Thin Cortex
Susan I. Blaser, MD, FRCPC
DIFFERENTIAL DIAGNOSIS
Common
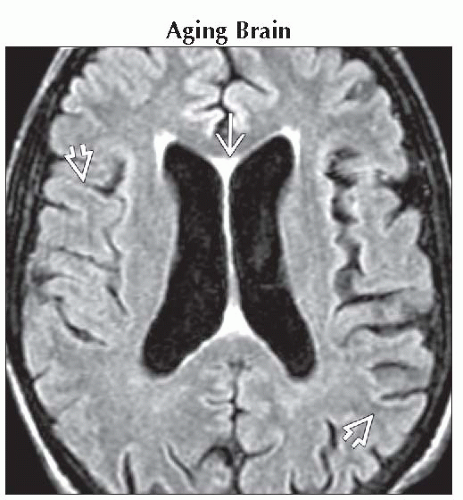
Aging Brain
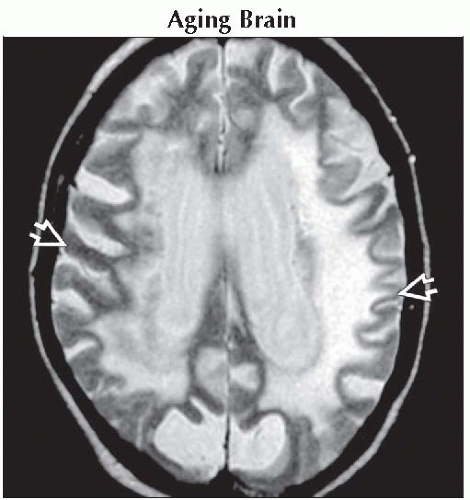
Prematurity
Obstructive Hydrocephalus
Cerebral Infarction, Chronic
Encephalomalacia, General
Less Common
Multiple Sclerosis
Alzheimer Dementia
Multi-Infarct Dementia
Frontotemporal Dementia
Rare but Important
Microcephaly
Subcortical Laminar Heterotopic Gray Matter
Inborn Errors of Metabolism (Gray Matter Disorders)
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Is cortical thinning focal (typical for encephalomalacia) or generalized?
Is cortex thin but normal signal intensity?
If abnormal, consider infection, infarction, trauma, etc.
Child vs. adult
Child: History important
Prematurity, family history of inborn error of metabolism
Seizures (heterotopias, encephalomalacia)
Adult: Normal cognitive function or demented?
Helpful Clues for Common Diagnoses
Aging Brain
White matter (WM), not gray matter (GM) volume loss predominates in normal “successfully aging” brain
Posterior vermis, cerebellum > cerebral hemispheres
Cortical thinning minimal
“Black line” in visual, motor/sensory cortex common in normal older patients
Prematurity
Hemispheric WM almost completely unmyelinated (“wet brain”)
Cortex always appears thin
Pre- and post-central gyri myelinate early
Hyperintensity on T1WI, hypointensity on T2WI normal
Note: White matter injury of prematurity spares GM
Undulating ventricular borders, ventriculomegaly
Generalized volume loss due to ↓ WM
Obstructive Hydrocephalus
“Maximal” hydrocephalus thins cortical mantle
May be difficult to distinguish from hydranencephaly on NECT
MR diagnostic
Cerebral Infarction, Chronic
Usually wedge-shaped, involves both cortex & underlying WM
“Hierarchy” of vulnerability to territorial or hypotensive ischemia
CA1 hippocampus most sensitive
GM generally more vulnerable than WM
Collateral flow across pial watershed (border zones) may permit cortex within ischemic penumbra to survive
Thin rim of cortex may persist adjacent to densely ischemic core of infarct
Often hyperintense on T2/FLAIR, reflecting spongiosis/gliosis
Encephalomalacia, General
Trauma, infection, toxic-metabolic insults
May primarily affect GM, WM, or both
Can be generalized (e.g., following global hypoperfusion) or focal
Helpful Clues for Less Common Diagnoses
Multiple Sclerosis
Multiple T2/FLAIR hyperintensities perpendicular to callososeptal interface
Chronic, severe multiple sclerosis (MS) causes variable brain atrophy
WM > > GM
But normal-appearing GM may have abnormal metabolic profile with ↓ NAA
Cortical loss in secondary-progressive MS common
Alzheimer Dementia
Alzheimer dementia (AD) is most common of all dementias
Best diagnostic clue = temporoparietal cortical atrophy + disproportionate hippocampal volume loss
Multi-Infarct Dementia
Also known as “vascular” dementia
Second most common dementia after AD
10-30% of all dementing disorders
Imaging findings vary
Generalized, diffuse atrophy
Large ventricles, superficial sulci
Generalized cortical thinning
Focal territorial &/or lacunar infarcts
Subcortical WM T2/FLAIR hyperintensities
Diffuse bilateral, confluent deep WM hyperintensity secondary to arteriolosclerosis
Frontotemporal Dementia
One of several tauopathies, also known as Pick disease
Frontotemporal dementia (FTD) causes disproportionate frontotemporal atrophy
“Knife-like” gyri with very thin cortex
Subcortical WM usually hyperintense
Parietal, occipital lobes relatively spared
Helpful Clues for Rare Diagnoses
Microcephaly
Small head size, ↓ craniofacial ratio
Sutural overlap common
Simplified gyri with thin cortex
Shallow sulci
Many causes
Primary (genetic) microcephaly (e.g., § microlissencephaly, many syndromes)
Secondary (nongenetic) microcephaly (e.g., TORCH infection, fetal alcohol syndrome)
Subcortical Laminar Heterotopic Gray Matter
“Band” heterotopia (“double cortex”): LIS1 or LISX1
Thick inner band of dysplastic GM in subcortical WM =’
Overlying cortex thin (not all neurons “arrive”) §
Classic lissencephaly: (LIS1)
Shallow sylvian fissure (“hourglass” configuration of hemispheres)
Thin outer layer of GM
“Cell sparse” WM zone
Thick inner band of GM
Inborn Errors of Metabolism (Gray Matter Disorders)
Includes inborn errors of metabolism that affect WM > > GM
Many “poliodystrophies”; all uncommon
All have similar imaging appearance
Generalized atrophy with ↑ sulci, thinned cortex
Cortical signal generally normal
BUT WM often hyperintense due to secondary axonal degeneration
Lysosomal (example: Neuronal ceroid lipofuscinosis) clue
Hypointense thalami (best seen on standard T2WI, not FSE T2WI)
Image Gallery
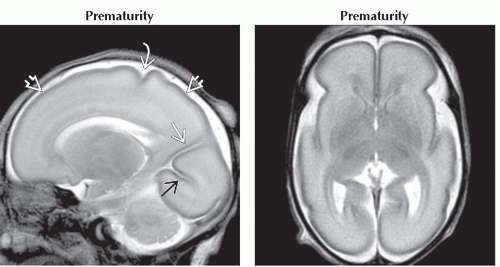 (Left) Sagittal T2WI MR in a normal 28 week premature infant shows thin cortical ribbon
 . The brain is smooth, and only the central . The brain is smooth, and only the central  , calcarine , calcarine  , and parietooccipital , and parietooccipital  fissures are present. (Right) Axial T2WI MR in the same patient shows age-appropriate, undersulcated brain. The shallow, “squared” sylvian fissures are normal, as is the very thin cortical mantle overlying almost completely unmyelinated hemispheric white matter. fissures are present. (Right) Axial T2WI MR in the same patient shows age-appropriate, undersulcated brain. The shallow, “squared” sylvian fissures are normal, as is the very thin cortical mantle overlying almost completely unmyelinated hemispheric white matter.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|