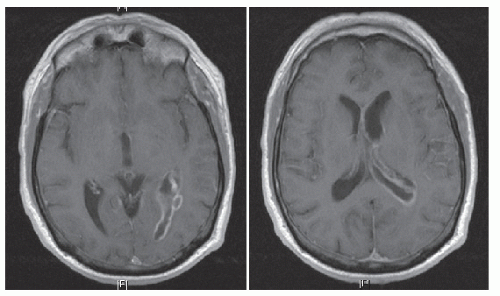
D. Manage complications (subdural empyema, brain abscess, ventriculitis, acute hydrocephalus, vasculitis, vascular spasm, venous thrombosis, and hyponatremia due to SIADH) (Fig. 58.1).
E. No universally accepted standard for duration of treatment.
F. Empiric antibiotic treatment of immunocompetent patients with community-acquired meningitis: ceftriaxone or cefotaxime plus vancomycin plus dexamethasone 0.15 mg per kg IV every 6 hours for 4 days (American Academy of Pediatrics recommendation for infants and children—first dose to be given before or within 4 hours of antibiotic). See Table 58.1 for antibiotic doses.
G. Consider ceftazidime if Pseudomonas infection is suspected.
H. Consider ampicillin if Listeria infection is suspected, as in an immunocompromised host.
I. Consider doxycycline if Rickettsia, Anaplasma, Ehrlichia, or Coxiella burnetii is suspected.
J. Chemoprophylaxis of meningococcal and Haemophilus influenzae infection with rifampin.
V. HERPES SIMPLEX ENCEPHALITIS
A. Fluid and ICP management.
B. Seizure control.
TABLE 58.1 Antibiotic Therapy for Bacterial Meningitis | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||
C. Acyclovir IV 10 mg per kg every 8 hours for 14 to 21 days; adjust dose to patient’s renal function.
D. Untreated has a mortality rate of 70%.
VI. BRAIN ABSCESS
A. If there is no clear etiologic factor, administer ceftriaxone (Table 58.1) plus vancomycin (Table 58.1) plus metronidazole 500 mg every 6 hours in adults and 7.5 mg per kg every 8 hours in children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree