Chapter 9 The Chiari Malformations and Syringohydromyelia
• Chiari malformations are pathological herniations of the hindbrain through the foramen magnum and into the cervical spinal canal. Chiari malformations are being recognized with increasing frequency because of the increased availability of magnetic resonance imaging (MRI).
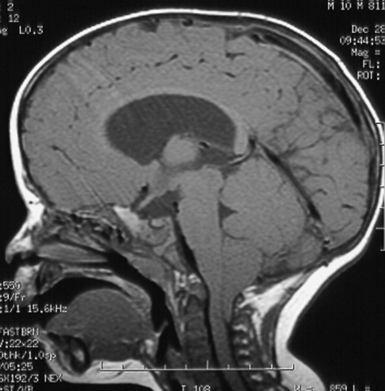
• Chiari I malformation (CIM) represents downward herniation of the cerebellar tonsils into the cervical canal at least 3 to 5 mm on sagittal MRI. The impaction of the tonsils in the foramen magnum causes an anatomical and physiological block of cerebrospinal fluid (CSF), which normally flows from the posterior fossa into the cervical subarachnoid space. The symptoms of CIM commonly include headache or neck pain worsened by activity or Valsalva maneuver, or signs of brainstem compression. Syringomyelia may be associated with CIM, and those patients often present with signs of spinal cord dysfunction.
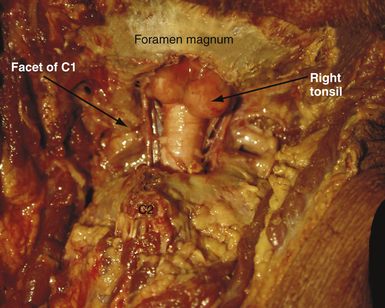
• The most widely accepted treatment of CIM is a posterior fossa decompression with removal of the posterior arch of C1 and dural augmentation graft. The goal of surgery is to enlarge the posterior fossa and permit normal flow of CSF from the posterior fossa to the cervical subarachnoid space. In the majority of patients, the symptoms of headache resolve and there is a concomitant collapse of the associated syrinx. Only rarely does the surgeon have to treat directly the associated syringomyelia.
• Chiari II malformation (CIIM), which is a downward migration of the cerebellar vermis and brainstem through the foramen magnum, is most commonly seen in patients with myelomeningocele. It is associated with hydrocephalus in 90% of the patients. Syringomyelia is also very common. In addition, on MRI, patients often have low-lying tentorium, tectal beaking, cervicomedullary kinks, agenesis of the corpus callosum, and other brain abnormalities. A small, but significant, number of patients will present with acute brainstem, cerebellar, or progressive spinal cord dysfunction. The initial step in this treatment should be the surgical establishment of a functioning shunt. If the symptoms progress or do not resolve in this setting, then a formal decompressive procedure may be required.
• Syringomyelia, or cavitation of the spinal cord, has many causes in addition to hindbrain herniation. Signs and symptoms of a syrinx include pain and temperature loss, reflex changes, or motor weakness. Treatment of the syrinx, when not the result of hindbrain herniation, often includes shunting of the syrinx into the peritoneum or pleura. The goal is to drain the syrinx and to reestablish a patent subarachnoid space.
In the early 1890s, the pathologist Hans Chiari1 described four congenital malformations that would later become known as the Chiari malformations. The four traditional varieties of Chiari malformations represent varying degrees of involvement of rhombencephalic derivatives. Three of these (types I to III) have progressively more severe herniation of these structures outside the posterior fossa as a common feature. These three also have in common a pathogenesis that involves a loss of free movement of cerebral spinal fluid (CSF) out of the normal outlet channels of the fourth ventricle. Pathological differences between Chiari I malformations (CIMs) and Chiari II malformations (CIIMs) can be explained with knowledge of the differences in the timing of the development of the hindbrain herniation.2
Chiari 0—These patients do not appear to have significant hindbrain hernias, although the posterior fossa may appear “crowded”; they have large syringes that resolve with posterior fossa decompression and have a unique position in our thinking about this subject.3,4 These malformations have been informally termed Chiari 0 because they behave as though they have fourth ventricular outlet obstruction, and at surgery they frequently do have physical barriers to CSF movement but do not have caudal displacement of the cerebellar tonsils beyond a point that could be considered pathological.
Chiari I—This common group of patients has been found to have caudal displacement of the cerebellar tonsils more than 5 mm below the foramen magnum. The brainstem is in a normal position and they may or may not have a syrinx. The 5 mm “rule” concerning the definition of pathological extent of caudal migration of the tonsils is arbitrary. Numerous patients have tonsils well below this point and are asymptomatic, especially young infants and children. When followed over time they frequently remain asymptomatic if their initial evaluation was performed for an unrelated reason. The extent of their caudal migration may progressively improve with time and become less impressive. This, however, is not assured and the patient should be followed for the development of symptoms. Syringomyelia is often associated with the CIM.
Chiari I.5—Although somewhat confusing, this term is applied to patients who bridge the gap between the CIM and CIIM. They have characteristics of both groups and are best considered separately. They are unassociated with neural tube defects and have caudal displacement of the cerebellar tonsils similar to that seen in the CIM patient. However, their brainstem and fourth ventricle are displaced inferiorly like CIIM patients. In our series of patients with a hindbrain hernia but without a neural tube defect, 17% had significant caudal displacement of the brainstem.5,6
Chiari II—This lesion almost always occurs in patients with neural tube defects (myelomeningoceles and encephaloceles). It consists of caudal migration of the cerebellar vermis, brainstem, and fourth ventricle. Syringomyelia is common in this group.
Chiari III—The Chiari III malformation is a rare and extreme form of hindbrain hernia that may be confused with an occipital encephalocele. It comprises less than 1% of all patients in this category. Patients have low occipital or high cervical sacs containing significant portions of the cerebellum and brainstem.7 Other intracranial anomalies such as are found with CIIM patients may be seen with this group. Hydrocephalus is common and severe neurological and developmental problems are almost always present.
Chiari IV—Type IV Chiari malformation patients have cerebellar hypoplasia or aplasia; this malformation is not a form of hindbrain hernia. For this reason, inclusion in a discussion of hindbrain hernias is debatable and will not be considered further.
Chiari I Malformation
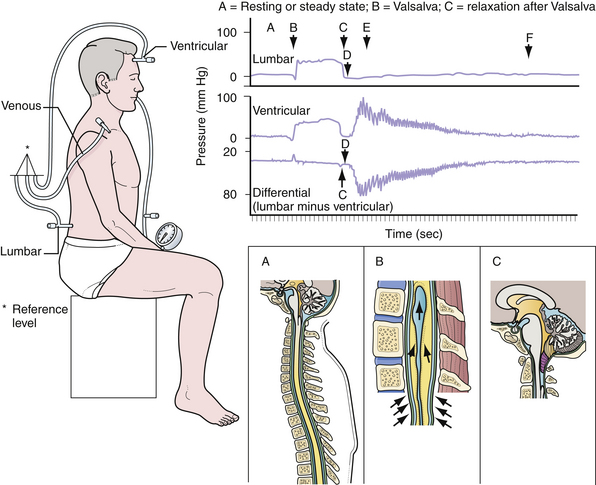
Many theories have been put forth to explain the development of Chiari malformations in the absence of hydrocephalus (Figs. 9.1 to 9.3). Currently, the most appealing theory emphasizes the difficulty in rapidly equilibrating the CSF pressure wave seen during the Valsalva maneuver.8–10 During this delay in achieving equilibrium, there is a vector of force out of the intracranial cavity (Fig. 9.4). The prolonged intracranial hypertension relative to the intraspinal compartment may result in the downward migration of the cerebellar tonsils, resulting in obstruction of normal CSF flow between the posterior cranial fossa and the cervical subarachnoid space. Conditions that impede the physiological flow of CSF at the foramen of Magendie enhance the formation of the malformation. These could include arachnoid veils or septations in this region as well as adhesions.11 Alternatively, conditions that artificially lower the intraspinal pressure relative to the intracranial pressure (lumboperitoneal shunts) have been observed to “cause” the CIM with the subsequent development of syringomyelia. Parenthetically, there is some evidence that the CIM may result from derailment on chromosomes 9 and 15.12
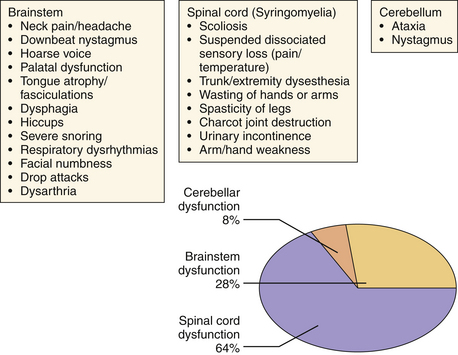
Initially considered an “adult” disease, the CIM is reported more frequently now in the pediatric population as a result of the widespread availability of detailed MRI. The clinical presentation of CIM essentially falls into three categories (Fig. 9.5):
1. Signs or symptoms related to brainstem compression
2. Signs or symptoms associated with cerebellar compression
Most commonly, patients present with occipital or cervical pain that is nonradicular but frequently associated with dysesthesias in the C2 dermatome.13 The neck pain or headache is frequently brought on by exertion or by coughing or sneezing (Valsalva-induced). Nonverbal children may relate their pain via irritability, crying, failure to thrive, or the presence of opisthotonos.
The diagnosis of CIM can easily be confirmed with MRI. The presence and extent of syringomyelia, seen in 50% to 75% of patients,5,14–16 should be determined with an MRI of the entire spinal cord. Computed tomography (CT) may further elucidate the bony abnormalities and plain films may assist in the evaluation of stability issues. Dynamic MRI (cine-MRI) has been used to evaluate CSF flow around the craniocervical junction. In a review of 800 MRI examinations, one study noted that “normal” or “asymptomatic” patients may have cerebellar tonsils that extend 3 mm below the foramen magnum.17 The tonsillar herniation was noted to be clearly pathological when it exceeded 5 mm. Similarly, Barkovich and associates18 studied 200 normal patients and 25 patients with a “firm” diagnosis of CIM. Tonsils 2 mm below the foramen magnum were considered as the lowest extent of the tonsils in normal patients (specificity of 98.5% [three false positive results] and a sensitivity of 100%). Tonsils 3 mm below the foramen magnum were considered the lowest extent in normal patients (sensitivity 96% and specificity 99.5%). An additional study has documented ascent of the tonsils with increasing age in some patients.19
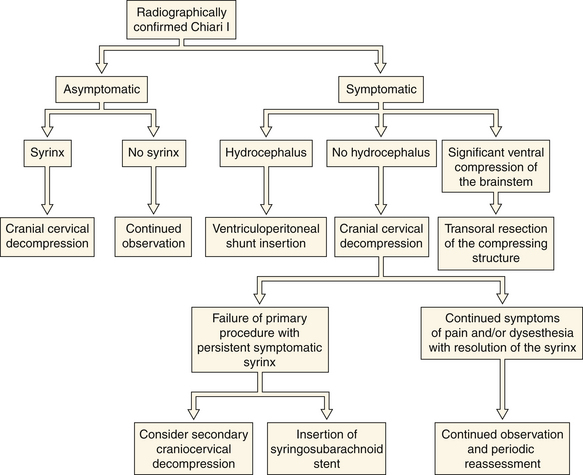
No medical treatment exists for the Chiari malformations. Numerous therapeutic paradigms exist (Fig. 9.6). The first decision that must be made is whether the lesion is truly symptomatic. Observation is warranted in asymptomatic patients without an associated syrinx. In symptomatic patients or asymptomatic patients with syringomyelia, surgical intervention is recommended. The degree of brainstem compression and tonsillar herniation is taken into account as well. In about 10% of patients hydrocephalus is associated with the CIM, in which case a CSF diversionary shunt or endoscopic third ventriculostomy should be the initial form of therapy. Similarly, symptomatic ventral compression out of proportion to dorsal compression may require a ventral decompression (i.e., transoral odontoid resection), especially in cases of myelopathy. The most common surgical procedure for the treatment of CIM is posterior fossa decompression. The goal of the operation is to enlarge the posterior fossa and to re-create the cisterna magna, thereby permitting normal flow of CSF from the posterior fossa to the cervical subarachnoid space. In the majority of CIM patients with a syrinx, the syrinx decreases in size and does not require direct treatment because the posterior fossa decompression treats the underlying pathological process causing the syringomyelia.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree