Chapter 11 The pelvis
The pelvis (literally ‘basin’) ‘is massive because its primary function is to withstand compression and other forces due to body weight and powerful musculature…’ (Gray’s anatomy 1995).
A partial list of pelvic differences related to gender includes the following.
• The pelvic cavity is longer and more cone shaped in the male and shorter and more cylindrical in the female.
• The male pelvis has a heavier architecture for attachment of larger muscle groups.
• The male iliac crest is more rugged and more medially inclined anteriorly. The female ilia are more vertically inclined, but do not ascend as far as in the male, making the iliac fossae shallower. This probably accounts for the greater prominence of the hips in females (Gray’s anatomy 2005, p. 1431).
• The female sacral base and sacrum as a whole are broader than in the male.
• The male acetabulum is larger than in the female.
• In females the pubis, which forms the anterior pelvic wall, has a lower height than the male.
Different pelvic types
Gray’s anatomy (2005) suggests that there are four major classifications of pelvic types. Differences are greater at the inferior aperture than at the brim (crest).
• Anthropoid (males only): which is common in males and has a typical deep, fairly narrow, pelvic bowl.
• Android (common in both males and females): which is an intermediate design, somewhere between the anthropoid and gynaecoid.
• Gynaecoid (females only): characterized by a wide and shallow pelvic bowl.
• Platypelloid (rare): which has an even wider and shallower pelvic bowl than the gynaecoid.
Pelvic architecture
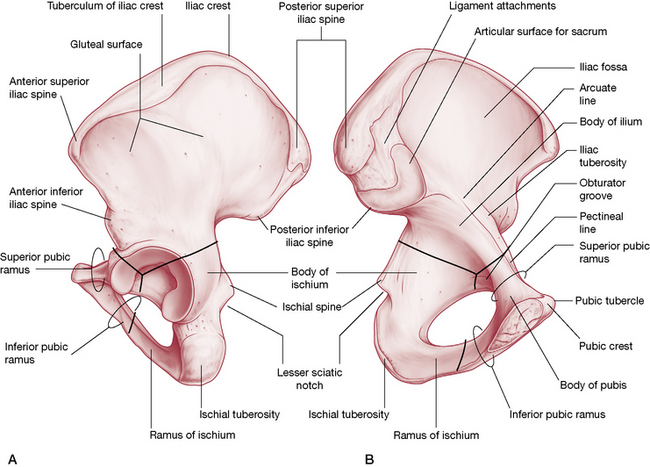
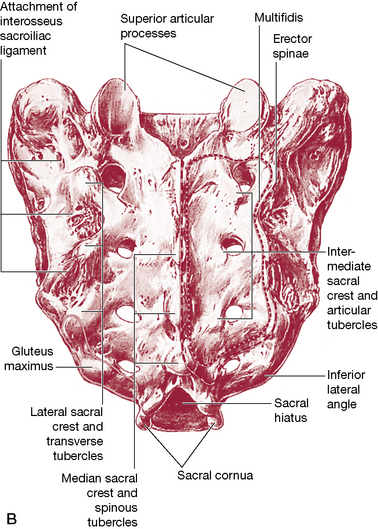
The pelvis is composed of two innominate bones (each made up of an ilium, ischium and pubis), with the sacrum wedged between the ilia posteriorly. The ilium, ischium and pubis have cartilaginous connections in the young but fuse to become one bone by adult life. (Fig. 11.1A/B)
The pelvic girdle or ring
• two innominate bones (literal meaning: ‘nameless’), which are formed from the ilia, ischia and pubic bones. These three bones have cartilaginous connections that fuse to become one bone by adult life
• the sacrum, which wedges between the ilia
• the coccyx, which comprises one or two bones and which attaches to the sacrum, is formed from four fused rudimentary vertebrae
• a multitude of ligamentous structures that bind much of the pelvis together
• Lee (2004) includes the two femoral bones as part of the pelvic structure.
The main function of the pelvic girdle is to offer a linkage mechanism between the upper body and the lower limbs for locomotion; however, it also provides support for the abdomen and pelvic organs (Gray’s anatomy 2005, p. 1430). Expandability of the pelvis during gestation and childbirth is augmented by hormonal involvements that allow relaxation of supporting ligaments and therefore gradual and significant structural distortion.
Pregnancy and the pelvis
The ligaments of the pelvis relax during pregnancy, making the joints they serve flexible for expansion and often creating instability in the process. The relaxation of previously stable structures increases the potential for dysfunction and Gray’s anatomy (2005, p. 1439) reports that:
Note: Form and force closure mechanisms for the SI joint are discussed fully later in this chapter.
Levangie & Norkin (2005) discuss the influences of relaxin, a hormone produced during pregnancy that is thought to activate the collagenolytic system. This system alters the ground substance by increasing its water content and decreasing viscosity and also regulates new collagen formation.
Cyriax (1982) states that relaxin is present for up to 3 months after pregnancy. In the authors’ opinion, this is the ideal time to assess and deal with possible displacement of the pelvic bones that may have occurred as a result of pregnancy and/or labor. If possible, correction of such situations should take place before the depletion of relaxin firms the ligaments with the bones in inappropriate positions.
Lee (2004) reports that:
The innominates
As mentioned previously, each innominate is formed from three component bones, the ilium, ischium and pubic bone, and these elements can be described individually (Figs. 11.2 A/B).
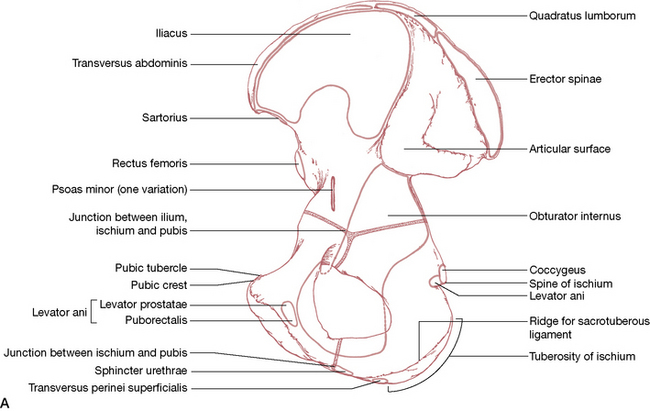
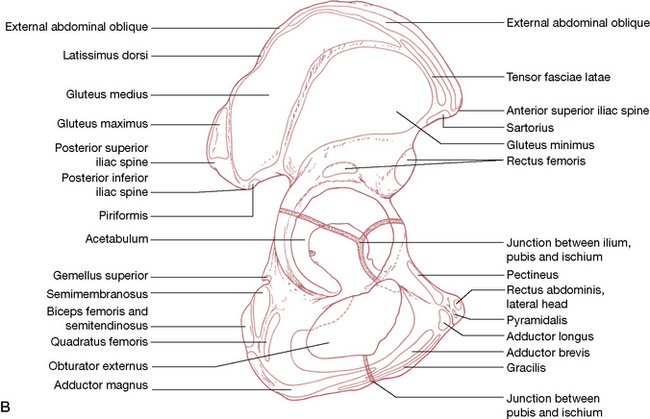
Figure 11.2 Muscle attachments of pelvis A: Medial (internal) view B: Lateral (external) view
(reproduced with permission from Gray’s anatomy 1995).
The ilium (Fig. 11.3)
• A fan-shaped crest is ‘sinuously curved’ (Gray’s anatomy 2005) as it connects the anterior superior iliac spine (ASIS) with the posterior superior iliac spine (PSIS – which is easily palpated beneath the ‘dimpled’ area approximately 4 cm lateral to the second sacral spine) (Fig. 11.4).
• The ASIS is palpable at the lateral end of the inguinal fold.
• The lateral part of the ilium forms the superior aspect of the acetabulum, which hosts the head of the femur.
• Inferior to the PSIS is the posterior inferior iliac spine (PIIS), which lies just posterior to the articular surface of the sacroiliac (SI) joint.
• The articular surface, which forms the ilial portion of the SI joint, is L-shaped and is found on the posterosuperior aspect of the medial surface of each ilium (Fig. 11.5).
• The L-shaped articular surface has a long arm that runs anteroposteriorly and a short arm that runs inferosuperiorly.
• A number of important muscles and ligaments attach to the ilium including quadratus lumborum, erector spinae, iliacus, transversus abdominis, rectus femoris, gluteus minimus, medius and maximus, sartorius, tensor fasciae latae, obliquus abdominis externus and internus, latissimus dorsi and piriformis –see Figs 11.2A/B.
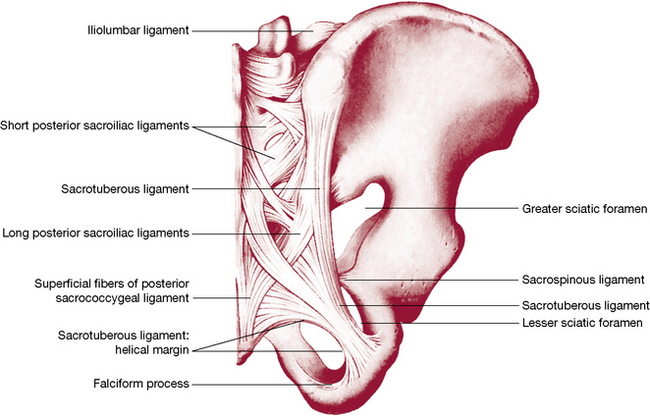
Figure 11.4 Joints and ligaments on the posterior aspect of the right half of the pelvis and 5th lumbar vertebra
(reproduced with permission from Gray’s anatomy 1995).
The ischium
• Each ischium forms one inferoposterior aspect of its respective innominate.
• Anterior to the border of the ischium is the obturator foramen.
• A tuberosity projecting from the body of the ischium (‘sit bone’) takes the weight of the upper body in sitting.
• The superior part of the body of the ischium forms the floor of the acetabulum as well as a portion of the posterior part of the articular surface of the hip joint.
• A projection (ramus) anteromedially from the lower aspect of the body of the ischium meets the inferior ramus of the pubis.
• There are a number of powerful muscular attachments to the ischium, most notably the hamstrings (biceps femoris, semimembranosus and semitendinosus) as well as quadratus femoris, obturator externus and adductor magnus (see Figs 11.2A/B).
Pubic bones
• The anterior aspect of the pelvis is formed by the junction of the two pubic rami at the symphysis pubis.
• The pubis links to the ilium superiorly by means of the superior pubic ramus, which makes up the anterior portion of the acetabulum.
• The inferior pubic ramus joins the ischium at the obturator foramen’s medial aspect.
• A great many muscular attachments including gracilis, adductors longus and brevis, pectineus and rectus abdominis (lateral head) are connected to the pubis (see 11.2A/B).
The symphysis pubis
• The junction of the two pubic bones is fibrocartilaginous, joined by the superior and the arcuate pubic ligaments.
• An interpubic disc connects the medial surfaces of the pubic bones.
According to Gray’s anatomy (2005): ‘Angulation, rotation and displacement are possible but slight…Some separation is said to occur late in gestation and during childbirth’. Despite Gray’s suggesting that ‘possible but slight’ displacement can occur at the symphysis, osteopathic and chiropractic clinical experience contradicts this apparent minimizing of the potential for pubic dysfunction. Pubic dysfunction patterns, and suggested treatments, are described on p. 334 (Greenman 1996, Ward 1997).
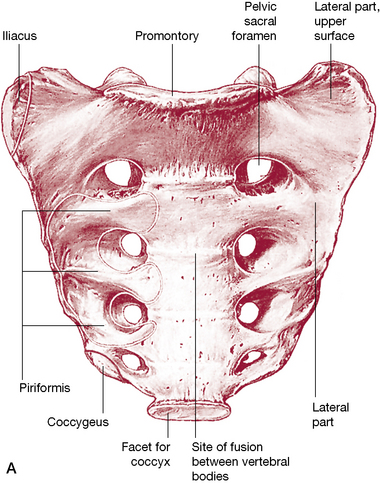
The sacrum (Figs. 11.6 A/B)
• The female sacrum is shorter and wider than the male’s, as a rule (as is the pelvic cavity – see notes on pelvic classifications on p. 301).
• The sacrum, a triangular fusion of five vertebrae, is wedged between the innominate bones to form the posterosuperior wall of the pelvic bowl.
• The caudal end of the sacrum (the apex) articulates with the coccyx while the flat cephalad aspect (the base) articulates with the 5th lumbar vertebrae at the sacrovertebral angle.
• The dorsal surface of the sacrum is convex and the ventral surface concave.
• The sacral base is wide transversely with an anteriorly projecting edge, the sacral promontory.
• The sacral foramen is triangular in shape and caudally is known as the sacral hiatus.
• The superior, concave-shaped, articular processes of the sacrum project cephalad, articulating with the inferior articular processes of the 5th lumbar vertebra.
• Modified transverse processes and costal elements fuse together, and to the rest of the modified vertebral structure, to form the sacral ala or lateral mass.
• The ventral surface of the sacrum is usually vertically and transversely concave.
• The four pairs of sacral foramina have access to the sacral canal via intervertebral foramina, through which the ventral rami of the upper four sacral nerves pass on the ventral surface.
• Lateral to the foramina, costal elements merge and, together with the transverse processes (also known as the costal elements), form the lateral aspect of the sacrum.
• The dorsal surface of the sacrum has a sacral ‘crest’ with either three or four spinal tubercles, formed from fused sacral spines.
• Inferior to the lowest spinal tubercle is the sacral hiatus formed by the failure of the 5th sacral segment’s laminae to meet medially, so exposing the dorsal surface of the 5th sacral vertebral body.
• Fused laminae lie alongside the sacral tubercles and lateral to these are the dorsal sacral foramina (which lead to the sacral canal) through which run the dorsal rami of the sacral spinal nerves.
• Medial to the foramina runs the intermediate sacral crest, composed of fused sacral articular processes, the lowest pair (5th) of which is not fused and projects caudally to form the sacral cornua on each side of the sacral hiatus.
• The sacral cornua links with the coccygeal cornua by means of the intercornual ligaments.
• The lateral surface of the sacrum is formed from fusion of the vertebral transverse processes and costal elements.
• The inferior half of the lateral surface is L-shaped and broad (auricular surface) and articulates with the ilium (see p. 311, sacroiliac joint).
• Posterior to the auricular surface is a rough area where ligamentous attachments occur (see later in this chapter).
• The sacral apex is formed from the inferior aspect of the 5th sacral vertebral body and has an oval facet that articulates with the coccyx.
• The sacral canal, as discussed, forms from fused sacral vertebral foramina, with the upper aspect of its triangular opening pointing cranially when the individual is in a standing position.
• The cauda equina, the filum terminale and the spinal meninges run through the sacral canal.
• The lateral walls of the canal open to the sacral vertebral foramina while inferiorly the canal opens at the sacral hiatus.
• The filum terminale (which attaches to the tip of the coccyx) exits from the sacral hiatus (as do the 5th sacral spinal nerves).
• Attaching to the ventral and dorsal surfaces of the first vertebral sacral body are terminal fibers of anterior and posterior longitudinal ligaments. The lowest pair of ligamentum flava attach to the upper laminar borders.
• The ala or lateral mass is smooth superiorly (covered by psoas major) and laterally rough where the iliolumbar ligament attaches. Iliacus attaches to the anterolateral aspect of this area.
• The sacrum’s pelvic surface provides attachments for piriformis muscles.
• Running anterior to piriformis, having emerged from the pelvic foramina, are the first three sacral ventral rami.
• The sympathetic trunks and the median sacral vessels descend medial to the foramina, directly in contact with bony surfaces.
• Lateral sacral vessels descend lateral to the foramina, also in touch with the bony surface.
• The ventral surface of the upper sacral segments is covered by parietal peritoneum and is crossed by the attachment of the sigmoid mesocolon.
• The rectum is directly in contact with the pelvic surfaces of the 3rd, 4th and 5th sacral vertebrae.
• Erector spinae attach to the dorsal sacral surface, overlying multifidus, which also attaches to the sacrum.
• The upper three sacral spinal dorsal rami penetrate these muscles as they emerge from the dorsal foramina.
• The auricular surface is covered by cartilage and has elevations cranially and caudally. Posterior to the auricular surface are depressions and roughened attachment sites for interosseous sacroiliac ligaments.
• Inferior to the auricular surface are a cluster of attachment sites for gluteus maximus and coccygeus as well as the sacrotuberous and sacrospinous ligaments.
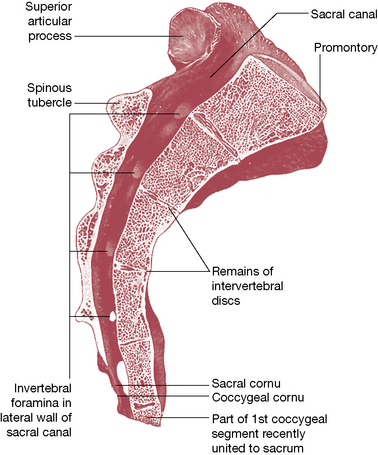
Figure 11.7 Median sagittal section through the sacrum
(reproduced with permission from Gray’s anatomy 1995).
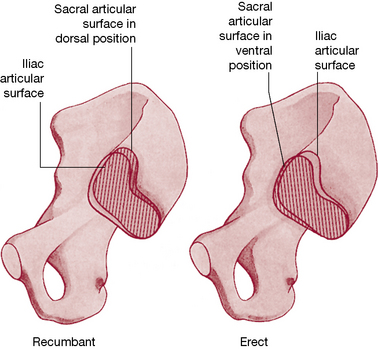
Nutation
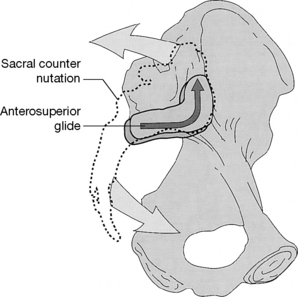
Bilateral sacral nutation and counternutation movements occur around a coronal axis within the interosseous ligament. Unilateral sacral nutation takes place when the lower extremity is extended. There is also a constant degree of alternating (muscularly) ‘braced’ nutation in the standing position (Dorman 1997). Some muscular influences on sacroiliac function are discussed later in this chapter.
Figures 11.8 and 11.9 illustrate clearly the way in which the SI joint allows a gliding action of the sacrum to occur inferiorly (caudally) along the short arm and posteriorly along the long arm of the joint during nutation; during counternutation the sacrum glides anteriorly on the long-arm surface and superiorly (cephalad) along the short arm. The total degree of movement that occurs in either nutation or counternutation does not exceed 2 mm, but is palpable (see palpation tests later in this chapter). Snijders et al (1997) report that multifidus and levator ani act as a force couple, to help in control of the sacral nutation/counternutation processes.
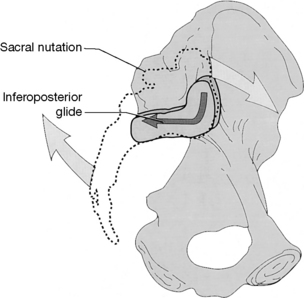
Figure 11.8 When the sacrum nutates, its articular surface glides inferoposteriorly relative to the innominate
(reproduced with permission from Lee 1999).
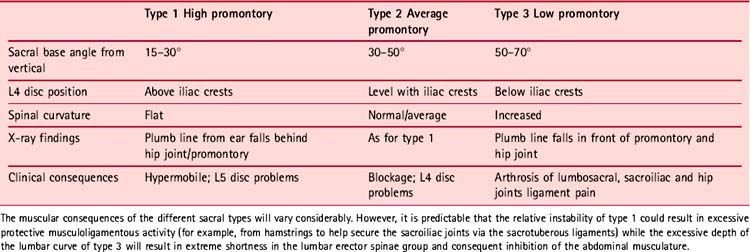
Sacral differences (see Fig. 11.10 and Table 11.1)
Lewit (1985) pays tribute to the early work of Erdmann (1956) and Gutmann (1965) into pelvic biomechanics:
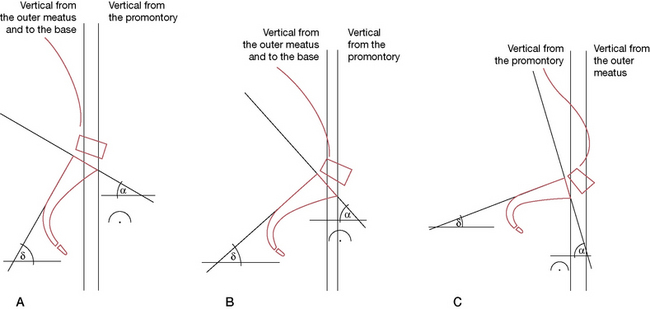
Figure 11.10 Pelvic types showing (A) high promontory, (B) average type, (C) increased pelvic (sacral) inclination
(adapted from Manipulative Therapy in Rehabilitation of the Locomotor System by K Lewit. Reprinted by permission of Elsevier Science Limited).
The coccyx
• The coccyx is composed of three, four (most commonly) or five fused, rudimentary vertebrae. The first coccygeal vertebral body forms its upper surface, or base, and articulates via an oval facet with the sacral apex.
• Dorsolaterally to the facet lie two coccygeal cornua, which articulate with the sacral cornua superiorly.
• A thin, fibrocartilagenous disc, somewhat thinner laterally, lies between the surfaces of the coccyx and sacrum.
• Rudimentary transverse processes project superolaterally, which sometimes articulate and sometimes fuse with the inferolateral sacral angle, to complete the 5th sacral foramina.
• The 2nd to 4th coccygeal segments become progressively smaller, described by Gray’s anatomy (2005) as ‘mere fused nodules’.
• The levator ani and coccygeus muscles attach to the pelvic surface laterally.
• The ventral sacrococcygeal ligament attaches ventrally to the 1st and sometimes 2nd coccygeal bodies, as well as to the cornua.
• Between the 5th sacral body and the cornua an intervertebral foramen allows passage of the 5th sacral spinal nerve.
• The dorsal surface of the coccyx has attachments for gluteus maximus, sphincter ani externus (at the very tip) and the deep and superficial dorsal sacrococcygeal ligaments.
• The filum terminale lies between the deep and superficial dorsal sacrococcygeal ligaments, merges with them and to the dorsum of the 1st coccygeal segment. This filament therefore represents a direct attachment of the meninges of the brain, via the spinal dura, to the coccyx. Goodheart (1985) has described a positional release method involving the coccyx and the filum terminale. The objectives include easing spinal and pelvic dysfunctions relating to hypothesized dural restrictions (see Box 11.1).
Box 11.1 Goodheart’s filum terminale (coccygeal) lift technique
Goodheart (1985) has described a method that seems to rely on the crowding, or slackening, of spinal, dural tissues with the coccyx being used as the means of achieving this. Good clinical results in terms of improved function and release of hypertonicity in local areas, as well as those some distance from the point of application, are claimed. Goodheart’s term for this is a ‘filum terminale cephalad lift’.
Goodheart (1985) and Walther (1988) report that there is frequently a dramatic lengthening of the spinal column after application of this coccygeal lift procedure, with Goodheart mentioning specifically that, in good health, there should be no difference greater than about 1 inch in the measured length of the spinal column sitting, standing and lying, using a tapeless measure, which is rolled along the length of the spine.
Goodheart (1984) states:
Improvements in pelvic, spinal and cervical function have been reported (Goodheart 1985, Walther 1988) following use of the coccygeal lift.
Method
• The patient is sidelying and an area of particular sensitivity to pressure is located in the cervical spinal area.
• The patient uses his own digital pressure to monitor the pain once the practitioner has identified it. A score of ‘10’ is ascribed to the tender point and the objective is for this to reduce by at least 70% during the procedure.
• The practitioner stands at upper thigh level, behind the sidelying patient, facing the side of the table.
• Using the lateral aspect of her cephalad hand (which should be relaxed and not tense throughout the procedure) she achieves contact along the length of the coccyx as she tucks her cephalad elbow against her hip/abdomen area.
• The force required to move the coccyx toward the head is applied by the practitioner leaning into the hand contact, not by any arm or hand effort.
• This application of pressure is not a push on the coccyx but a slowly applied easing of it toward the head and should cause no pain in the coccygeal region if introduced gently but firmly.
• Simultaneously the caudad hand holds the ASIS area in order to stabilize the anterior pelvis and so be able to introduce fine tuning of its position during the ‘lift’, in order to reduce the reported sensitivity score.
• As in positional release methods, the patient reports on the changes in palpated pain levels until a 70% reduction is achieved.
• This position is held for 90 seconds after which reevaluation of dysfunctional structures is performed.
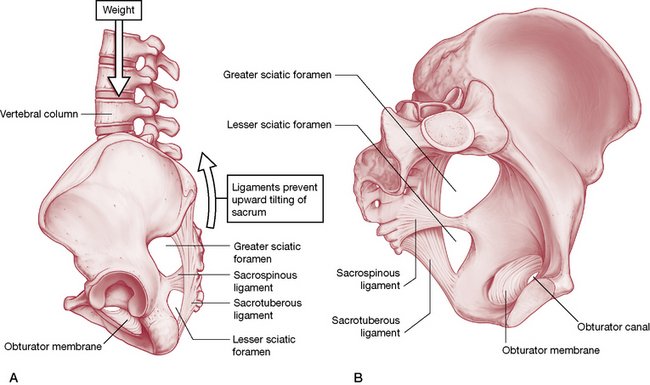
Ligaments of the pelvis
The ventral (or anterior) SI ligament
This forms from an anteroinferior capsular thickening, which is most developed near the arcuate line and the PIIS, from where it connects the 3rd sacral segment to the lateral surface of the peri-auricular sulcus. Bogduk (2005) suggests that it both helps to bind the ilium to the sacrum and prevents anterior diastasis (slippage, separation) of the joint.
The interosseous SI ligament
This vast connection is the main bonding structure between the sacrum and the ilium, filling much of the space posterosuperior to the joint. Covering it superficially is the dorsal SI ligament (below). Gray’s anatomy (2005, p. 1439) describes this as ‘the major bond between the [sacrum and ilia], filling the irregular space posterior superior to the joint’. It is the largest typical syndesmosis in the body (a syndesmosis is a fibrous articulation in which the bony surfaces are held together by interosseous ligaments). Bogduk (2005) regards this structure as ‘the most important ligament of the sacroiliac joint’, the main function of which is to bind the ilium strongly to the sacrum.
The dorsal (or posterior) SI ligament
This covers the interosseous ligament, with the dorsal rami of the sacral spinal nerves and blood vessels lying between them. There are short and long fibers that link the lateral sacral crests to the PSIS and internal aspect of the iliac crest. The short posterior SI ligament helps to stabilize, as well as to prevent posterior flaring of, the joint. Additionally there are inferior posterior fibers that link the 3rd and 4th sacral segments to the PSIS. The long posterior SI ligament is continuous laterally with the sacrotuberous ligament (see below) and medially with the thoracolumbar fascia. It has an additional role in reducing the degree of backward rocking (counternutation) of the sacrum on the ilium (Bogduk 2005).
The sacrotuberous ligament
The sacrotuberous ligament is really a vertebropelvic ligament although it has, via its connections, profound influence over the SI joint. Both it and the sacrospinous ligament (see below) reduce the opportunity for the sacrum to tilt (nutate), by holding it firmly to the ischium (Bogduk 2005).
Gray’s (1995, p. 668) notes:
The ligament is penetrated by the coccygeal branches of the inferior gluteal artery, the perforating cutaneous nerve and filaments of the coccygeal plexus (Gray’s anatomy 2005)
The clinical significance of these attachments warrants emphasis. For example, as Van Wingerden et al (1997) state:
Also relevant is the knowledge that an active trigger point in biceps femoris may modify its own tone (Simons et al 1999) and thereby influence SI joint stability (i.e. the muscle would have increased tone but may well be weaker than is appropriate, causing imbalances). This highlights the need for a trigger point search in muscles associated with dysfunctional joints. The eventual course of therapeutic action may or may not involve deactivation of a trigger point in such a setting. See the discussion on trigger points and gluteus weakness on p. 365.
The sciatic foramina
There are two sciatic foramina, the greater and the lesser on each side. The greater sciatic foramen has as its anterosuperior margin the greater sciatic notch, with the sacrotuberous ligament forming its posterior boundary and the ischial spine and sacrospinous ligament providing its inferior borders. The piriformis muscle passes through it as do the superior gluteal vessels and nerves, which leave the pelvis via this route. Below the piriformis, a number of additional structures exit the pelvis via the greater foramen, including the sciatic nerve (usually), inferior pudendal nerve and vessels, inferior gluteal nerve and vessels, posterior femoral cutaneous nerves and the nerves to obturator internus and quadratus femoris (Heinking et al 1997).
Note: Piriformis is a postural muscle, which will shorten if stressed (Janda 1983). The effect of shortening is to increase its diameter and, because of its location, this allows for direct pressure to be exerted on the sciatic nerve within the foramen, since they pass through it together. After exiting the foramen, the nerve passes under the piriformis in 85% of people. However, in the other 15% the sciatic nerve (or part of it) passes through the muscle so that contraction, spasm, or contractures could produce direct muscular entrapment of the nerve (Beaton & Anson 1938, Te Poorten 1969, Travell & Simons 1992). A diagnosis of piriformis syndrome might be made for either foraminal or muscular belly entrapment (Fig. 11.11).
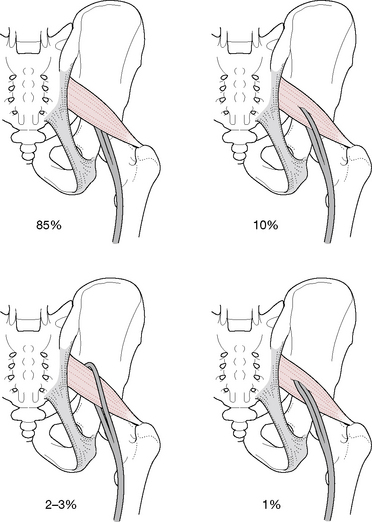
Figure 11.11 Normal and idiosyncratic sciatic nerve positions in relation to the piriformis muscle
(adapted from Ward 1997).
In addition, the pudendal nerve and the blood vessels of the internal iliac artery, as well as common perineal nerves, posterior femoral cutaneous nerve and nerves of the hip rotators, can all be affected in a similar manner (Janda 1996). If the pudendal nerve and blood vessels, which pass through the greater sciatic foramen and reenter the pelvis via the lesser sciatic foramen, are compressed because of piriformis contractures, impaired circulation to the genitalia will occur (in either gender). Since external rotation of the hips is required for coitus by women, pain noted during this act, as well as impotence in men, could relate to impaired circulation induced by piriformis dysfunction within the sciatic foramen.
The next focus of this chapter is the sacroiliac joints – a major source of pain and dysfunction. Before looking at this remarkable structure, we suggest that the subjects of pain in general, and pain as it relates to the pelvis in particular, as discussed in Box 11.2 on p. 317, should be read as the definitions are relevant in the remaining discussions.
Box 11.2 Definitions of pelvic pain
Epidemiology
Female: It is suggested that approximately 15–20% of women, aged 18–50 years, have experienced chronic pelvic pain (CPP) lasting for more than one year (Howard 2003).
Male: A prevalence of 8% chronic prostatitis/chronic pelvic pain syndrome is estimated in the US male population. (Anderson 2008)
In 2002 The International Association for the Study of Pain (IASP) proposed the following definition: ‘Pain is an unpleasant sensory and emotional experience associated with either actual or potential tissue damage, or described in terms of such damage.’ (Merskey & Bogduk 2002)
Pelvic girdle pain (PGP)
The pelvic girdle is considered to be the bony ring formed by the hip bones and the sacrum, to which the lower limbs are attached. A definition has been proposed of pelvic girdle pain (and dysfunction), that aims to distinguish this from pelvic pain and dysfunction relating to gynecological or urological disorders. (Vleeming et al 2008)
• ‘Pelvic girdle pain (PGP) generally arises in relation to pregnancy, trauma, arthritis and osteoarthritis.
• Pain is experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the SIJ.
• The pain may radiate in the posterior thigh and can also occur in conjunction with/or separately in the symphysis.
• The endurance capacity for standing, walking, and sitting is diminished.
• The diagnosis of PGP can be reached after exclusion of lumbar causes.
• The pain or functional disturbances in relation to PGP must be reproducible by specific clinical tests.’
CPP has been defined as follows (Fall et al 2004):
The American College of Gynecologists, also in 2004, proposed the following definition of CPP:
Noncyclical pain of at least six months’ duration, involving the pelvis, anterior abdominal wall, lower back, and/or buttocks, serious enough to cause disability or to necessitate medical care. (ACOG 2004)
The sacroiliac joint
With age, in both genders, fibrous adhesions and other changes gradually obliterate the joint. ‘In old age the joint may be completely fibrosed and occasionally even ossified’ (Gray’s anatomy 2005, p. 1438). Clinically, these changes are important as radiographic research has demonstrated that even before age 50, 6% of joints show evidence of a degenerative process (Cohen et al 1967).
SI joint movement
A very small amount of anteroposterior rotation occurs around a transverse axis when the trunk is flexed or extended, with the degree of movement increasing during pregnancy. According to Gray’s anatomy (1995):
Bogduk (2005) explains the essential role of the SI joints.
Indeed, the evidence is that when the SI joint fuses, as it does in some people due to age or disease (ankylosing spondylitis, for example), the sacrum does literally crack, especially if weakened by osteoporosis (Lourie 1982). Bogduk (2005) reports:
The current understanding of the SI joint is therefore that it performs stress absorption functions as forces from above or below are transferred into the pelvic mechanism. These forces are partially absorbed into the enormous and powerful ligamentous support which the joint enjoys and partially into the unique mechanical relationship the sacrum has with the ilia, where an osseous locking device allows transfer of forces into the pelvis as a whole. Bogduk (2005) again succinctly summarizes the way in which the functional needs of the SI joint have been accommodated into its design.
These functional needs have been superbly incorporated into the SI joint’s design.
Self-locking mechanisms of the SI joint
Form closure is the state of stability that occurs when the very close-fitting joint surfaces of the SI joint approximate, in order to reduce movement opportunities. The efficiency and degree of form closure will vary with the particular characteristics of the structure (size, shape, age) as well as the level of loading involved. Lee (2004) lists three ways that fit (form) of the sacroiliac joint protect it from shear.
1) the sacrum is wedge-shaped vertically and anterioposteriorly, which allows the innominates to stabilize it
2) the articular cartilage is irregular (not smooth), especially on the ilium
3) a frontal dissection of the SIJ reveals bony extensions covered with cartilage that protrude into the joint.
Force closure refers to the support offered to the SI joint by the ligaments of the area directly, as well as the various sling systems which involve both muscular and ligamentous structures (see discussions within this chapter) (Vleeming et al 2007).
Examples of ‘force closure’ are:
• during anterior rotation of the innominate or during sacral counternutation, the SI joint is stabilized by a tightening of the long dorsal sacroiliac ligament
• during sacral nutation or posterior rotation of the innominate, the SI joint is stabilized by the sacrotuberous and interosseous ligaments.
Motor control and force closure
O’Sullivan & Beales (2007) suggest that the motor control system can become dysfunctional in a variety of ways, leading to maladaptation and pain (see Figure 11.12). Maladaptive changes might then in turn lead to reduced force closure (involving a deficit in motor control) or excessive force closure (involving either a deficit, or an increase in motor activation), resulting in a mechanism for ongoing peripheral pain sensitization and leading to chronic pain that involves the sacroiliac and/or other pelvic structures. Additionally the pelvic floor itself may be involved in such adaptations – with the possibility of chronic pelvic pain (CPP) symptoms emerging (O’Sullivan, 2005).
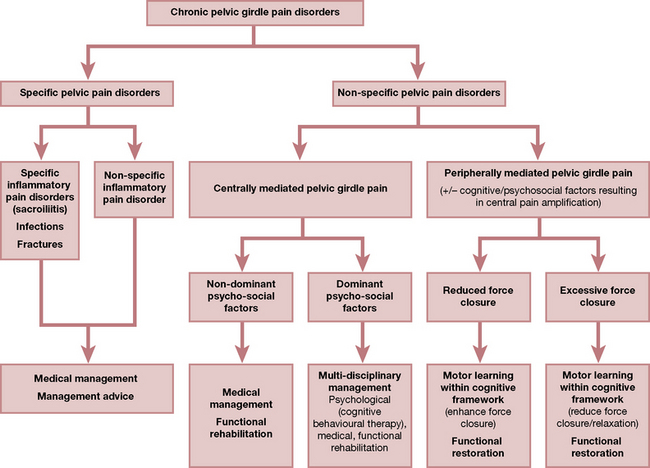
Figure 11.12 The vicious cycle pain from centrally mediated girdle pain.
From O’Sullivan P, Beales D 2007 [pp e4 figure 3] Diagnosis and classification of pelvic girdle pain disorders, Part 2: Illustration of the utility of a classification system via case studies. Manual Therapy 12:e1–e12
Note: See notes toward the end of this chapter on pelvic floor issues.
A summary of muscular involvements in these processes is outlined below.
Innervation of the SI joint
Bogduk (2005) reports that there is little in the way of authoritative evidence to support various contradictory claims as to the precise innervation of the joint. Lee (2004) reports that there is evidence that posteriorly the SI joint is supplied from the posterior rami of the S1 and S2 spinal nerves (Solonen 1957); that the dorsal SI ligaments (and probably the joint) are supplied from lateral divisions of the dorsal rami of L5, S1, S2 and S3 spinal nerves (Bradlay 1985), while the lateral branches of L5, S1 and S2 dorsal rami form a plexus between the interosseous and dorsal sacroiliac ligaments (Grob 1995). There was contradictory research evidence from Solonen and from Grob as to the ventral neural supply to the SI joint, which apparently varied considerably between different individuals. Lee asserts: ‘The wide distribution of innervation is reflected clinically in the variety of pain patterns reported by patients with SI joint dysfunction’.
Muscles and the SI joint
According to Bogduk (2005) there are no muscles that actively move the SI joints; however, a great many muscles attach powerfully on either the sacrum or the ilia and are therefore capable of strongly influencing the functional adequacy of the pelvis as a whole and of SI joints in particular.
Dorman (1997) suggests that: ‘Judging by their attachments, various muscles are probably involved, directly or indirectly, in force closure of the SIJ’. Indirectly muscles can act on ligaments and fascia (see the discussion regarding the influence of the hamstrings on the sacrotuberous ligament on p. 436 and in Chapter 3).
Muscle activity and the SI joint when walking
Dorman (1995) analyzed muscular activity relating to SI function during the gait cycle.
• Erector spinae ‘might be expected to promote nutation’. Dorman (1995) suggests that select subsegments of this group might fire independently when required.
• Gluteus maximus promotes self-locking of the SI joint and controls nutation when the fibers which attach to the sacrotuberous ligament contract. This is clearly a secondary function of gluteus maximus and would only operate in particular postural and nutation positions.
• Gluteus medius has a distinctive role to play in locking the SI joint during the stance phase of the gait cycle. However, Dorman (1997) suggests that it is subject to reflex inhibition when the ilium on the affected side is in an anterior position, at which time tenderness will be noted on deep palpation under the rim of the iliac crest (sidelying).
• Latissimus dorsi joins across the mid-line with the contralateral gluteus maximus via the thoracolumbar fascia and activates during trunk rotation (which occurs during gait). The thoracolumbar fascia can also be tightened by the erector spinae. The effect is to stabilize the SI joint.
• Biceps femoris can change the tension of the sacrotuberous ligament, modulating its tension and influencing the SI joint. This influence varies with body position and the degree of nutation.
Slings, units and systems (Fig. 11.13)
Lee (2004) discusses muscular contributions to the stability of the pelvic structures (as well as the lumbar spine and the hip) and points out that there are two muscular systems involved, a local and a global system.
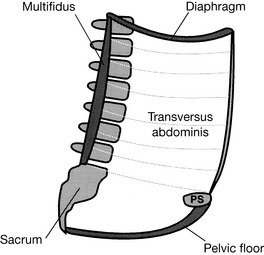
Figure 11.13 The muscles of the inner unit include the multifidus, transversus abdominis, diaphragm and the pelvic floor
(reproduced with permission from Lee 1999).
• the muscles of the pelvic floor (primarily levator ani and coccygeus)
• deep fibers of multifidus and
In the past, four slings (then referred to as systems) were described by Lee (1999) as comprising the second muscle system, these being
• Posterior oblique system (latissimus dorsi, gluteus maximus and the lumbodorsal fascia which links them). When latissimus and contralateral gluteus maximus contract there is a force closure of the posterior aspect of the SI joint.
• Deep longitudinal system (erector spinae, deep laminae of the thoracodorsal fascia, sacrotuberous ligament and biceps femoris). When contraction occurs, biceps femoris influences compression of the SI joint and sacral nutation can be controlled (Van Wingerden et al 1993).
• Anterior oblique system (external and internal obliques, the contralateral adductors of the thigh and the intervening abdominal fascia). The obliques take part in most upper and lower limb as well as trunk movements, with transversus abdominis stabilizing. The obliques act almost constantly in unsupported sitting, although cross-legged posture allows them ‘time-out’ (see the discussion of this phenomenon later in this chapter). Snijders et al (1997) suggest that cross-legged sitting offers stabilization for the SI joint, obviating the need for force closure.
• Lateral system (gluteus medius and minimus and contralateral adductors of the thigh).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree