The Unconscious or Confused Patient
BACKGROUND
Level of consciousness: assessment of the unconscious and confused patient
The reticular activating system in the brainstem maintains normal consciousness. Processes that disturb its function will lead to altered consciousness.
This can happen as a result of (Fig. 27.1):
Assessment of patients with altered consciousness will be divided into:
Examination of unconscious patients must:
• distinguish the three syndromes listed above
• attempt to define a cause—frequently requires further investiga- tions.
The terms used to describe levels of unconsciousness—drowsiness, confusion, stuporous, comatose—are part of everyday language and are used in different senses by different observers. It is therefore better to describe the level of consciousness individually in the terms described below. Some issues relating to confusion and delirium are discussed towards the end of the chapter.
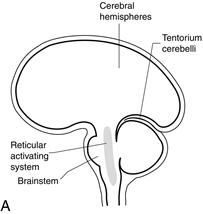

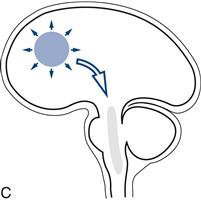
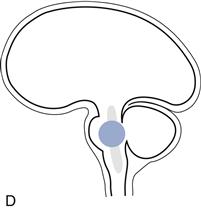
Figure 27.1 Sites of lesions that produce unconsciousness:
A. Key; B. Diffuse encephalopathy; C. Supratentorial lesions; D. Infratentorial lesions
Changes in level of consciousness and associated physical signs are very important and need to be monitored. Always record findings.
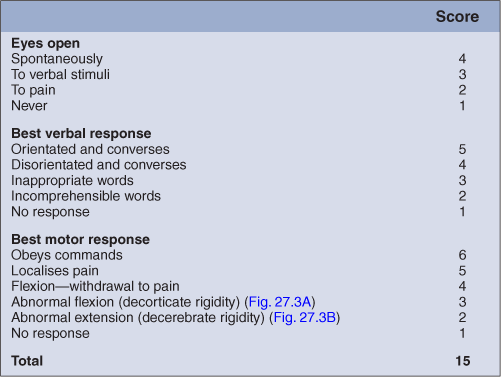
The Glasgow Coma Scale is a quick, simple, reliable method for monitoring level of consciousness. It includes three measures: eye opening, best motor response and best verbal response.
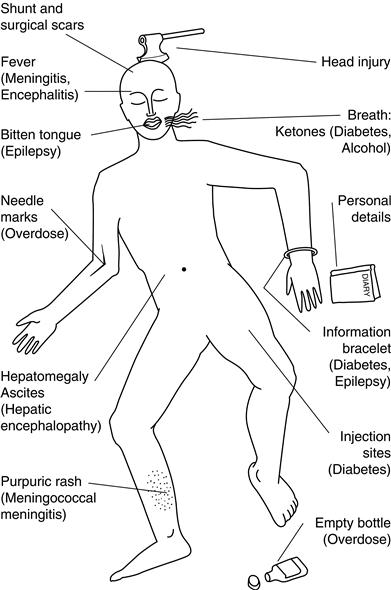
History can be obtained in patients with altered consciousness, from either friends, relatives, bystanders, or nursing or ambulance staff. The clothing (incontinent?), jewellery (alert bracelets/necklaces), wallet and belongings are silent witnesses that may help (Fig. 27.2).
Herniation or coning
Coning is what occurs when part of the brain is forced through a rigid hole, either:
There is a characteristic progression of signs in both types of herniation.
1 Uncal herniation
What happens
A unilateral mass forces the ipsilateral temporal lobe through the tentorium, compressing the ipsilateral third nerve and later the contralateral upper brainstem, and eventually the whole brainstem. Once cerebrospinal fluid (CSF) flow is interrupted, the process is accelerated by an increase in intracranial pressure.
Physical signs
Early:
Later:
Later still:
Progression is usually rapid.
2 Central herniation
What happens
A supratentorial lesion forces the diencephalon (the thalamus and related structures that lie between the upper brainstem and cerebral hemispheres) centrally through the tentorium. This compresses first the upper midbrain, and later the pons and medulla.
Physical signs
Early:
Later:
Later still:
Progression is usually slower.
WHAT TO DO
Resuscitation
Use the Neurological ABC:
N: Neck Always remember there may be a neck injury. If this is possible, do not manipulate the neck.
C: Circulation Check there is adequate circulation; check pulse and blood pressure.
D: Drugs Consider opiate overdose; give naloxone if indicated.
E: Epilepsy Observe for seizures or stigmata, bitten tongue; control seizures.
F: Fever Check for fever, stiff neck, purpuric rash of meningococcal meningitis.
G: Glasgow Coma Scale Assess score out of 15 (Table 27.1). Record subscores (eyes/verbal/motor) as well as total.
H: Herniation Is there evidence of coning? See above, rapid neurosurgical assessment.
N.B. Pulse, BP, respiration rate and pattern, temperature. Monitor Glasgow Coma Scale.
EXAMINATION
This is aimed at:
• finding or excluding focal neurological abnormalities
• looking for evidence of meningism
• determining the level of consciousness and neurological function.
Position and movement
What to do
Look at the patient: often best done from the end of the bed.
If there is movement:

 TIP
TIP