The Use of Cervical Orthoses, Halo Devices, and Traction in Children
Lawson A.B. Copley
John P. Dormans
The orthoses and immobilization techniques used in children demonstrate a spectrum of ability to restrict cervical motion (1, 2, 3, 4, 5, 6, 7 and 8). A particular device may be effective in limiting a particular segment of the cervical spine but relatively ineffective in limiting motion in other cervical regions. The appropriate selection of a cervical immobilization device may allow adequate immobilization for a specific purpose, and this selection should be guided by knowledge of the relative ability of that device to adequately restrict undesirable motion given the underlying pathology. The purpose of this chapter is to categorize and evaluate the effectiveness of currently available forms of cervical immobilization for children and adolescents.
BACKGROUND
An important milestone in the development of cervical immobilization devices was the work of White et al. (9) in the biomechanical analysis of the stability of the cervical spine at Yale in the 1970s. The supplemental work involving radiographic evaluation of cervical motion in multiple planes laid the groundwork for comparative studies of the various forms of cervical immobilization since that time (6,9). Of lasting value were the objective criteria to define clinically significant instability based on injury patterns and specific measurable radiographic features (Fig. 38.1) (9).
CLASSIFICATION OF CERVICAL IMMOBILIZATION DEVICES
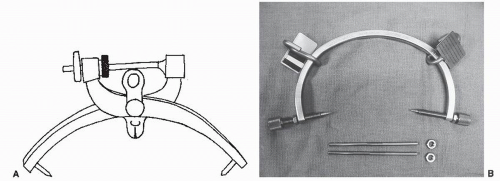
General categories of cervical immobilization devices used in children include cervical orthoses (COs), cervicotho-racic orthoses (CTOs), noninvasive traction devices, invasive traction devices, and halo immobilization. The advent of lightweight plastic materials that can be prefabricated to fit most patients and mass-produced has led to a broad array of devices available through several device manufacturers. For many of these devices, comparison studies have been performed to evaluate their relative efficacy in immobilizing the cervical spine (1, 2, 3, 4, 5, 6, 7 and 8). Some studies assess the closing capillary wedge pressure to indicate the potential risk for decubitus ulcer formation in unconscious patients requiring prolonged immobilization.
Overall, COs are less restrictive than CTOs, and invasive immobilization with a halo ring and vest results in the most reliable restriction. Some studies have shown the comparative efficacy between CTOs and halos in children (8,10,11). CTOs tend to limit motion in the middle and inferior cervical regions well but are less effective in limiting the upper cervical spine. The halo tends to limit motion well in the upper cervical region but allows paradoxic motion in the lower cervical spine and at the cervicothoracic junction (2,4,6). Ultimately, there is a trade-off between the amount of restriction and the increased risk for complications when comparing different devices (12,13).
A variety of off-the-shelf devices are available for pediatric cervical immobilization. However, under some circumstances, particularly when there is body habitus variation or the need to have access to the abdomen for gastrostomy, colostomy, or urinary diversion purposes, a custom-fabricated orthosis may be necessary. Generally, this is more expensive and time-consuming and requires close communication between the treating physicians and a trained orthotist. Another technique that should not be overlooked is the direct application of Minerva or halo casts. This requires experience and capable assistance to ensure that all bony prominences are well padded to avoid pressure breakdown within the cast (11,14).
BIOMECHANICAL CONSIDERATIONS
The cervical spine can be analyzed according to motion segments or anatomic region. The motion of each segment from the occipitocervical junction to the cervicothoracic junction can be evaluated in each of three planes including flexion/extension, right and left lateral bending, and axial rotation. Further consideration may be given to anteroposterior translation or side-to-side translation at each motion segment. This is useful methodology
for biomechanical and radiographic analyses of cervical motion. Also, it is relevant clinically when considering the relative motion or displacement of an injured segment compared to proximal and distal noninjured segments.
for biomechanical and radiographic analyses of cervical motion. Also, it is relevant clinically when considering the relative motion or displacement of an injured segment compared to proximal and distal noninjured segments.
The most relevant work in this area was performed by White et al. (9). They concluded that the normal adult spine should not permit horizontal motion greater than 2.7 mm between vertebrae (3.5 mm with radiographic magnification) or angular displacement greater than 10.7 degrees (commonly rounded to 11 degrees) relative to adjacent vertebrae (9). They also determined that the anterior elements of the spine, comprised of the anterior longitudinal ligament, costotransverse ligaments, annulus fibrosus, vertebral body, and posterior longitudinal ligament, were most useful in stabilizing the spine in extension (9). The cadaveric studies of White et al. (9) illustrated that the spine would be stable in extension until essentially all of the anterior elements were destroyed or unable to function. The posterior spinal elements, comprised of the facet joint capsules, facet joints, ligamentum flavum, and interspinous and supraspinous ligaments, function to stabilize the spine in flexion. White et al. (9) demonstrated that the spine would be stable in flexion until essentially all of the posterior elements were destroyed or unable to function. Although similar research has not been performed in children, this information is nonetheless useful in evaluating cervical instability and integrity in older children (above 8 years of age) and adolescents who demonstrate anatomic features and injury patterns similar to adults.
An organized approach to evaluating cervical spine motion segments by radiographic analysis was introduced by Johnson et al. (6) in 1977. With this methodology, it is possible to objectively compare various cervical immobilization devices with other devices using volunteers with normal cervical spines. Sagittal plane motion is measured on lateral cervical spine films in neutral, maximal flexion, and maximal extension. Lateral bending is measured on anteroposterior films during the extreme of this motion. Rotation is measured using overhead photographs of the head and shoulders. This methodology has been repeated in a number of studies comparing other forms of cervical immobilization that were introduced following Johnson’s initial comparison of the soft cervical collar, Philadelphia collar, sternooccipital mandibular immobilizer (SOMI), four-poster brace, cervicothoracic brace, and halo with plastic body vest (1,2,4, 5, 6, 7 and 8).
Other methods of comparative evaluation of cervical immobilization devices include goniometry and cineradiography. Goniometry has been shown to have a high correlation with radiographic techniques and has the obvious advantage of avoiding radiation exposure (4). However, the precision of this method is limited, and it does not give information on the degrees of motion at individual vertebral levels (4).
Besides segmental motion analysis, another means of evaluating the cervical spine is by anatomic region. This provides a measure by which to assess injury and healing patterns from a clinical perspective. Most clinical outcome studies that compare different forms of treatment of cervical spine injuries divide the spine into anatomic regions, with the upper cervical injuries (occipitocervical, atlas, and axial) separated from subaxial injuries (15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 and 32). Many studies further subdivide the upper cervical injuries based on the specific injury location such as occipitocervical dissociation, Jefferson’s fractures (atlas), odontoid (subtypes I, II, and III), and hangman’s fractures (axis posterior element) (19,21,22,24,26,28,29). It is likely that the biomechanical properties and response to the forces of injury of these different areas are substantially affected by their unique anatomic features. Therefore, such regional anatomic evaluation is useful in predicting the natural history of a specific injury pattern and location with respect to the relative likelihood of successful outcome with conservative immobilization versus surgical intervention.
COMPARISON AND EVALUATION OF NONINVASIVE CERVICAL IMMOBILIZATION DEVICES CERVICAL ORTHOSES (COS)
SYMPTOMATIC SUPPORT COLLARS
A soft collar provides negligible cervical stabilization and has no role in the management of the potentially unstable pediatric spine. In most studies, the restricted motion with soft or hard collars is less than 5% (6,33). This device is used mainly for treatment of minor cervical muscle strains and
mild whiplash injuries. The symptomatic relief provided by the soft collar is thought to result from the warming effect on the underlying soft tissues as well as the support to the weight of the head, which is otherwise balanced by the cervical musculature. This allows the muscles to rest during the period of myofascial inflammation following the injury. Patient compliance is high because of the comfort of the device. Hard collars made with supplemental plastic integrated into the soft support fabric are similar in function to soft collars. They do not add substantially to cervical stabilization (Fig. 38.2).
mild whiplash injuries. The symptomatic relief provided by the soft collar is thought to result from the warming effect on the underlying soft tissues as well as the support to the weight of the head, which is otherwise balanced by the cervical musculature. This allows the muscles to rest during the period of myofascial inflammation following the injury. Patient compliance is high because of the comfort of the device. Hard collars made with supplemental plastic integrated into the soft support fabric are similar in function to soft collars. They do not add substantially to cervical stabilization (Fig. 38.2).
PREHOSPITAL EXTRICATION COLLARS
The rationale behind the use of prehospital immobilization is to prevent the initiation or propagation of cervical spinal cord injury (SCI) in individuals with high-energy trauma who are at risk for underlying cervical spinal column injury. The injury mechanisms that are responsible for most cervical spine trauma include motor vehicle collision, fall from height, diving, and collision sports. With the advent of modern prehospital resuscitation and transportation through the emergency medical system (EMS), the use of careful cervical immobilization has become the standard of care (1,18).
Numerous devices and supplemental immobilization techniques are available. Each has its own advantages and disadvantages. The decision as to which device will be used is largely in the hands of the emergency medical transport services and technicians who are the immediate responders to trauma in the field. However, physician leadership and oversight is necessary to ensure that children who are transported to emergency facilities and trauma centers by EMS have appropriate devices applied in a manner that protects the cervical spine and prevents the occurrence or worsening of neurologic injury.
Ideally, a prehospital collar allows for adequate immobilization and possesses the following features: is easy to apply while in-line cervical control is maintained, inexpensive, and comfortable (avoiding anxiety or resistance); has small storage space requirements; is adjustable to fit a variety of patient sizes and shapes; and reduces the risk of decubitus ulceration with extended use during transportation and early hospital immobilization (especially in unconscious or sedated children) (18). Because the exact amount of acceptable residual motion of the cervical spine is unknown, it is necessary to carefully supplement all collars, regardless of their comparative efficacy, with additional techniques of total spinal immobilization. Spine board and short board techniques are the most effective supplemental methods to support the cervical spine and prevent unacceptable rotation or movement (34,35). Head bolsters, taping, and strapping are performed in a team approach to rapidly secure the trauma patient for safe transport (36,37). Leadership and open communication are needed to execute this in a repeatedly safe manner.
Special attention is necessary in the pediatric population in order to maintain neutral cervical alignment. Anthropometric data show that the head circumference and sagittal diameters increase at logarithmic rates during childhood, whereas the thoracic height increases at a linear rate. The resulting mismatch creates excessive cervical spine flexion when a small child is immobilized on a flat spine board. To prevent this, it is necessary to provide supplemental elevation of the thorax with either a thoracic pad or an occipital recess in the spine board. Because the exact amount of padding necessary to align the cervical spine may vary substantially from child to child, the thoracic padding may allow more latitude in adjusting cervical alignment. The general rule of thumb is to apply sufficient padding under the thorax that allows the external auditory meatus to be in alignment with the crown of the shoulder (Fig. 38.3) (38). Padding of the spine board has been shown to reduce patient discomfort while maintaining
the same degree of cervical protection as is accomplished with unpadded boards (39). Unfortunately, transcutaneous oxygen tension of the sacrum is not notably improved with spine board padding (39). It is essential for hospital personnel to be mindful of the risk for decubitus ulcer formation with prolonged use of the spine board during early hospitalization (40,41). Every effort should be made to remove the spine board and prehospital cervical immobilization as soon as spinal clearance can be achieved by radiographic and clinical protocols. Unconscious or sedated children may require alternative techniques such as magnetic resonance imaging (MRI) or fluoroscopy to help clear the spine. Consideration may also be given to adopting a meticulous skin care protocol to reduce the risk of skin ulceration (40,42).
the same degree of cervical protection as is accomplished with unpadded boards (39). Unfortunately, transcutaneous oxygen tension of the sacrum is not notably improved with spine board padding (39). It is essential for hospital personnel to be mindful of the risk for decubitus ulcer formation with prolonged use of the spine board during early hospitalization (40,41). Every effort should be made to remove the spine board and prehospital cervical immobilization as soon as spinal clearance can be achieved by radiographic and clinical protocols. Unconscious or sedated children may require alternative techniques such as magnetic resonance imaging (MRI) or fluoroscopy to help clear the spine. Consideration may also be given to adopting a meticulous skin care protocol to reduce the risk of skin ulceration (40,42).
 Figure 38.3. Prehospital extrication immobilization collar (NecLoc; Jerome Medical, Moorestwon, NJ). |
Examples of prehospital extrication collars include the Philadelphia collar (Philadelphia Collar Co., Philadelphia), NecLoc collar (Jerome Medical, Moorestown, NJ), Stiffneck collar (Laerdal Medical Corp., Armonk, NY), Aspen collar (International Healthcare Devices, Long Beach, CA), Jobst Vertebrace collar (Jobst Institute, Inc., Toledo, OH), and Vacuum Splint cervical collar (Germa, Sweden; supplied by Med-Tech, Loveland, CO).
AMBULATORY IMMOBILIZATION COLLARS
There are several different ambulatory immobilization collars available currently. Indications for the use of these devices include symptomatic treatment for cervical strain or spasm and supplemental immobilization following surgical stabilization in selected cases. These collars do not provide adequate immobilization of the cervical spine to reliably restrict undesired motion in the potentially unstable spine. A study of cervical collars used in rheumatoid atlantoaxial subluxation showed that none of the collars were effective in limiting anterior subluxation of the atlas in maximum flexion (43). Another study compared the rate of healing of type II dens fractures treated with a Philadelphia collar to those treated in a halo and demonstrated fracture union in 74% of halo patients compared with only 53% of collar patients (29). However, one study did demonstrate that isolated stable burst fractures of the atlas were effectively treated with the Miami J collar (Jerome Medical, Moorestown, NJ), a rigid, ambulatory cervical collar (24).
Some of these devices are well padded and provide a higher degree of patient comfort and compliance. Generally, the ambulatory immobilization collars are more expensive than the prehospital extrication collars. Examples of this type of collar include the Miami J collar and the Philadelphia collar (Figs. 38.4, 38.5 and 38.6).
The treatment of children with cervical collars requires an understanding of the variability of body habitus, which occurs during growth and maturation. The posterior occipital prominence progressively diminishes with age, while the relative neck length increases into adolescence and then diminishes into adulthood. Unfortunately, many cervical immobilization devices designed for use in children and adolescents resemble scaled-down versions of adult products. As a result of research and improved technology, dedicated pediatric products are available to improve the fit, comfort, and efficacy of these devices in children. The Miami Junior collar (Jerome Medical, Moorestown, NM) was created taking into account the anthropometric data on occipital size and neck length during maturation.
 Figure 38.4. Ambulatory immobilization collar for children (Miami Junior;Jerome Medical, Moorestown, NJ).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|