Chapter 38 Thoracolumbar Junction Stabilization
ANTERIOR STABILIZATION
The use of spinal instrumentation for anterior column reconstruction is known to improve fusion rates and provide immediate stability at the thoracolumbar junction. Anterior instrumentation for the thoracolumbar spine was first applied by Dwyer and colleagues for the correction of scoliosis, using the cable and screw system.1 Zielke and colleagues modified the Dwyer system by substituting a 3.2-mm single threaded rod with nuts for the cable.2 Kostuik has reported the anterior spinal fixation system using a Dwyer-Hall vertebral plate and Harrington distraction rod (anterior Kostuik-Harrington system) in the treatment of spinal fracture3 (Fig. 38-1).
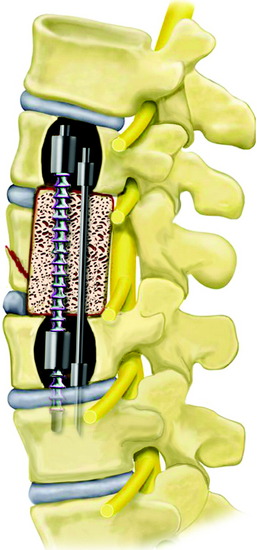
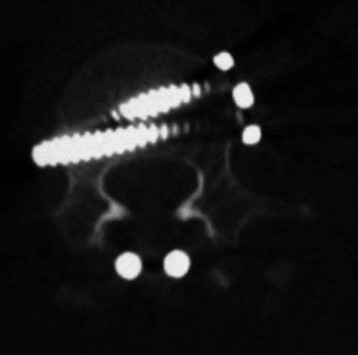
Kaneda and co-workers developed a technique of spiked vertebral plates attached to vertebral bodies via screws interconnected by rigid rods. The Kaneda Smooth Rod Spine System (Kaneda SR™; DePuy Spine, Raynham, MA) consists of rods and four constrained bicortical screws that allow compression and distraction (Fig. 38-2).
OPTIONS IN ANTERIOR FIXATION OF THORACOLUMBAR JUNCTION
SCREW-ROD SYSTEM
Tumor Removal (Corpectomy) and Graft Insertion
The discs and endplate material rostral and caudal to the tumor are removed. The removal of the tumor-infiltrated vertebral body is performed. The posterior cortex of the vertebral body is removed, and the ventral dura should be visible. After corpectomy, the width of the vertebral bodies above and below the corpectomy site is measured using the depth gauge. This value can be used as a guide to select the correct screw length to achieve bicortical fixation. As a general rule, anterior screws are typically 5 mm shorter than posterior screws. The selected vertebral body spacer with bone graft is replaced. A titanium mesh cage with a larger diameter and/or augmentation of the internal end ring produces a significant increase of the interface strength between the cage and the vertebra.4
Staple Placement
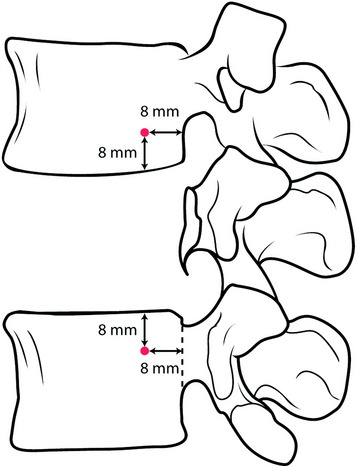
The selected staples are fixed into the proper position on the vertebral body (Fig. 38-3). The center spike enables the surgeon to create a firm attachment.
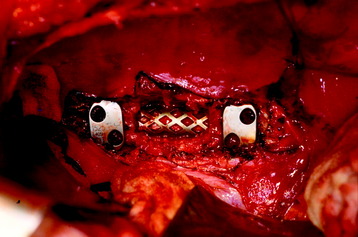
Fig. 38-3 Staple placement after graft insertion. Anterior slots are kept farther apart than posterior slots.
When placed, the staples should be oriented on the spine so that the anterior screw holes are farther apart than the posterior screw holes. The location of the posterior hole is 8 mm apart from the posterior cortical margin and from the adjacent endplate (Fig. 38-4).
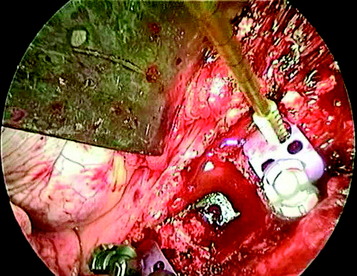
Screw Insertion
The awl may be used to create the pilot screw hole. The awl will create a 15-mm deep channel into the bone to guide the tap and screw. Following the awl’s path, the tapping screw is inserted (Fig. 38-5). The anterior and posterior screws’ trajectory should be arranged in a convergent fashion. The converging angle between them is about 8 degrees. On the coronal plane, they should be arrayed in parallel with the adjacent endplate. For maximum rigidity in an anterior spinal construct, the ideal device is one that provides graft compression by means of four bicortical screws constrained to the rods. Anterior screws may fail to bear axial loads effectively because of parallelogram translational deformation. A simple convergent insertion of the screws should prevent construct failure of this mechanism. Screws should be inserted until the screw head comes into contact with the staple. Screw openings should be parallel to the spine to allow for insertion of the rods. In principle, the screw is positioned for the bicortical purchase. Bicortical screws are significantly stronger in resisting pullout than are unicortical screws (Fig. 38-6). Advancing an anterior vertebral body screw to engage the second cortex increases resistance to pullout by 25–44%, depending on vertebral bone mineral density.5
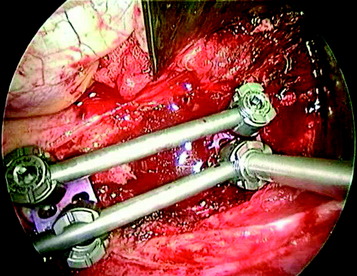
Rod Placement and Tightening
The rod is laid down on the screw head, and the rostral screw is locked with the rod stabilizer and tightening torque wrench to 80-inch pounds (Fig. 38-7). The caudal set-screws remain loose for compression of the construct. If the construct has a load-sharing capacity, the implant construct requires short fixed or applied moment arm cantilever beam constructs. The implant construct also should be in a compression mode, which causes the load to be shared between the graft and the implant construct. While the compression force is applied to the caudal screw, the set-screw is locked with a tightener.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree