The Prevention of Adjacent Segment Disease Associated with Cervical Spine Fusion
Saad B. Chaudhary
Thomas E. Mroz
Cervical spondylosis is a progressive degenerative process that can involve only a single motion segment or the entire cervical spine. It is among the most common pathologies seen by a spine surgeon (1). Disk degeneration results in loss of disk height followed by altered facet loading and uncovertebral and facet joint arthrosis. The sum total of these ventral and dorsal processes is often nerve root(s) and/or spinal cord compression. A common method of management for patients who fail to improve with conservative treatment is surgical decompression and stabilization. However, with a variety of ventral and dorsal techniques available, the optimal surgical approach and strategy remains controversial (2, 3, 4 and 5). The surgical plan rests on several factors including the exact nature of the pathology, location of the lesion, the number of spinal segments involved, patient-specific factors, and surgeon preference. Despite the availability of multiple surgical techniques, most spine surgeons prefer the ventral approach (6) due to high patient satisfaction and good to excellent clinical outcomes (7).
Anterior cervical discectomy and fusion (ACDF) was first described by Smith and Robinson (2) and then modified by Cloward (4) in 1958. Since its introduction five decades ago, ACDF has been established as the gold standard treatment for degenerative cervical disk disease resulting in symptomatic root or cord compression. However, long-term follow-up studies after ventral decompression and fusion have revealed that a substantial percentage of patients develop radiographic changes at the adjacent levels, that is, adjacent segment degeneration (Fig. 84.1). Furthermore, a proportion of these patients develop symptoms (i.e., adjacent segment disease) correlative to these radiographic changes. Although this process is detailed extensively in the spine literature, the exact pathogenesis of postarthrodesis adjacent level cervical degeneration is still debated. The etiology for adjacent segment degeneration is probably multifactorial and can be best explained by a combination of the natural progression of cervical spondylosis, the biomechanical changes associated with cervical motion segment fusion, and, possibly, iatrogenic trauma to the adjacent soft tissues during the index surgery. This chapter briefly outlines the causes of adjacent segment degeneration and focuses on surgical concepts and techniques that can minimize and prevent this phenomenon.
ADJACENT SEGMENT DISEASE FOLLOWING ANTERIOR CERVICAL FUSION
Several authors have reported on the radiographic evidence of adjacent segment degeneration following a cervical fusion. The radiographic appearance of this process can vary from ventral and dorsal osteophyte formation to severe disk degeneration, facet hypertrophy, and segmental hypermobility with central and/or foraminal stenosis (Fig. 84.2). Hunter et al., in 1980, provided one of the earliest radiographic delineations of degeneration of the segments cranial and caudal to a prior fusion. In their retrospective review of nine patients with a minimum follow-up of 7 years, nine patients underwent cervical decompression and fusion for nontraumatic reasons and eight developed radiographic evidence of adjacent degeneration. However, no clinical correlation or follow-up was provided in this study (8). Other authors have utilized magnetic resonance imaging to show the degenerative changes at motion segments adjoining prior fusions. Wu et al. provided a shortterm (3-year) follow-up on 68 patients who underwent an anterior cervical decompression and fusion. They compared the MRI findings between the surgical group and 68 control patients. They reported an increased incidence in degenerative changes at immediately adjacent levels of the fusion when compared to the nonoperative controls (9). Similarly, in a very recent MRI study, Matsumoto et al. (10) prospectively reported a 10-year follow-up on
asymptomatic controls and 64 patients who underwent cervical decompression and fusion. They concluded that although both groups display a progression of disk degeneration at 10 years, the surgical group has a significantly higher incidence of adjacent segment deterioration. The incidence of disk degeneration and foraminal stenosis was 15% versus 1% at the cranial level and 22.6% versus 5.5% at the caudal level in the ACDF versus the control group, respectively.
asymptomatic controls and 64 patients who underwent cervical decompression and fusion. They concluded that although both groups display a progression of disk degeneration at 10 years, the surgical group has a significantly higher incidence of adjacent segment deterioration. The incidence of disk degeneration and foraminal stenosis was 15% versus 1% at the cranial level and 22.6% versus 5.5% at the caudal level in the ACDF versus the control group, respectively.
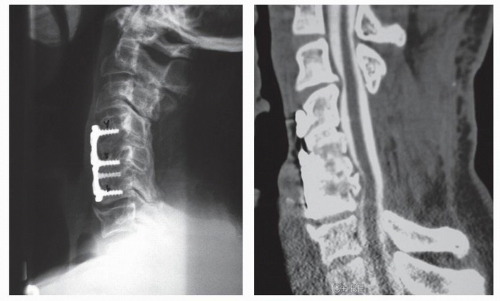 Figure 84.1. Subadjacent level degeneration at C6-C7 greater than at C4-C5 with incomplete decompression at index surgeries. |
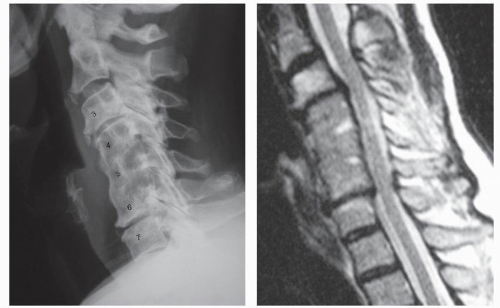 Figure 84.2. A 61-year-old female 7 years s/p C4-C6 discectomy and fusion. Presents with neck pain, early myelopathy, and bilateral C7 radiculopathy due to central and foraminal stenosis. |
It is crucial to distinguish between the radiographic evidence of adjacent segment degeneration and the actual development of associated clinical symptoms. Hilibrand et al. (11) distinguished the two entities into adjacent segment degeneration versus disease. Their definition of adjacent segment disease is the presence of new clinical symptoms that persist for two consecutive follow-up visits after an anterior cervical fusion. In their experience, there is a constant annual incidence of 2.9% for adjacent segment disease. Kaplan-Meier Survivorship analysis predicts that 25.6% of the patients will have symptoms adjacent to a cervical fusion at 10-year follow-up. More importantly, greater than two-thirds of these patients required additional cervical surgery to treat their new symptoms. Several other authors have reported on the incidence of adjacent segment disease and the need for additional surgery at an annual incidence of 1.5% to 4% (12, 13 and 14).
Various biomechanical studies are also available to shed light on the etiology of adjacent segment degeneration (15, 16, 17 and 18). Several of these studies attribute this process to the altered kinematics and added stiffness and strain at the adjacent motion segments. Unfortunately, the exact pathogenesis and the clinical development of disease at the adjacent levels are not yet completely understood. However, it is evident that both biologic and mechanical processes act in conjunction to produce adjacent segment degeneration and disease. The detailed description of altered segmental motion, increased intradiskal pressures, and other biomechanical changes adjacent to a cervical fusion are beyond the scope of this chapter and are better expressed elsewhere in this book (see Chapter 118). The main focus of this chapter is on the prevention of adjacent segment degeneration.
PREVENTION STRATEGIES
SURGICAL DECISION MAKING
The primary step in prevention can be executed by a careful selection of the approach and type of surgery that is appropriate for each patient. Although the primary task of this chapter is to outline prevention strategies against adjacent segment degeneration in fusion surgery, a consideration of adjacent segment degeneration must include an overview on motion-preserving procedures. Cervical radiculopathy and cervical spondylotic myelopathy do not always warrant a fusion surgery. Several nonfusion options are available for treatment, and they include laminoplasty, laminoforaminotomy, laminectomy, ventral uncoforaminotomy and discectomy, and cervical total disk arthroplasty. Cervical radiculopathy in the absence of instability and kyphosis can often times be addressed by a laminoforaminotomy without a fusion. Although Herkowitz and Henderson independently reported a similar annual incidence of adjacent segment degeneration in patients with either a dorsal laminoforaminotomy or an anterior cervical fusion, Clarke reported a significantly reduced risk of adjacent segment degeneration with a dorsal foraminotomy.
Herkowitz et al. studied 44 patients who were randomized to ACDF (n = 28) or dorsal foraminotomy without fusion (n = 16) for the treatment of cervical radiculopathy. After a 4.5-year mean follow-up, they found a 41% prevalence of adjacent segment degeneration in the anterior fusion group and 50% prevalence in the dorsal foraminotomy group (19). Henderson reported a prevalence of adjacent level degeneration of 9% and an average annual incidence of approximately 3% in 846 patients who underwent dorsal foraminotomy without fusion. Seventy-nine of the 846 patients (9%) developed adjacent segment disease requiring additional surgery (20). However, Clarke et al. analyzed 303 patients, using a similar survivorship analysis as Hilibrand, and showed that only 6.7% of patients who had a dorsal cervical foraminotomy would have new disease at an adjacent level within 10 years after the operation. They reported an annual incidence of 0.7% (21).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








