51 The Role of Spinal Fusion and the Aging Spine
Stenosis with Deformity
KEY POINTS
Introduction
Adult scoliosis is a common and sometimes disabling degenerative condition of the spine, with an overall prevalence reported in up to 60% of the elderly population.1 Adult scoliosis has a marked impact on patients’ general medical health and well-being; it has been shown that scoliotic patients have a significantly depressed perception of their mental and physical health in comparison with the general U.S. population. Even when individuals are compared with those having additional comorbidities, the adult scoliosis patients rate lower in clinical health assessment. In addition to the subjective considerations of this progressive disease, severe pain and disability occur in this population.2
Definition of Stenotic Degenerative Disease in Deformity
Neural compression associated with adult lumbar scoliosis is commonly manifested as a radicular pain that may be related to physical activity. As the apex of a curve rotates, there is associated hypertrophy and subluxation of the facet joints in the concavity of the curve. Additionally, collapse in the concavity results in narrowing of a neural foramen between adjacent pedicles. As a result, symptoms occur in the anterior portion of the thigh and leg (resulting from compression of the cephalic and middle lumbar nerve roots). Radiating pain in the posterior portion of the lower extremity is more common on the side of the convexity of the lumbar curve; such pain is due to compression of the caudal lumbar nerve roots and the sacral nerve roots, well caudad to the apex, as the spine curves back to meet the pelvis. 2
Clinical Complex of Symptom Presentation
Neurologic pain occurs with activity-related claudication caused by diminished blood flow to the nerves. It is incumbent upon the healthcare provider to rule out common causes of leg pain such as peripheral vascular disease, cardiac disease, arteriosclerotic vascular disease, and/or primary neurologic disease. Compressive radicular pain occurs on the concave collapsing side of a degenerative scoliosis, from direct compression of the nerve at the exiting foramen or subarticular space. Nerve stretch radicular pain occurs on the convex nerve roots that are exiting from the stenotic collapsing scoliotic spine. Therefore, a patient may present with either convex radicular pain or concave nerve root pain, or both.
Adult Scoliosis Classification
Adult Scoliosis is classified by Aebi 3 using an AO system based on a pathoanatomic etiology and on a temporal onset of deformity. His classification defines adult scoliosis as spinal deformity in a skeletally mature patient with a Cobb angle of more than 10 degrees in the coronal plane. Aebi separates adult scoliosis into four types:
Schwab et al.4 proposed a three-tier classification system for adult scoliosis based on parameters of coronal and sagittal plane. These radiographic criteria include lumbar lordosis, location of coronal curve apex, olisthesis of vertebra segments relative to each other, and sagittal balance on x-ray (Figures 51-3 through 51-6). The classification system has accurately correlated radiographs with clinical significance, in an attempt at suggesting the most appropriate successful treatment in the adult patient. The rate of disease progression is influenced by the magnitude of the curve, the degree of lateral listhesis, the quality of the bone and the severity of associated spondylotic disease. Table 51-1 shows two classification schemes.
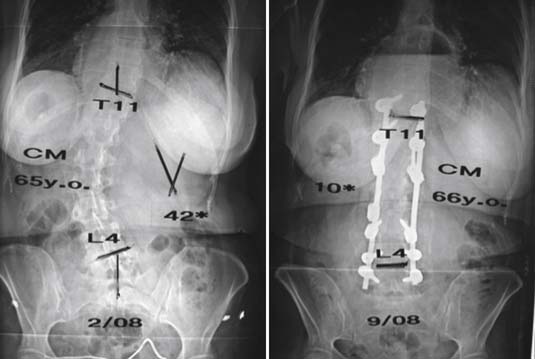
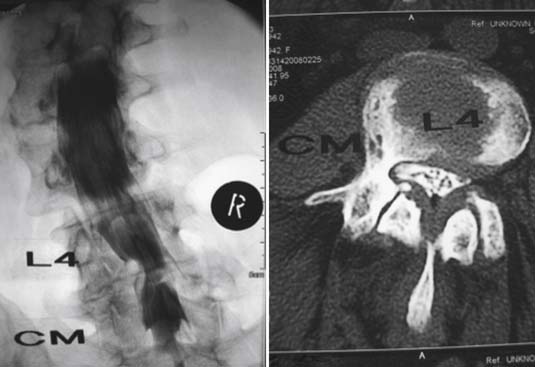
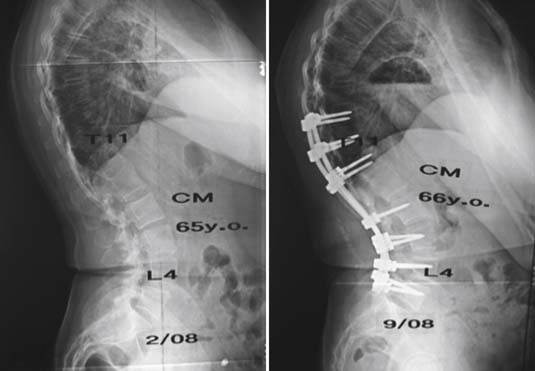
FIGURE 51-3 A 66-year-old female with symptoms of back pain and pseudo-radicular leg pain plus neurogenic claudication. She had an AO (Aebi) type 1 de novo scoliosis curve pattern, also categorized as a Schwab type 5, A+ pattern. After work-up and failure of extended nonoperative treatment, she underwent a posterior multilevel spine decompression /laminectomy and stabilization reconstruction / realignment with fusion and segmental pedicle screw implant instrumentation. Follow-up evaluation demonstrated excellent clinical improvement with resolution of symptoms and an excellent radiographic result, similar to that demonstrated in Figure 51-6.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree