Interest in understanding psychopathy continued from the nineteenth century into the twentieth century. Based on interviews conducted with hundreds of prisoners, Cleckley formed a narrative conceptualization and description of psychopathic personality structure and dimensions [9]. Subsequently, Hare and others organized the conceptualization of psychopathy into a 2-factor model, i.e., aggressive narcissism and deviant antisocial lifestyle [10]. This 2-factor model was later refined into 1-, 3-, and 4-factor models, with the latter composed of interpersonal deficits characterized by lack of affiliative attachment; affective deficits characterized by lack of fear and empathy; antisocial lifestyle characterized by lack of prosocial goals and behaviors; and overt antisocial acts characterized by a callous disregard for the rights and welfare of others [11].
It is worth noting that although the 4-factor model has become dominant, controversy and debate continue regarding the factor-analytic structure of psychopathy, as well as debate as to whether psychopathy should best be conceptualized in categorical versus dimensional terms. In parallel with the evolving psychological modeling of psychopathy, Raine [12] and others reported that a blunted autonomic response to frightening images during childhood was directly correlated with later criminal behavior. Conversely, increased childhood autonomic responsiveness was found to be inversely correlated with later violent and criminal behavior [12]. Taken together with prior psychological assessments indicating that diminished interpersonal affective responsiveness was a core component of psychopathy, it came to be widely hypothesized that the observed autonomic hyporeactivity was the substrate of psychopathic personality structure development [13]. This hypothesis, in turn, has driven several lines of research aimed at understanding the neurobiology of psychopathy. Such understanding of the neural structures and distortions of neural circuit activity that underlie psychopathy are critical to identifying effective means of treatment to ameliorate the burden of violence and suffering imposed on others by psychopathic individuals [14].
Review of Recent Developments
Classically, it has been observed that childhood adversity or trauma can give rise to emotional and adaptive states that may go on to become persisting personality traits [15]. A recent meta-analysis of 27 peer-reviewed studies of nonclinical samples published through August 2012 found a positive correlation between childhood adversity, including trauma, and a lower transcription efficiency polymorphism of the gene for monoamine oxidase, type A (MAOA). Diminished expression of MAOA leads to diminished catabolic capacity for norepinephrine and serotonin, and was associated with the development of antisocial features (callous violence, substance abuse, and criminal behavior) in men, as well as a similar, but less robust, relationship in women [16]. Nevertheless, it is worth noting that a study of 3356 Caucasian men and 960 African-American men failed to confirm the interaction of childhood maltreatment, lesser MAOA transcriptional efficiency, and development of antisocial behavior [17]. Thus, while an interaction of childhood adversity and altered brain catecholamine/indoleamine activity remains an attractive research area regarding the development of psychopathic personality characteristics, the data remain inconclusive.
Additional genes implicated, at least indirectly, in development of psychopathic personality structure include the Val-Met polymorphism of the gene coding for the amino acid sequence of brain-derived neurotrophic factor (BDNF), the oxytocin receptor gene polymorphism RS53576, and polymorphisms of the genes involved in serotonin signal transduction [18–20]. More specifically, the Met-Met variant of the gene coding for BDNF made child and adolescent males more vulnerable to aggressive influences by peers. The RS53576 oxytocin receptor polymorphism was associated with diminished capacity to form affiliative attachments during periods of distress. Additionally, single nucleotide polymorphisms diminishing 5HT-1B and 5HT-2A receptor serotonin signal transduction were associated with callous and unemotional traits in adolescent males.
Moreover, genetic studies to date underscore the importance of interactions between the inherited genetic polymorphisms and negative childhood and adolescent events and influences. These observations of the importance of genetic and environmental interactions comport with Raine’s early observation that a minority of his autonomically hyporeactive children went on to develop prosocial lives and careers, e.g., police officers, bomb disposal experts, test pilots, etc., rather than becoming criminals [12]. These observations suggest that early interventions designed to limit childhood adversity and combat antisocial influences can ameliorate the development of psychopathy. Despite this promise, it should be noted that prior attempts to extend diagnostic and intervention approaches to children and adolescents have found the developmental pathways into psychopathy and, consequently, intervention responses to be complex [21]. Nevertheless, it can be speculated that continued genetic research may yield future specific biological targets for the risk screening, prevention, or treatment of psychopathy.
Although not topographically precise, many electroencephalographic (EEG) studies have associated forebrain circuit dysfunction and psychopathy. For example, a recent study of four men with medication-resistant medial prefrontal lobe epilepsy who exhibited antisocial behaviors found that the antisocial behaviors resolved following surgical ablation of the epileptiform or seizure foci [22]. Event-related investigation of psychopathic individuals has shown an inverse relationship between P3 amplitude, reflecting cortical electrical activity at c. 300 ms post event, and proneness to externalizing behaviors, suggesting a deficit in cortical attention in the context of introspective moral and empathetic processing [23]. Another study of psychopaths found that P3 amplitude was diminished in response to abrupt auditory stimuli and was directly correlated with interpersonal affective deficits [24]. These observations seem especially enlightening, given recent spatiotemporal electroencephalographic data suggesting that in healthy controls, processing of moral decisions involves first a processing of affective interpersonal context within the temporal lobes, followed by ventromedial prefrontal cortical processing of ethical and empathetic factors [25]. Taken together, these studies lead to the speculation that improved temporal lobe and ventromedial prefrontal communication and cortical processing in the contexts of affiliative interpersonal affective connections and processing of moral decisions might ameliorate psychopathic behavior.
A variety of anatomic and functional imaging studies have implicated dysfunction of the amygdala as a core element of psychopathy [14]. In particular, although antisocial personality disorder and psychopathy overlap substantially, differential dysfunction in which the amygdala nuclei fail to respond to images designed to convey fear or negative emotion distinguish psychopaths from nonpsychopathic antisocial individuals [26]. Ancillary dysfunction of the fusiform gyrus also has been implicated in psychopaths in the context of inability to interpret negative facial expressions [27]. Finally, psychopaths exhibit a failure to activate the temporal lobe poles in response to anxiety-provoking stimuli [28]. Taken together, these studies suggest that in the psychopathic brain, the temporal lobes fail to adequately process emotional and social cues associated with negative emotions, resulting in an attenuated output signal to the ventromedial prefrontal cortex (VMPC). This lapse would appear to be a critical defect in initiating moral or ethical judgments [25].
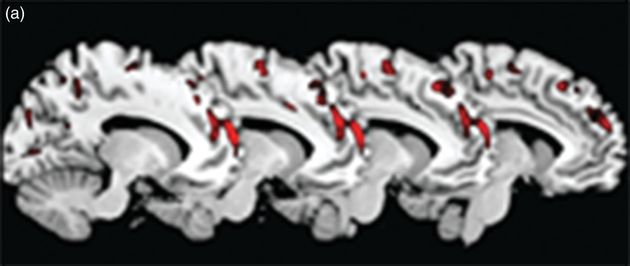
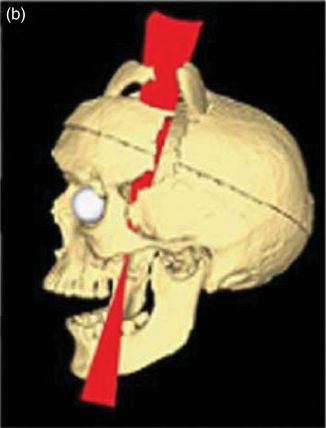
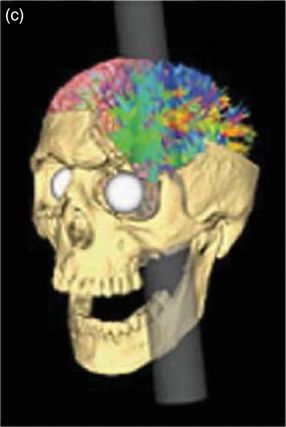
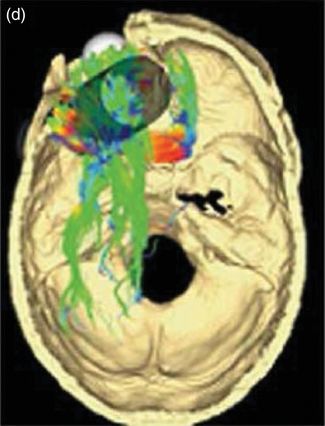
As suggested, the VMPC appears to be pivotal to processing of the utilitarian or consequential aspects of moral and ethical judgments. In this context, the amygdala provides input regarding aversive affective context [29]. Recent magnetic resonance imaging (MRI) and functional magnetic resonance (fMRI) studies have affirmed prior observations of decreased amygdala and VMPC gray matter, but have gone further in identifying decreased connectivity between the amygdala nuclei, as well as other anterior temporal lobe structures and the VMPC via the uncinate fasciculus, but increased connectivity between the VMPC and the dorsolateral prefrontal cortex in psychopaths [30–32]. Moreover, it has been hypothesized that this neural circuit configuration underlies the callous, non-empathetic, unemotional, amoral, and inflexible features of psychopathic personality structure. White matter abnormalities also have been identified with respect to the genu of the corpus callosum and the fronto-occipital tract; however, the functional meaning of these observations remains to be fully investigated [33,34]. An illustration of gray matter deficits in psychopaths compared to nonpsychopathic antisocial individuals is shown in Figure 12.2 [35].
Additional forebrain and striatal structures have been found to play roles in psychopathic individuals. For example, impaired signal transduction between the VMPC and the mirror neuron network in the interhemispheric prefrontal cortex has been hypothesized to underlie the deficit observed in psychopaths to develop empathy or to appreciate the mental states of others [36]. Similarly, inadequate frontotemporal communication with the cingulate gyrus may result in difficulty distinguishing one’s egocentric desires and values from those of others, contributing to a narcissistic social perspective [37]. Also, diminished VMPC top-down suppression, coupled with hypersensitivity of the ventral tegmental area and nucleus accumbens (hypothalamus) to anticipated reward, have been hypothesized to underlie the impulsivity and increased addiction liability of psychopaths [38].
In sum, considering the 4-factor model of psychopathy derived from studies of the Psychopathy Checklist, Revised (PCLR) [39], neural structures appear to align as illustrated in Table 12.1.
| PCLR factor | Associated brain structures | Clinical correlates |
|---|---|---|
| Interpersonal deficits | VMPC | Impaired capacities to make ethical judgments about harm to others |
| Mirror neuronal network | Impaired capacity to make interpersonal attachments | |
| Cingulate cortex | Impaired capacity to appreciate values of others | |
| Affective deficits | Amygdala | Blunted response to fearful or negative emotional stimuli |
| Temporal poles | Diminished fear response | |
| Uncinate fasiculus | Attenuated output of affective information to the VMPC | |
| Fusiform gyrus | Deficit in recognizing negative emotions in faces of others | |
| Antisocial lifestyle | VMPC | Insensitivity to social obligations |
| Cingulate gyrus | Narcissistic viewpoint | |
| Mirror neuronal network | Lack of empathic responses | |
| Antisocial acts | VMPC | Impaired impulse inhibition |
| Ventral striatum/nucleus accumbens | Reward hypersensitivity |
PCLR = Psychopathy Checklist, Revised; VMPC = ventromedial prefrontal cortex.
To date, society has dealt with criminal psychopaths primarily via incarceration or execution; however, even in secure correctional or forensic psychiatric settings, such individuals inflict disproportionate violence on others and engage in antisocial enterprises [40–42]. In particular, it has been noted that within forensic psychiatric systems, it is likely vital to be able to match the level of security to the level of risk [43]. That is, external successful amelioration of violent and antisocial behaviors depends on being able to move the psychopathic individual into more secure settings when risks are elevated and to return the individual to lesser levels of security when levels of risk are ameliorated. As previously noted, the majority of confined psychopathic individuals return to the community.
Prior observations that not all persons with the biological substrate for psychopathy go on to become criminal or violent, coupled with recent observations that psychopaths can be trained to exhibit empathy, hold promise that inherent plasticity in forebrain circuits may permit development of more prosocial responses among psychopaths [12,44]. This working knowledge is the underlying basis for recent psychosocial approaches, such as risk–needs–responsivity (RNR) treatment programs [45].
Such treatment programs have shown positive preliminary treatment outcomes.
Historically, pharmacological approaches to treating violent and criminal behavior in psychopathic persons have been disappointing, as compared to pharmacological responses in other pathological personality structures [46–48]. For example, while lithium reduced impulsive violence and irritability in a group of chronically aggressive prisoners, it did not alter instrumental violence or overall criminality [49]. Similarly, a double-blind randomized trial of sertraline reduced impulsivity but increased fearlessness and dominance of others [50]. Importantly, however, preliminary data from a case series study of severely psychopathic nonpsychotic individuals treated with clozapine in a high-security forensic psychiatric hospital demonstrated impressive reductions in violence in six of seven patients at modest plasma concentrations of clozapine (mean 171 ng/ml) [51]. Recently, there has been speculation regarding the potential benefits of electrical modulation of amygdala and nucleus accumbens activity in the context of psychiatric disorders; however, no data yet exist with respect to psychopathy or other mental disorders [52].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree