Chapter 4 The close environment
• altering the close environment influences
• either completely avoiding or at least changing the pattern of use, for example, posture (to a better rather than simply a different one)
• performance of activities to help counterbalance the negative effects of the behavior in question (stretching, toning, exercising, etc.).
In this chapter some of these important influences will be evaluated. Taken together with the information in Chapters 1, 2 and 3, a perspective should emerge that will encourage practitioners to use their own bodies more efficiently and less stressfully, as well as being able to advise and guide their recovering patients appropriately regarding the everyday influences of their close environments.
The bodyworker’s close environment
Acture guidelines for bodywork students and practitioners
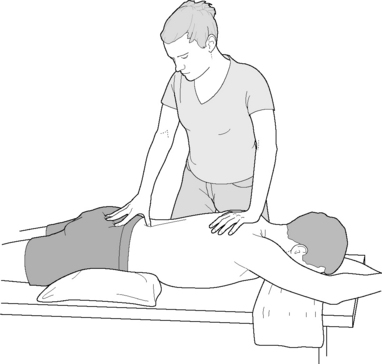
• Maintain a wide base of support. The feet should be separated with the potential for easy weight transfer from one foot to the other, allowing contact hand pressures to be increased or decreased as required by means of weight transfer rather than muscular effort (practice of tai chi encourages this type of movement). Balanced stance calls for careful positioning in relation to the treatment table and the patient, in order to be able to easily move the upper body and to transfer weight from one leg to another, without losing balance and without the need to readjust foot positioning. A wide base of support offers a chance for smooth movements without strain and creates a stable, centered stance which would not be easily perturbed by an unexpected need for alteration of position (Fig. 4.1).
• Maintain the spine in neutral as far as possible. This calls for flexion occurring (if possible) at the knees and hips and with the lumbar spine being required to produce only minimal flexion and extension movements during the application of treatment.
• Awareness of one’s own center of gravity, which lies just anterior to the second sacral segment (approximately 2 inches (5 cm) below the umbilicus and 2 inches (5 cm) deep), is important. Flexion of the knees and hips will encourage conscious movement of this center of gravity.
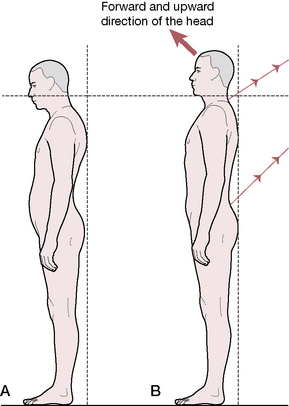
• The head and neck should be held in a ‘forward and upward’ mode, the typical Alexander technique model of posture in which there is a perpetual lengthening of the spine (from the head) rather than a slumping collapsed posture in which the weight of the head drags the upper body forward and down. During application of therapeutic measures any tendency for the upper cervical region to extend should be resisted, a particularly difficult habit for many to break (Fig. 4.2).
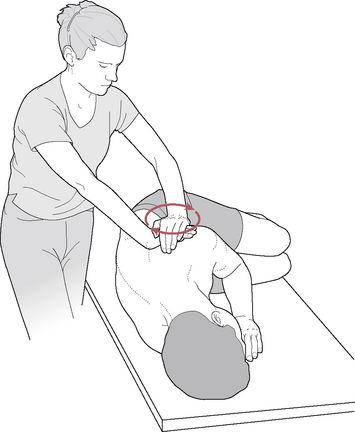
• Economy of effort relates to the concept of using the body efficiently in terms of reducing strain as well as energy output, thereby avoiding fatigue. Discussing the ‘principle of least effort’, chiropractor and Feldenkrais practitioner John Hannon (2000a) has described an example in which the standing practitioner engages the lateral border of the scapula of the sidelying patient in order to mobilize it.
The therapist positions himself so that his sternum faces the client’s scapular spine. He adjusts the table height until an easy folding of [his own] trunk is possible by forward bending at the hips (Fig. 4.3). His hands surround the top-most [superolateral aspect of the] scapula …By taking a broad, stable stance, it is possible for him to arrange his pelvis and trunk to counterpoise each other. In other words, by suitable arrangements, he creates an unstable equilibrium of his trunk upon his pelvis, and his legs upon his ankles…the therapist, by rocking his trunk forward upon his femoral heads, and by rocking his lower extremities backward upon his ankles, is able to maintain his balance [Fig. 4.4]. The reason for insisting upon a sense of balance is to avoid tensing of the fingers, stiffening of the arms, and holding of the breath, yet allowing the therapist to induce ‘therapeutic strain’ by merely tipping forward [and backward].
• Use of mechanical advantage encourages economy of effort and minimal personal strain for the practitioner. Hannon (2000b) uses the term ‘creating an irresistible force’ as he positions himself in relation to the patient and uses the forces available from gravity, inertia and skilled use of body mechanics and leverage to slowly and gently ‘oblige’ shortened or restricted tissues to yield, lengthen or mobilize. The difference, when attempting to stretch tissues, between use of ‘irresistible force’ and muscular force is the difference between gentle but persistent persuasion and coercion. Both ‘work’ but one is far more pleasant than the other.
Figure 4.4 Demonstration of standing in ‘unstable equilibrium’ as described in the text
(reproduced with permission from Journal of Bodywork and Movement Therapies 4(2): 119 with thanks to John Hannon DC).
Quoting at some length from Hannon (2000d) offers the reader an opportunity to understand more fully the somewhat abstract terms ‘inertia, gravity and skilled use of body mechanics’. It is suggested that reference be made to the notes on tensegrity structures in Volume 1, Chapter 1 in order to appreciate the use of sound physics in the application of the forces Hannon describes. Particular note should be taken of the way Hannon describes practitioner positioning, since this is subsequently used to achieve the greatest possible mechanical advantage, with minimal effort or personal stress.
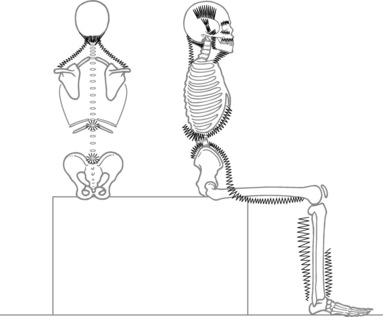
The therapist is sat on a stool, feet flat on the floor with the trunk hinged forward upon the sacrum. The ischia were perched solid, but freely rockable, upon the stool, with elbows wedged into the therapist’s distal medial thigh flesh. This allowed the bones of the thighs, elbows and spine to be stiffened into two triangles radiating out from the spine. [Fig. 4.5]…Gravity became the prime motive force for the treatment in this position; the practitioner simply rocked forward on the ischial contacts, and fell ever so slightly toward the client. Empirically, it seems that the client felt this touch to be much less strong and invasive as compared to that of clutched fingers pressed into the same point of anatomy. Rhythmic pressures were applied by a combination of trunk leaning and minimal [practitioner] thigh abduction/adduction. These movements drove the [practitioner’s] forearms forward into the contact with the client. The hands molded the contact upon the client’s thigh, remaining soft and malleable. … As the therapist rocked backward upon the stool, a tensile strain was applied to the client’s thigh. A twisting traction was created deep in the client’s thigh by selectively rocking and rotating upon one ischium and applying a compressive force strain with one hand and a tensile strain with the other.
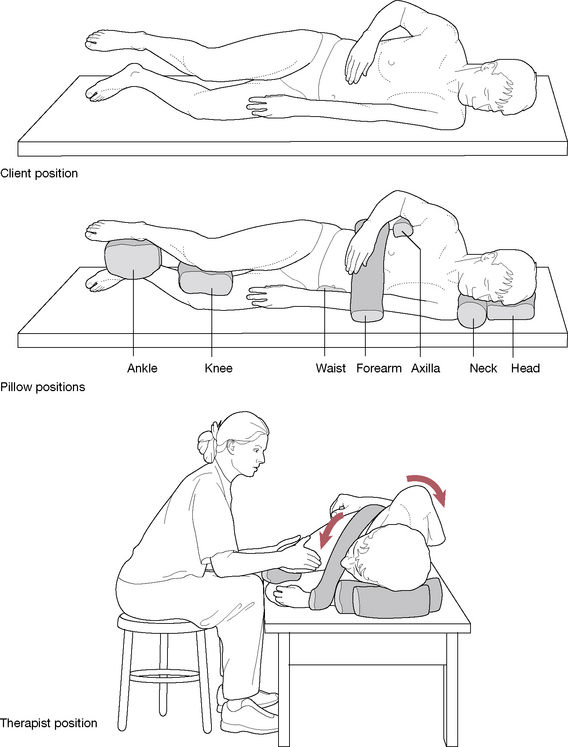
Figure 4.5 Therapist position to maximize stillness while performing myofascial release of the right proximal thigh (reproduced with permission from Journal of Bodywork and Movement Therapies 4(4):281 with thanks to John Hannon DC). Note: The authors have found that similar stable positioning of the patient is achievable using the bodyCushions™ available from Body Support Systems, Inc. Contact details are given below – on this page.*
These movements perfectly illustrate ‘least effort’ and utilize the transmission of forces through a tensegrity structure which has been created by the careful construction of an interaction between the practitioner and the client, in which any movement, whether pivoting on an ischial tuberosity or adduction of a thigh, transmits force through the contact hands and into the tissues. Hannon (2000d) then goes on to describe additional therapeutic processes in this case. The extensive extract quoted above gives insights into the use of forces such as gravity and inertia, which are freely available and which can be easily employed, without strain to practitioner or patient.
• A combination of the features of good ‘acture’ therefore involves sound positioning, a wide base of support, balance (and sometimes, in Hannon’s term, ‘unstable equilibrium’) and the ability to transfer weight and force by minimal repositioning of the practitioner’s body, employment of gravitational forces and tensegrity, all with the intent of achieving the principle of least effort (‘less is more’). A final thought from Hannon (2000c) is worthy of repetition. Stopping movement, but maintaining a monolithically static treatment contact would reduce some of the flow of sensation to the client and might sharpen their sensate focus. And stillness of the therapist would allow more control of the specific forces that impinge upon the client’s skin and joint fascial sensors. Just as an essential, if rarely considered, part of music is the silence between the notes, stillness may have a place in the manual therapist’s tool box. (see Box 4.1)
• It should be kept in mind that when the patient is placed in sidelying position, in most cases the height of the working surface changes. For example, the uppermost shoulder or hip is higher than the surface of the torso was when it was in a prone or supine position. It may be advantageous to keep a small platform nearby (such as is used in step aerobic classes) on which to stand, should elevation be needed in order to more effectively apply body weight. In the ideal practice setting, this problem could be eliminated by a hydraulic table, which could adjust the patient height with a touch of a button.
• For the patient’s comfort, bodyCushions™ may be used with the patient placed in various positions.* These cushions have been designed to encourage relaxation of the patient’s neuromusculoskeletal systems. It should be noted that the cushions add to the height of the working surface and the table height must be lowered, or the practitioner raised, in order to avoid strain.
Box 4.1 Hannon’s ‘treatment house-rules’ (Hannon 2000c)
1. Sit whenever possible (‘why should the client get all the rest?’). Sitting provides stability.
2. Have your feet on the floor to ‘take advantage of the solid ground reaction force to aid in precise delivery of force’. This is not possible if seated with legs dangling or if standing with weight on one leg only!
3. Use rocking movements to apply treatment force. A solid sitting perch together with having both feet planted allows fine control of the forces involved in contact with the patient.
4. Use pelvic movement potentials. ‘By cultivating an erect spine, solid footing and toned abdominal and gluteal muscles’ the pelvis can be put to work in pivoting and translating movements which transfer to the forces applied to the patient via the relaxed contacts with the patient’s tissues.
5. With firm but gentle contacts it is possible, when seated, to introduce strain, torque and traction into the patient’s tissues, by rotating your pelvis, balancing yourself on one ischial tuberosity which acts as an axis and utilizing variations in pressure from one foot or the other. Hannon refers to this as ‘turning the other cheek’.
6. Position the sternum and spine to line up with the area being worked on to reduce unnecessary strain.
7. Have the forearms symmetrical and parallel to the lines of force involved in the handling of the tissues being treated. This releases rotational stresses in the arm and hand muscles.
8. Maintain hand contacts soft and molded to the tissues. ‘Your hands last longer that way.’
9. Avoid excessive effort as this ‘blunts your senses, coarsens your treatment, and clouds your day with fatigue’. It also creates stress in what Hannon calls your ‘clench zones’, including suboccipital region, eyes, tongue, jaw, throat and diaphragm (Fig. 4.6).
11. Keep elbows heavy and relaxed.
12. Keep the spine erect and easy, not stiff. The lumbar spine is more easily maintained in neutral if flexion takes place at the hip joints.
Automobile influences
Sitting in a car can be a health hazard, especially for the driver. The link between driving and back pain is well established (Wilson 1994). A man who spends half the working day driving is 300% more likely to develop a herniated disc than the non-driver. For heavy vehicle drivers, the risk rises by 500% (McIlwraith 1993).
Driving: the vibration factor
Waddell (1998) has very strong opinions about the risks involved in sitting and driving, which he believes have more to do with the vibratory influences than the seated position. ‘Many studies show a higher prevalence of back pain, early degeneration of the spine and disc prolapse with driving. The key physical event seems to be exposure to whole-body vibration.’ He suggests that people who spend more than half their working time driving are particularly likely to suffer back trouble and points out that the vibratory frequency of many vehicles is 4–6 Hz which, according to Pope (1991), is also the resonating frequency of the spine. Wilson (1994) agrees that vibration and jarring increase the rate of muscle fatigue, accelerating the negative influence on discs of prolonged sitting. Good seating design together with good seated posture and optimal tire pressures, as well as the best possible automobile suspension, are all factors that can reduce the vibratory, jarring forces inherent in driving.
Automobile risk factors
• The design of the driver’s seat may be inappropriately offset in relation to the foot controls in some cars, causing a permanent torsion of one or both legs, or of the pelvis, when driving.
• The driver’s seat may not be adjustable for height, in which case the body size of the driver may be inappropriate for that particular car. There should be at least 10 cm (4 inches) head clearance when sitting comfortably, not slumped, and the shorter driver should be able to easily see over the dashboard without straining.
• The driver’s vision may be compromised due to the seating position and, if so, head, neck and back strain and distortion become likely. It is clearly easier for a short individual to increase height by means of a cushion than for a tall driver to contort to fit into a low-roofed vehicle. The height of the roof in relation to the height of the tall individual is therefore a more critical feature than the height of the dashboard is to a short person, since it cannot be as easily corrected. Some automobiles have adjustable seat height, which may eliminate this particular hazard.
• Seat design should ensure that the seat could be reclined and raised/lowered to meet the needs of the driver’s body type. Seating should also be contoured to support the back, ideally with an adjustable lumbar support area and side support.
• The headrest should be adjustable with a tilt potential.
• Lumbar support may be missing or non-adjustable. A lumbar roll or purchased car seat overlay which offers lumbar support can be added to those cars which lack adequate support.
• Poor steering-wheel design may create awkward body positioning, depending on the driver’s body type and other physical characteristics (for example, there may be special needs due to body height and/or length of the arms). Most such problems are eased if the steering mechanism is adjustable and further eased if there is power steering.
• Air conditioning, if used excessively and/or if streams of cold air are inappropriately directed, can exacerbate muscle discomfort and produce aggravation of trigger point activity, particularly in the neck and shoulder areas.
• The amount of time spent in the driving position, as well as the number of times the individual gets in and out of the car, are key contributing factors to the development of backache linked to driving. Within this text it is recommended to stop frequently to get out and move about; however, the effort of extracting oneself from the car can also be a stress factor and more so if the back is already irritated. Proper positioning of the body while getting in and out of the car is therefore a critical factor.
• Wilson (1994) lists the driving-related features, which were self-reported by a group of drivers with backache as aggravating factors:
Most driver-related problems, however, are solvable by inexpensive and relatively simple strategies such as inclusion of a lumbar support or a cushion to increase height, proper body usage when getting in and out of the car, the use of a small yet solidly based step stool when climbing in and out of high vehicles and by ensuring regular breaks if driving is prolonged, say 5–7 minutes every hour, for a stretch and a walk (Wilson 1994). Despite the obvious inconvenience, such breaks should be taken every hour, if possible, and not accumulated to be a longer break every 3 hours. This is especially important for the person who already suffers from back pain. Leisure time should include muscle-toning exercise activities that focus on the abdominal and back stabilizing muscles and should be incorporated into daily life and not just sporadically interspersed during a trip.
Seatbelts and airbags
Over and above its profound influence on seated posture, automobile design has the potential, through seatbelt and/or airbag-induced trauma, to contribute in a major way to injuries sustained in road accidents. Nordhoff (2000) offers clear insights into the processes that occur in relation to motor vehicle accidents. He also cites evidence that suggests that in many instances seatbelts are responsible for more injury than any other physical part of an automobile (although they undoubtedly reduce fatalities).
Gender issues in accident after-effects
• Major research studies show that women report injuries from traffic accidents twice as frequently as men (Murphy 2000).
• A French study evaluated injuries in 1500 car occupants involved in motor vehicle accidents and reported that 47% of female occupants and 21% of male occupants had cervical injuries (Foret-Bruno 1991).
• A Swedish study showed that regardless of the size of the car involved, women incurred more neck injuries than men (Koch 1995).
• Nordhoff (2000) suggests this gender difference may be because of the smaller neck diameter in females, as well as (in general) smaller body mass and therefore a higher rebound velocity from seatbacks, especially with rear-end accidents.
Multiple symptoms and fibromyalgia syndrome (FMS) following vehicle injuries
Larder (1985) analyzed the pattern of symptoms following motor vehicle injury and found that:
• there was a mean patient reporting of 3.1 symptoms
• most common symptoms related to neck pain (94.2%), headaches (71.5%), shoulder pain (48.9%), low back pain (37.2%), visual disturbance (21.1%) and loss of balance (16.1%) along with other symptoms including vertigo, tinnitus and radicular irritation
• fatigue, anxiety, sleep disorders and a range of musculoskeletal problems, such as thoracic outlet and carpal tunnel syndromes, and TMJ disorders were also reported
• symptoms did not always appear soon after the injury, but often up to 96 hours later.
Chester (1991) noted that a diagnosis of fibromyalgia was present in more than 50% of 48 rear-end motor vehicle crash cases, in a 7 month – 7 year study.
A study involving over 100 patients with traumatic neck injury as well as approximately 60 patients with leg trauma evaluated the presence of severe pain (fibromyalgia syndrome) an average of 12 months post trauma (Buskila & Neumann 1997).
• The findings were that ‘almost all symptoms were significantly more prevalent or severe in the patients with neck injury [i.e. whiplash] … The fibromyalgia prevalence rate in the neck injury group was 13 times greater than the leg fracture group’.
• Pain threshold levels were significantly lower, tender point counts were higher and quality of life was worse in the neck injury patients as compared with leg injury subjects.
• Over 21% of the patients with neck injury (none of whom had chronic pain problems prior to the injury) developed fibromyalgia within 3.2 months of trauma as against only 1.7% of the leg fracture patients (not significantly different from the general population).
• The researchers make a particular point of noting that: ‘In spite of the injury or the presence of FMS, all patients were employed at the time of examination and that insurance claims were not associated with increased FMS symptoms or impaired functioning’.
Murphy (2000) reports that: ‘Post-traumatic FMS is usually unilateral in its presentation [because] most motor vehicle crashes load the human body with asymmetrical forces’.
Simons et al (1999) report that headache symptoms may not arise for weeks after the trauma, while Moles (1989) and Kaplan & Williams (1988) state that damage to the TMJ may not become apparent for months after the ‘whiplash’ has occurred.
Wenberg & Thomas (2000) observe:
When someone suffers a cervical or temporomandibular strain following a whiplash-type injury, it is logical to suspect additional structural insult to nearby tissues. The same shearing forces that tear and damage the cervical musculature may also damage fascial structures and neurons in the brain and brainstem. The visual system is exceptionally vulnerable. Burke (1992) clearly correlates ocular motor complications with whiplash. Such damage can severely compromise the rest of the body through alterations in gait, as proprioceptive information reaching the brain becomes unreliable (see Chapter 3 on proprioceptive influences on gait).
The vehicle injury close environment
The driver or occupant, if wearing a seatbelt, is likely to sustain injuries at the seatbelt’s points of contact, most notably the neck. In a study of over 3000 accidents, 20% of occupants reported neck injuries (mostly minor) directly resulting from seatbelts, as against only 8% of unrestrained individuals (Morris & Thomas 1996).
A further study of almost 4000 accident occupants showed that 21% of the belted and 14% of the non-belted occupants reported neck injuries (Maag et al 1990) (Fig. 4.7).
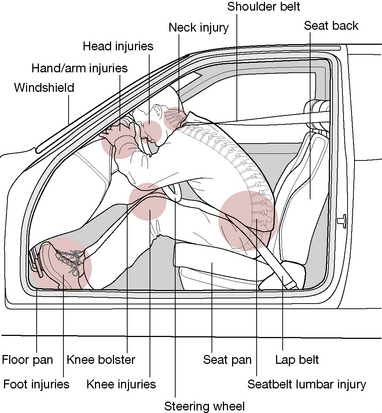
Figure 4.7 Frontal impact forces from interior elements of automobile in head-on crash
(adapted from Nordhoff 2000).
As Nordhoff (2000) explains: ‘With all restrained occupants, regardless of seating position, the seat belt is responsible for generating more injuries than any other contact source within the vehicle’. Most such injuries are minor and most occur because the seatbelt is working precisely as it was designed to do.
In such circumstances severe damage may occur, including fatalities, as the vulnerable anterior neck takes the force of impact. This type of injury is more likely with small adults and children; the use of booster seats for children between 40–80 pounds is strongly urged (see Box 4.2).
Box 4.2 Protecting the child passenger
The objective in choosing and using restraining devices should be to reduce the chance of these impacts and, at the same time, reduce (as much as possible) potential injury by the restraining device itself by using it properly. Vehicle design, airbags and snug-fitting seatbelts (with shoulder harnesses) all assist in protecting the adult body during the crash. The tighter the seatbelts are adjusted, the lower the body’s overall deceleration, thereby reducing the potential rate of impact between the skeleton and internal organs (including the brain against the skull) (Weber 2000). Additionally, distributing the load of impact as widely as possible and onto the strongest body parts (in adults, primarily the shoulder and pelvis and secondly the chest) optimally reduces impact injury.
• child can sit with lumbar spine and upper buttocks fully against the seatback
• the knees bend at a 90° angle at the seat edge
• shoulder belt fits across the shoulder
• lap belt over the thighs or bony pelvis
• the child is mature enough to sit reasonably still during the ride (Sachs & Tombrello 2000).
Since the younger child (either backward or forward facing) is buckled into a restraining device by a harness or shield and then the child restraint device itself must also be buckled down, great care must be taken to assure that both systems are tightly fastened to avoid excessive movement or ejection of the child, or child with car seat, during a crash. Weber (2000) notes: ‘A large observation study in four states found that about 80% of child restraints were not being used as intended (Decina & Kneobel 1997)…Clearly a failure to anchor the CR [child restraint] or to harness the child is about the same as nonuse, but there are many other opportunities to do the wrong thing’. These mistakes may include inadequate tightening of the harness that holds the child, or of the seatbelt that restrains the car seat, or the use of the wrong type of seatbelt for that particular restraining device.
When the child matures to (about) 4 years old and 40 lbs and his height or weight surpasses the upper limits recommended by the manufacturer (many manufacturers use different weight and height limits so read instructions carefully), many adults erroneously conclude that the child should be advanced to adult seatbelts. At this stage, the child’s body is still too small to properly fit the adult belt. Proper placement of the seatbelt includes the lap portion of the belt fitting snugly across the bony portion of the pelvis and with the shoulder strap fitting across the mid-sternum and crossing the shoulder about halfway between the neck and the arm. With the child’s body (especially upon impact), the lap belt rides up into the fleshy abdomen and the shoulder strap onto the anterior cervical region, often resulting in serious (including spinal cord) injuries (Weber 2000). Equally or more dangerous is the practice of placing the shoulder portion behind the child or under the arm to avoid irritation to the neck, resulting (upon impact or even during hard braking) in the child submarining under the belt or being ejected over it, leading to serious injury or fatality. The child who cannot achieve a proper fit of both lap and shoulder belt should ride in a booster seat specifically designed to adapt the adult seatbelt to the child’s body.
Weber (2000) reports:
A lap belt that is placed or rides up above the hips can intrude into the soft abdomen and rupture or lacerate internal organs (Rouhana 1993, Rutledge et al 1991). Moreover, in the absence of a shoulder restraint, a lap belt worn high can act as a fulcrum around which the lumbar spine flexes, possibly causing separation or fracture of the lumbar vertebrae in a severe crash…A belt-positioning booster (BPB) raises the child so that its body geometry is more like that of an adult and helps route a lap/shoulder belt to fit that body size.
The National Highway Traffic Safety Administration (NHTSA 2000) is responsible for developing a comprehensive 5-year strategic plan to reduce deaths and injuries caused by failure to use the appropriate booster seat in the 4–8-year-old age group. The NHTSA notes that in February 2000 they launched their ‘Don’t Skip a Step national booster seat campaign to educate parents about the risks of improperly positioned adult seat belts and the effectiveness of belt-positioning booster seats for children ages 4 to 8 years’.
• American Academy of Pediatrics – www.aap.org (great information for typical and atypical children)
• National Center for Injury Prevention – www.cdc.gov/injury/
• Insurance Institute of Highway Safety – www.highwaysafety.org
• National Highway Traffic Safety Administration – www.nhtsa.dot.gov
• SafetyBeltSafe USA – www.carseat.org
• University of Michigan Transportation Research Institute (UMTRI) Research Review (newsletter – $35/yr subscription) – www.umtri.umich.edu
Airbag injuries are different from those deriving from seatbelt restraints. There tend to be far fewer neck and skull injuries with airbags but far more brain injuries, as well as upper and lower limb injuries resulting from air-bag deployment. Caution has been suggested regarding the distance and positioning of the upper body and head of the driver from the steering wheel which houses the airbag. The force of deployment is significantly greater, as is the danger of head damage and facial laceration, when closer than 38 cm (15 inches) (Dischinger et al 1996).
Children under 12 years of age should not ride in a seat that has a frontal-impact airbag as serious injury and a substantially increased risk of fatality may result from the impact of the airbag. This is especially true for young children and, in particular, infants in rear-facing restraints placed in front seats with airbags. Regarding subsequent airbag deployment, Weber (2000) reports:
Nordhoff (2000) describes the mechanisms of trauma relating to motor vehicle collisions.
• First mechanism: vertical (axial) lengthening of the spine – an ‘accordion’ effect created via seatback pressure.
• Second mechanism: segmental motion may occur beyond normal anatomical limits as sternocleidomastoid pulls on the skull when the torso moves forward and the head lags behind.
• Third mechanism: swift extension-flexion of the neck increases cerebrospinal fluid and blood pressure to approximately 10 times greater than normal for milliseconds (called the ‘blood hammer’), leading to damage to spinal nerve ganglia; injury to lower cervical and upper thoracic nerve roots and spinal ganglia due to mechanical strain during extension stress.
• Fourth mechanism: global hyperextension of the neck beyond the normal anatomical limits of its ligaments, joint capsules and muscles; even low speeds (under 10 mph) can produce musculoligamentous tears, hemorrhage and even disc avulsion, especially if the head was rotated at the time of impact. At higher velocities compression fractures of the vertebrae may result.
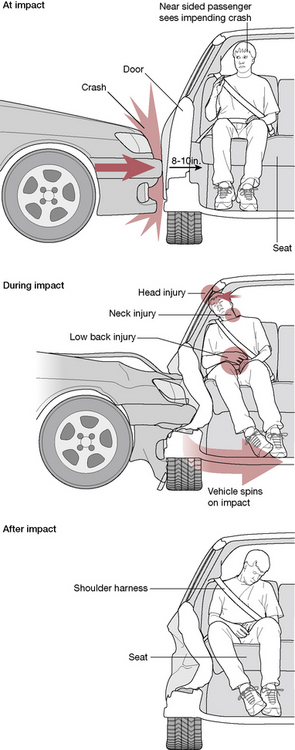
Side-impact collisions (Fig. 4.8) are commonly more severe than front-end collisions because there is little to absorb impact energy other than the side of the vehicle. This usually violently loads the occupant’s torso and pelvis laterally while the head remains behind. Cervical and back injuries commonly involve disc damage. Side-impact airbags are beginning to appear with industry efforts focused on development of side airbags that will minimize injury risk to occupants (Weber 2000).
Several points made in Box 4.2 regarding children’s bodies apply also to those adults who are shorter than the ‘average’ body for which cars are designed. Additional details from that box remind us that, for the MVA patient, a series of collisions occurred, not just the primary one. After primary impact, the patient’s body (unless ejected from the vehicle) continues to move at the precrash speed until it is restrained by the seatbelts or other restraint, at which time the head/neck, arms, and legs continue to move until they reached the elastic limits of (or tore) their associated soft tissues, or impact the interior of the vehicle. The internal organs continue to move and very likely will impact against the bony structures that enclose them (brain to skull, lungs to ribs, etc.), each of these organs being enmeshed in an envelope of fascia that may also sustain injury or become an adherent ‘glue’ that fixates the organ to the bone. It is important when preparing a treatment plan to consider these and other possibilities, and to include assessment, treatment or referral to other health care practitioners in a whole body therapeutic approach.
Sitting on an airplane
• Talking with the head turned to one side for an extensive time, which can activate trigger points in levator scapula (Simons et al 1999) and other cervical muscles. Active, repeated rotation to the opposite side periodically during the conversation to stretch the shortened muscles will help reduce risk.
• Falling asleep with the head in a tilted position can activate trigger points, especially with a cold draft blowing from the air conditioner (Simons et al 1999). An inflatable neck pillow can support the head while conscious effort to avoid drafts or cover the neck when sleeping will reduce risk.
• Prolonged sitting can shorten the soleus and gastrocnemius muscles, which can activate trigger points in them. The soleus pedal exercise (Fig. 4.9) can be incorporated while seated during flight for active stretch of the soleus as well as to enhance the vascular pumping action this muscle offers (Travell & Simons 1992).
• Trigger points may be activated in the hamstring muscles if these are compressed against the edge of the seat, especially if the legs are too short to comfortably contact the floor (Travell & Simons 1992). A briefcase, book or other carry-on items can support the feet to elevate the legs. Alternatively a small, portable folding footrest (which stores easily in carry-on luggage or briefcase) can be purchased from occupation therapy supply catalogs such as the one detailed below.* Non-folding versions are also available which can be placed at a desk, reading station or other areas where portability is not a consideration.
• A combination of dehydration, prolonged sitting (especially on long flights) and reduced oxygenation in pressurized cabins contributes to the risk of ‘economy class syndrome’, involving potentially life-threatening deep vein thrombosis (DVT)/pulmonary emboli. These conditions may occur from clots arising from pooling of blood in the feet and legs as well as cramped conditions. People most susceptible to this are those who drink too much alcohol, use sleeping pills and/or are overweight. Avoidance of alcohol, adequate water intake and movement of the limbs when seated are all helpful in reducing these risks.
• For anyone at particular risk of DVT (markedly overweight, history of venous problems especially previous DVT, congestive heart conditions, elevation of clotting factors postoperatively or postpartum, recent fracture resulting in elevated platelet coagulant factors) prophylaxis should also include the wearing of elastic support stockings during flight, as well as consulting (prior to flying) a medical practitioner to evaluate the possible benefits of anticoagulant medication prophylactically (e.g. mini-doses of heparin or warfarin (Tikoff 1983) or self-administered aspirin, or garlic extracts (Kiesewetter 1993, Phelps & Harris 1993)).
• People with breathing pattern disorders (such as hyperventilation) are put at extra risk on long flights where aircraft may reach 35 000 to 37 000 feet above sea level for 10–12 hours. Cabins are, of course, pressurized to prevent altitude hypoxia and to ensure the comfort of the traveler. While older aircraft (such as the Boeing 737) relied entirely on fresh air flowing through all the aircraft’s sections, fuel conservation strategies in modern planes have led to the recycling of used air, mixed with fresh air in varying proportions, which can result in the reduction of the levels of available oxygen.
• Hyperventilation is a classic manifestation of ‘fear of flying’ and those suffering this may experience signs and symptoms of hypocapnia (decreased arterial carbon dioxide tension). ‘Fear of flying’ courses may help and should cover these issues. Much of this training and conditioning is based on maintaining breathing control, as well as cognitive skills to manage fear (Bradley 1998).
• Concerns for air travel safety and security issues that create delays in the process of arriving at the plane produce anxiety, provoke adrenal responses and create additional stresses. Poor food choices within the airport and on the plane add to the body’s challenges to maintain adequate nutritional stores and healthy energy. Frequent travelers and business travelers, in particular, may resort to caffeine, ‘power bars’, and other substances, in order to maintain the energy needed to work during the flight, attend meetings upon arrival, and to complete the travel ‘mission’. Despite the body’s need for recovery from the trip, as well as from altitude and temperature variations and the impact of time zone differences, many often push through it, only to repeat the process in a few days (or hours) with the next leg of the journey.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree