The Ocular Motor Nerves
The oculomotor, or third cranial nerve (CN III) arises from the oculomotor nuclear complex in the midbrain and conveys motor fibers to extraocular muscles, plus parasympathetic fibers to the pupil and ciliary body. A single midline structure, the central caudal nucleus, supplies the levator palpebrae muscles on both sides. The periaqueductal gray matter is also involved with eyelid function. The Edinger-Westphal (EW) subnucleus is a single structure that provides parasympathetic innervation to both eyes. The fibers of CN III course anteriorly through the mesencephalon, traversing the medial portion of the red nucleus and the substantia nigra. The nerve exits from the interpeduncular fossa on the anterior surface of the midbrain. It passes between the superior cerebellar and posterior cerebral arteries, then runs forward parallel to the posterior communicating artery. In its course toward the cavernous sinus, it lies on the free edge of the tentorium cerebelli, medial to the temporal lobe. CN III penetrates the dura just lateral and anterior to the posterior clinoid processes and enters the cavernous sinus. In the cavernous sinus, CN III has important relationships with the carotid artery, ascending pericarotid sympathetics, and CNs IV, V, and VI. CN III separates into its superior and inferior divisions in the anterior cavernous sinus, then enters the orbit through the superior orbital fissure.
The trochlear, or fourth cranial, nerve (CN IV) arises from the trochlear nucleus located just anterior to the aqueduct at the level of the inferior colliculus. The nerve filaments curve posteriorly around the aqueduct, decussate in the anterior medullary velum and exit through the tectum. It is the only cranial nerve to exit from the brainstem posteriorly. It penetrates the dura just behind and lateral to the posterior clinoid processes. Leaving the cavernous sinus, it traverses the superior orbital fissure, enters the orbit, and crosses over CN III to terminate on the superior oblique muscle on the side opposite the nucleus of origin.
The nucleus of the abducens, or sixth cranial, nerve (CN VI) lies in the mid to lower pons, encircled by the looping fibers of the facial nerve. The nerve exits anteriorly at the pontomedullary junction, then ascends the clivus in the prepontine cistern. It passes near the Gasserian ganglion, pierces the dura at the dorsum sellae, and enters the cavernous sinus in company with CNs III and IV, where it lies below and medial to CN III and just lateral to the internal carotid artery. CN VI is the only nerve that lies free in the lumen of the sinus; the others are in the wall. It enters the orbit through the superior orbital fissure to innervate the lateral rectus.
Examination of the eyes begins with inspection—looking for any obvious ocular malalignment, abnormal lid position, or abnormalities of the position of the globe within the orbit. Abnormalities of the external eye may occasionally be of diagnostic significance in neurologic patients.
Tortuous (“corkscrew”) blood vessels in the conjunctiva occur with carotid cavernous fistula, or there may be jaundice, evidence of iritis, Kayser-Fleischer rings, chemosis, dysmorphic changes (e.g., epicanthal folds), xanthelasma due to hypercholesterolemia, keratoconjunctivitis sicca, premature cataract, or ocular complications of upper facial paralysis. Basal skull fractures often cause bilateral periorbital ecchymosis (raccoon eyes).
Tortuous (“corkscrew”) blood vessels in the conjunctiva occur with carotid cavernous fistula, or there may be jaundice, evidence of iritis, Kayser-Fleischer rings, chemosis, dysmorphic changes (e.g., epicanthal folds), xanthelasma due to hypercholesterolemia, keratoconjunctivitis sicca, premature cataract, or ocular complications of upper facial paralysis. Basal skull fractures often cause bilateral periorbital ecchymosis (raccoon eyes).
Exophthalmos
The globe may be abnormally positioned within the orbit so that it protrudes (exophthalmos, proptosis) or recedes (enophthalmos). Subtle proptosis can often be better appreciated by looking down at both eyes from above the vertex of the head, or by comparing side views. Exophthalmos is usually bilateral and most commonly due to thyroid eye disease ([TED], Graves ophthalmopathy, Graves orbitopathy); thyroid disease can have a host of neurologic complications. Some of the neurologically significant causes of unilateral proptosis include orbital mass lesion, carotid cavernous fistula, cavernous sinus thrombosis, sphenoid wing meningioma, meningocele, and mucormycosis.
The Eyelids
Patients may couch the complaint of ptosis in ways other than droopy eyelid (e.g., eye has shrunk). Ptosis may have been present for a very long time before coming to the patient’s attention. Looking at old photographs is often helpful. Note the position of the eyelids and the width of the palpebral fissures bilaterally. Note the amount of iris or pupil covered by the lid. The normal upper eyelid in primary position crosses the iris between the limbus (junction of the iris and sclera) and the pupil, usually 1 mm to 2 mm below the limbus; the lower lid touches or crosses slightly above the limbus. Normally there is no sclera showing above the iris. The width of the palpebral fissures should be equal on both sides, although a slight difference occurs in many normal individuals. The palpebral fissures are normally 9 mm to 12 mm from upper to lower lid margin. Measurement can also be made from the lid margin to the corneal light reflex. The upper lid margin is normally 3 mm to 4 mm above the light reflex. Patients may try to compensate for ptosis by contracting the frontalis muscle, causing a telltale wrinkling of the ipsilateral forehead. If the examiner fixes the frontalis muscle with her finger, the patient may be unable to raise the eyelid.
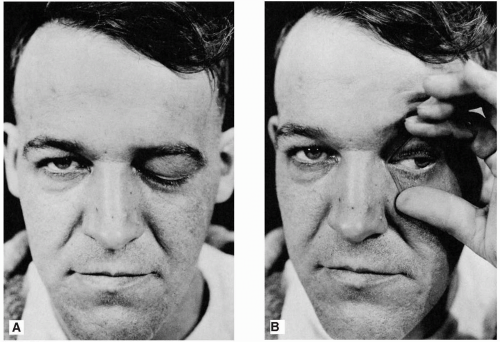
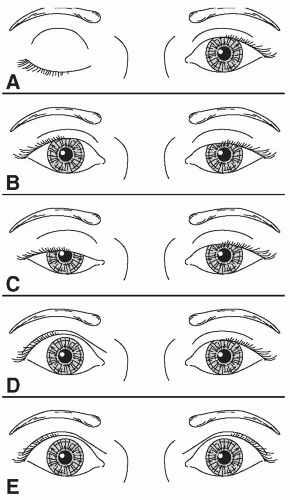
With ptosis, the lid droops down and may cross at the upper margin of the pupil, or cover the pupil partially or totally. With complete ptosis, the eyelid is down and the eye appears closed (Figure 10.1). Ptosis may be unilateral or bilateral, partial or complete, and occurs in many neurologic conditions (Figure 10.2). With eyelid retraction, the upper lid pulls back and frequently exposes a thin crescent of sclera between the upper limbus and the lower lid margin. Lid retraction is a classic sign of thyroid disease, but occurs in neurologic disorders as well. In addition to observing the lid position at rest, notice the relationships of the lid to the globe during eye movement.
Total unilateral ptosis only occurs with complete third nerve palsy. Mild to moderate unilateral ptosis occurs as part of Horner syndrome, or with partial third nerve palsy. Mild to moderate bilateral ptosis occurs in some neuromuscular disorders, such as myasthenia gravis (MG), muscular dystrophy, or ocular myopathy.
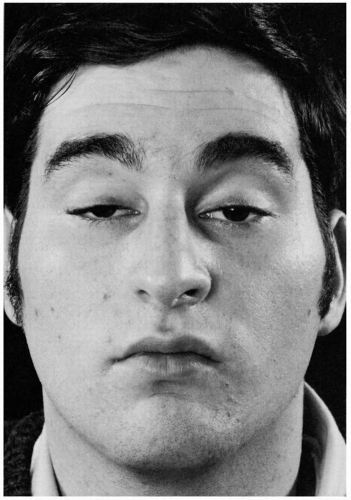
The ptosis in MG is frequently asymmetric and may be unilateral, though it will tend to shift from side to side (Figure 10.3). It characteristically fluctuates from moment to moment and is worsened by prolonged upgaze (fatiguable ptosis). The Cogan lid twitch sign, characteristic of myasthenia, consists of a brief overshoot twitch of lid retraction following sudden return of the eyes to primary position after a period of downgaze. When the ptosis is asymmetric, manually raising the more ptotic lid may cause increased ptosis on the other side (curtain sign, seesaw ptosis). Compensation for mild ptosis on one side may cause the involved eye to appear normal and the other eye to have lid retraction.
Lid Retraction
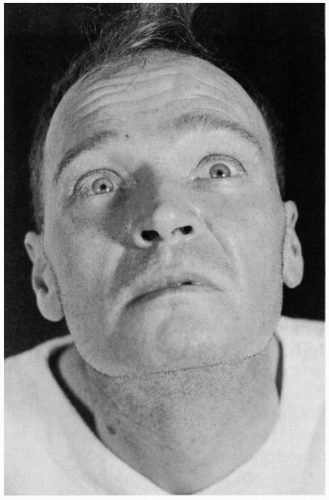
Lid position is abnormal if there is a rim of sclera showing above the limbus, indicating either lid retraction or lid lag. Thyroid eye disease is a common cause of lid abnormalities, including lid retraction in primary gaze and lid lag in downgaze. Lid retraction in primary gaze also occurs with lesions involving the posterior commissure (Collier sign). Lid retraction with posterior commissure lesions is bilateral, but may be asymmetric. With Collier sign, the levators relax appropriately and the lids usually descend normally on downgaze without lagging behind as they do in TED. In addition, the lid retraction may worsen with attempted upgaze (Figure 10.4). Aberrant regeneration of CN III may cause lid retraction on adduction. Lid retraction may also be mechanical, due to trauma or surgery. Lid retraction may be confused with ipsilateral proptosis or contralateral ptosis.
The Pupils
The function of the pupil is to control the amount of light entering the eye, ensuring optimal vision for the lighting conditions. The pupils should be equal in size, round, regular, centered in the iris, and should exhibit specific reflex responses.
Pupillary size depends primarily on the balance between sympathetic and parasympathetic innervation and the level of ambient illumination. The most important determinants are the level of illumination and the point at which the eyes are focused. Accurate measurements are important. Measurements should be made with a pupil gauge or a millimeter ruler; estimates are surprisingly inaccurate. The size of the pupils should be determined at distance in ambient and dim light and at near. The normal pupil is 2 mm to 6 mm in diameter. In ordinary ambient light the pupils are usually 3 mm to 4 mm in diameter. The pupils are small and poorly reactive at birth and in early infancy, becoming normal size around ages 7 to 8. They are normally larger in adolescents and young adults, about 4 mm in diameter and perfectly round. In middle age, they are typically 3.5 mm in diameter and regular, and in old age 3 mm or less and often slightly irregular.
Pupils less than 2 mm in diameter are miotic. Common causes of acquired miosis include old age, hyperopia, alcohol abuse, and drug effects. Neurologically significant causes of miosis include neurosyphilis, diabetes, levodopa therapy, and Horner syndrome. Acute, severe brainstem lesions, such as pontine hematoma, may cause bilaterally tiny, “pinpoint” pupils that still react.
Pupils more than 6 mm in diameter are dilated. Common causes of bilateral mydriasis include anxiety, fear, pain, myopia, and drug effects—especially anticholinergics. Only severe, bilateral lesions of the retina or anterior visual pathways, enough to cause near blindness, will affect the resting pupil size. Neurologically significant bilateral mydriasis occurs in midbrain lesions, in comatose patients following cardiac arrest, in cerebral anoxia, and as a terminal condition.
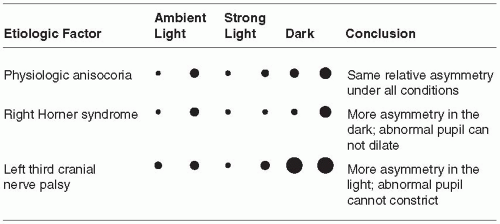
The normal pupil is round, with a smooth, regular outline. Gross abnormalities in shape are usually the result of ocular disease such as iritis or eye surgery. Synechia, a congenital coloboma (a gap in the iris), prior trauma, or iridectomy may all cause pupil irregularity. A slight change in shape, however, such as an oval pupil, slight irregularity in outline, serration of the border, or slight notching, may be significant in the diagnosis of neurologic disease. The pupils are generally of equal size. A difference of 0.25 mm in pupil size is noticeable, and a difference of 2 mm is considered significant. Physiologic anisocoria, mild degrees of inequality with less than 1 mm of difference between the two sides, occurs in 15% to 20% of normal individuals. With such physiologic anisocoria, the degree of inequality remains about the same in light and dark, and the pupils react normally to all stimuli and to instilled drugs (Figure 10.5). Unequal pupils may be caused by primary eye disorders, such as iritis. Unilateral mydriasis is never due to isolated, unilateral visual loss. The reactivity of the normal eye and the consensual light reflex will ensure pupil size remains equal.
The Pupillary Reflexes
The principal pupillary reflex responses assessed on examination are the light response and the near response (“accommodation”). The normal pupil constricts promptly in response to light.
Pupillary constriction also occurs as part of the near response, along with convergence and rounding up of the lens for efficient near vision. Normally, the light and near responses are of the same magnitude.
Pupillary constriction also occurs as part of the near response, along with convergence and rounding up of the lens for efficient near vision. Normally, the light and near responses are of the same magnitude.
The Light Reflex
The light reflex should be tested in each eye individually. The examining light should be shone into the eye obliquely with the patient fixing at distance to avoid eliciting a confounding near response. A common error in pupil examination is to have the patient fixing at near, as by instructing her to look at the examiner’s nose. This technique provides both a light stimulus and a near stimulus simultaneously, and the pupils may well constrict to the near target of the examiner’s nose even when the reaction to light is impaired or absent. Using this technique, the examiner would invariably miss light-near dissociation. Always have the patient fix at a distance when checking the pupillary light reaction. The normal pupillary light reflex is brisk constriction followed by slight dilatation back to an intermediate state (pupillary escape). The responses may be noted as prompt, sluggish, or absent, graded from 0 to 4+, or measured and recorded numerically (e.g., 4 mm → 2 mm.) In comatose patients, it is often important, but difficult, to see if the pupillary light reaction is preserved, especially if there is a question of brain death. A useful technique is to use the ophthalmoscope: focus on the pupil with high positive magnification, dim the ophthalmoscope, and then rapidly reilluminate. Even a small residual reaction may be seen.
The Accommodation Reflex
The accommodation or near reflex is elicited by having the patient relax accommodation by gazing into the distance, then shifting gaze to some near object. The best near object is the patient’s own finger or thumb. The response consists of thickening of the lens (accommodation), convergence of the eyes, and miosis. The pupils constrict at near to increase the depth of focus. The midbrain mechanisms for pupillary constriction to near are separate from those for the light reflex; one response may be abnormal while the other is preserved.
Effects of Drugs on the Pupil
Many systemically acting as well as locally acting drugs may influence pupil size and reactivity. An abnormal pupil may fail to respond appropriately, or respond excessively because of denervation supersensitivity. Sympathomimetics and anticholinergics cause pupillary dilation, and parasympathomimetics or sympathetic blockers cause pupillary constriction. Agents that cause mydriasis include the anticholinergics atropine, homatropine, and scopolamine and the sympathomimetics epinephrine,
norepinephrine, phenylephrine, hydroxyamphetamine, and cocaine. Agents that cause miosis include the cholinomimetics pilocarpine, methacholine, muscarine, and opiates, and the cholinesterase inhibitors physostigmine and neostigmine. Pupillary pharmacology can be applied in the neurologic examination, primarily in the evaluation of Horner syndrome and Adie pupil (see Table 10.1).
norepinephrine, phenylephrine, hydroxyamphetamine, and cocaine. Agents that cause miosis include the cholinomimetics pilocarpine, methacholine, muscarine, and opiates, and the cholinesterase inhibitors physostigmine and neostigmine. Pupillary pharmacology can be applied in the neurologic examination, primarily in the evaluation of Horner syndrome and Adie pupil (see Table 10.1).
TABLE 10.1 Summary of Pharmacologic Pupillary Testing for Horner Syndrome | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Disorders of the Pupil
Pupils can be abnormal for numerous reasons. Common problems include pupils that are too large or too small, unilaterally or bilaterally, or pupils that fail to demonstrate normal reflex responses.
The two conditions most commonly causing a unilaterally large pupil are third cranial nerve palsy and Adie tonic pupil. In CN III palsy, the large pupil has impaired reactions to light and to near; abnormalities of extraocular movement and eyelid position generally betray the origin of the abnormal pupil. With total CN III palsy there is complete ptosis; lifting the eyelid reveals the eye resting in a down and out position (Figure 10.1). Although CN III palsies often affect the pupil more than other functions, some ptosis and ophthalmoparesis is usually present. Since the pupillary parasympathetics occupy a position on the dorsomedial periphery of the nerve as it exits the brainstem, compressive lesions such as aneurysms generally affect the pupil prominently. Ischemic lesions tend to affect the interior of the nerve and spare the pupil, as in diabetic third nerve palsies, because the periphery of the nerve has a better vascular supply. This rule is not absolute. The pupil is usually involved early and prominently with third nerve compression due to uncal herniation (Hutchinson pupil).
The patient presenting with Adie tonic pupil is typically a young woman who suddenly notes a unilaterally enlarged pupil, with no other symptoms. The pupillary reaction to light may appear absent, although prolonged illumination may provoke a slow constriction. The reaction to near, although slow, is better preserved. Once constricted, the tonic pupil redilates very slowly when illumination is removed or the patient looks back at distance, often causing a transient reversal of the anisocoria. Adie syndrome is the association of the pupil abnormality with depressed or absent deep tendon reflexes, particularly in the lower extremities.
The term “tectal pupils” refers to the large pupils with light near dissociation sometimes seen when lesions affect the upper midbrain. Such pupils may accompany the impaired upgaze and convergence/retraction nystagmus of Parinaud syndrome. The variably dilated, fixed pupils reflecting midbrain dysfunction in a comatose patient carry a bleak prognosis. Acute angle closure glaucoma can cause severe frontotemporal headache and a dilated, poorly reactive pupil. Deliberately or accidentally instilled mydriatics will produce a dilated, fixed pupil.
Small pupils occur for many reasons. The pupils in the elderly are normally smaller. Many systemic drugs, such as opiates, may symmetrically shrink the pupils. Important neurologic conditions causing an abnormally small pupil include Horner syndrome and neurosyphilis.
Horner Syndrome
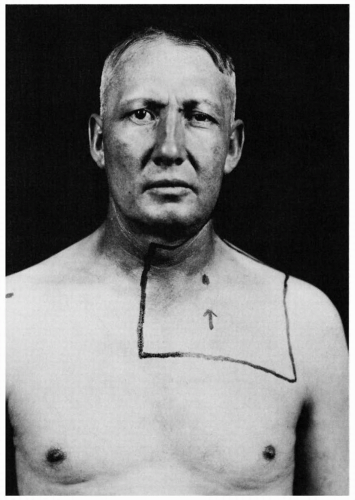
In Horner syndrome, sympathetic dysfunction produces ptosis, miosis, and anhidrosis. Lack of sympathetic input to the accessory lid retractors results in ptosis and apparent enophthalmos. The ptosis of the upper lid is only 1 mm to 3 mm, never as severe as with a complete CN III palsy, although it
may simulate partial third nerve palsy. The ptosis can be subtle and is often missed. The lower lid is frequently elevated 1 mm to 2 mm because of loss of the action of the lower lid accessory retractor that holds the lid down (inverse ptosis). The resulting narrowing of the palpebral fissure causes apparent enophthalmos. Since the fibers mediating facial sweating travel up the external carotid, lesions distal to the carotid bifurcation produce no facial anhidrosis except for perhaps a small area of medial forehead that is innervated by sympathetic fibers traveling with the internal carotid.
may simulate partial third nerve palsy. The ptosis can be subtle and is often missed. The lower lid is frequently elevated 1 mm to 2 mm because of loss of the action of the lower lid accessory retractor that holds the lid down (inverse ptosis). The resulting narrowing of the palpebral fissure causes apparent enophthalmos. Since the fibers mediating facial sweating travel up the external carotid, lesions distal to the carotid bifurcation produce no facial anhidrosis except for perhaps a small area of medial forehead that is innervated by sympathetic fibers traveling with the internal carotid.
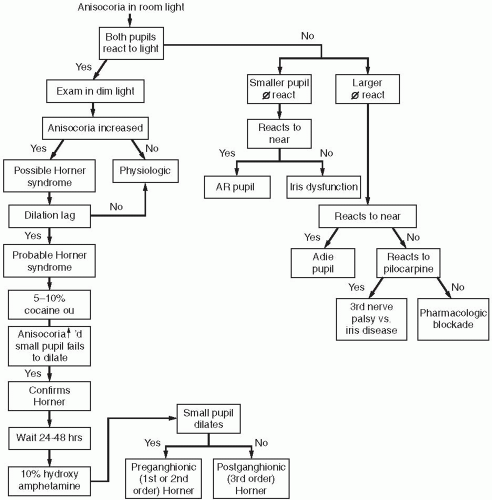
The small pupil in Horner syndrome dilates poorly in the dark. Pupillary asymmetry greater in the dark than in the light generally means Horner syndrome. Recall that physiologic anisocoria produces about the same degree of pupillary asymmetry in the light and dark. In contrast, third nerve palsy and Adie pupil cause greater asymmetry in the light because of the involved pupil’s inability to constrict. Examining the eyes under light and dark conditions can help greatly in sorting out asymmetric pupils (Figure 10.5 and Figure 10.6). Should the examiner err by having the patient fixate at near during testing, the pupillary constriction in the good eye may lessen the asymmetry and cause the abnormal pupil to be missed. The pupil in Horner syndrome not only dilates less fully, it dilates less rapidly. In the first few seconds after dimming the lights, the slowness of dilation of the affected pupil may cause the anisocoria to be even more pronounced (dilation lag). There is more anisocoria at 4 to 5 seconds after lights out than at 10 to 12 seconds.
The causes of Horner syndrome are legion and include the following: brainstem lesions (especially of the lateral medulla), cluster headache, internal carotid artery thrombosis or dissection, cavernous sinus disease, apical lung tumors, neck trauma, and other conditions (Figure 10.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree