Chapter 24 Thoracolumbar Spine Fractures
• The thoracolumbar junction is a flexible transition region in the spine, susceptible to injury due to transfer of kinetic energy.
• Clinicians should maintain a high suspicion of injury with thoracolumbar trauma because the incidence of a second vertebral fracture is 10% to 15%, and soft tissue injury may be as high as 50%.
• The most common mechanism of abdominal injuries is distraction or seat-belt injuries. Blunt abdominal aortic dissections are associated with distraction-rotational injuries of the thoracolumbar region.
• The three-column model of spine injury suggests that when all three columns are injured surgery may be necessary. Goals of surgery should be restoration of stability, balancing of opposing biomechanical forces, and decompression of the spinal canal with the aim to improve neurological outcome.
• Dorsal decompression via multilevel laminectomy alone after thoracic and thoracolumbar injuries has been shown to be ineffective and should not be performed as an isolated treatment strategy. Pedicle screw fixation provides for instrumentation of vertebrae with fractured or absent laminae, with purchase through all three columns. Increased rigidity by pedicle screw fixation permits fewer segments of fixation, leading to the preservation of more motion segments.
Approximately 160,000 patients a year in the United States suffer traumatic spinal column injuries, with 10% to 30% of them having a concurrent spinal cord injury.1–4 Although the majority of these injuries involves cervical (C1-C2) and lumbar (L3-L5) spine fractures, 15% to 20% of traumatic fractures occur at the thoracolumbar junction (T11-L2), whereas 9% to 16% occur in the thoracic spine (T1-T10).5,6 Paraplegia secondary to thoracic fractures have a first-year mortality rate of 7%,3,7 illustrating the devastating effects of thoracolumbar trauma.
Biomechanics
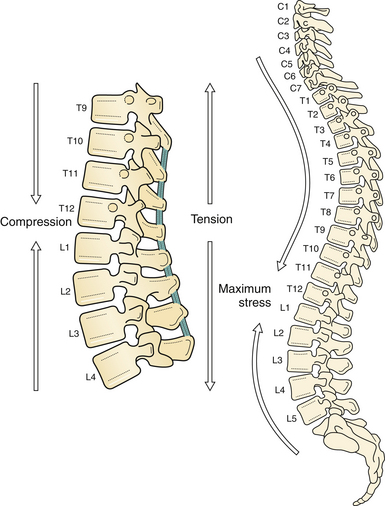
Forces along the long, rigid kyphotic thoracic spine catalyze an abrupt switch into the shorter, mobile lordotic lumbar spine at the thoracolumbar junction (Fig. 24.1). Biomechanically, this transition zone is susceptible to injury and is the most commonly injured portion of the spine. High-energy trauma (motor vehicle accidents) is the leading cause of injury over this region, followed by falls and sports-related injuries.8 Owing to the higher energy mechanisms of injury, additional organ systems are often injured in up to 50% of thoracolumbar trauma patients.8
The vertebral body is the primary load-bearing structure of the spine, with the intervertebral disk transferring all forces applied to the adjacent vertebral bodies.9,10 The annulus fibrosus of the intervertebral disk supports a significant portion of all applied axial and lateral loads and resists tension and shearing.11 The spinal ligamentous structures are essential in maintaining overall sagittal balance. The posterior longitudinal ligament (PLL) is a relatively weak ligament that provides some restriction to hyperflexion, along with the ligamentum flavum. The thick anterior longitudinal ligament (ALL) functions in resisting spinal hyperextension and distraction.12
The thoracic spine differs from the remainder of the spinal column because it is supported by and maintains articulations with the ribs. The intact rib cage increases the axial load-resisting capacity of the thoracic spine by a magnitude of four. The rib cage and facet articulations limit rotation, and therefore most thoracic spine fractures occur from a flexion or axial compression force vector.13 The majority of stability in flexion is provided by the costovertebral articulations.14,15 A significant factor in the degree and extent of fracture character is the rate of force impact loading.16
The thoracolumbar vertebrae are at an increased risk for developing compression fractures after trauma as a consequence of axial loads resulting from the natural kyphotic curvature of the thoracic spine.17 The kyphotic posture results in the placement of axial forces on the ventral portion of the vertebral body. If the strength of the ventral vertebral body is exceeded, a fracture of the vertebral body occurs, resulting in a vertebral compression fracture (VCF). The traumatic forces may also exceed the strength of the dorsal vertebral body and ligamentous elements, resulting in disruption of the dorsal tension band.
The osseous structures, ligaments, rib cage, and inherent anatomy impart great integrity on the thoracic and lumbar spine. The great kinetic energy needed for a fracture to the spine here is dissipated on impact through the soft tissue and viscous elements contained within and around the thoracic cavity, resulting in a high incidence of concurrent injuries. The incidence of concurrent injuries is reported to be greater than 80%, and these injuries involve the thorax, appendicular skeleton, and abdominal region.18–20 These high-energy impacts also affect remote areas from the trauma, such as the cranial vault. Petitjean and associates18 reported a 65% incidence of head injuries after high-velocity impacts, which resulted in incomplete thoracic spinal cord injury with 12% of these injuries classified as severe (Glasgow Coma Scale [GCS] score less than 8).18
Tearing or rupture of the aorta, with associated hemodynamic compromise, has been associated with thoracic vertebral fractures.18,21–23 Hemothorax in up to one third is another comorbidity.24,25 Pulmonary injuries have been reported in 85% of patients and typically consist of pulmonary contusions.26 Infrequently, perforation of the esophagus and tracheal injuries have also been associated with thoracic fractures.27–29
The thoracolumbar region is more vulnerable to concurrent injuries than the thoracic region because it is not provided the protection of the thoracic rib cage. Typically these injuries consist of hollow viscous injuries, such as intestinal perforations, mesenteric avulsions, or solid organ injuries.18,26,30
The most common mechanism of abdominal injuries is distraction or seat-belt injuries.18,26,31 Blunt abdominal aortic dissections are associated with distraction-rotational injuries of the thoracolumbar region.2,31 Multiple-level thoracic and lumbar fractures are also associated with a high incidence of abdominal injuries.2
Axial load injuries, particularly in patients who have jumped or fallen and landed on their feet, may manifest as both thoracolumbar fractures and calcaneal fractures. Miller and colleagues reported a 48% incidence of concurrent abdominal injuries associated with transverse process fractures.32 Therefore, a physician treating vertebral column injuries must be aware of not only the presence of spinal fractures but also the possibility of concurrent, nonspinal, soft tissue and bony injuries.
Radiographic Evaluation
In trauma patients, fractures are commonly missed in the early resuscitative period. Reportedly, between 5% and 15% of multisystem trauma patients have occult fractures missed on initial evaluation.33–35 Composing a minor proportion of traumatic fractures, thoracic spine fractures are extremely difficult to visualize compared to other vertebral or appendicular fractures. Approximately 20% to 50% of superior thoracic spinal fractures are not diagnosed by admission plain radiographs.5,20,36 Therefore, all suspected spinal trauma admissions should be immobilized until a thorough and detailed spinal evaluation can be performed. If appropriate stabilization precautions are not taken in this patient population, unforeseen neurological compromise may result.6
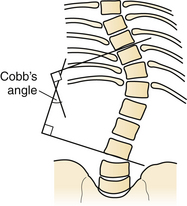
Initial radiographic assessment includes anteroposterior (AP) and lateral spine films assessing for loss of vertical body height, fracture of the pedicles, increased interpedicular distance, transverse process or rib fractures, and malalignment of vertebral bodies. One should examine the lateral radiograph for loss of body height, disruption of rostral or caudal end plate, dorsal cortical wall fracture with retropulsed bone, fracture of spinous processes, widening of interspinous distance, and subluxation or angulation of vertebral bodies.37 Malalignment in the AP plane is suggestive of fracture dislocation.38–40 The Cobb angle may also be calculated, for assessment of deformity.41
The Cobb angle is a measurement commonly used for evaluation of coronal spinal curves in scoliosis on an AP radiographic projection. When measuring the Cobb angle, first one must identify the apical vertebra of the curve in question. This is the vertebra that is the most displaced and rotated from the midline alignment. The end or transitional vertebrae are also identified from the curve above and below the apical vertebra. The end vertebrae are defined as the most superior and inferior vertebrae that are least displaced and least rotated but still present in the deformity’s curve. Two lines are drawn, one along the superior end plate of the superior end vertebra and a second line drawn along the inferior end plate of the inferior end vertebra. Because these lines typically will not meet in the space provided, unless they are severe curves, perpendicular lines are drawn. The angle between the intersecting perpendicular lines is the same as the original lines and is referred to as the Cobb angle (Fig. 24.2).
In the presence of a vertebral body injury, the entire spine should be imaged in an orthogonal manner because of the high incidence (5% to 20%) of noncontiguous spinal fractures.19,42–44 Radiographically, a typical superior end plate thoracic fracture has loss of vertebral height, with or without malalignment, a widened paraspinal line, and possibly a widened mediastinum.20 Difficulties in imaging the upper thoracic region (T1-T4) have led to decreased reliance on diagnosis with plain films. Computed tomography (CT) is more sensitive in detecting fractures than plain radiographs.45 CT is particularly adept at showing the integrity of the middle column, the degree of canal compromise, as well as subluxations or fractures of facets and lamina.
Sagittal reconstructions are helpful in visualizing flexion-distraction injuries and fracture dislocations. CT image reconstruction is also invaluable at the cervicothoracic junction because of the overlay of the scapula, shoulders, and surrounding tissues. In the obtunded patient this technique has been reported to identify more than 10% of fractures not visualized on plain radiographs.46 CT, however, has a limited capacity to visualize disk herniations, epidural or subdural hematomas, ligamentous disruption, or spinal cord parenchymal changes.47
Magnetic resonance imaging (MRI) has further improved the ability to visualize and comprehend the pathological anatomy of the soft tissue, ligamentous, intervertebral disk, and neural element disruption that occurs after spinal injury. MRI has supplanted CT myelography as the imaging tool of choice of the neuraxis, because it is faster, is noninvasive, and allows improved visualization of the spinal cord parenchyma.48,49
MRI evaluation is especially useful at the thoracolumbar junction because of the variable location of the cauda equina and conus medullaris in the adult population at this level.50 A neurological examination can be difficult to interpret at the conus/cauda equina transition level, as a result of the presence of lumbar spinal nerve sparing, the presence of concurrent injuries, sedation, in-dwelling catheters, and delayed reflex recovery. Accurate neural visualization may help in clarifying the pathological anatomy in this clinical situation.
Classification of Thoracolumbar Fractures
Injuries to the thoracic and lumbar spine account for more than 50% of all spinal fractures and a large portion of acute spinal cord injuries.51 Given this frequency and the significant impact of these injuries, significant advancements have been made in the surgical treatment of thoracolumbar trauma. Nonetheless, although there has been progress in the invention and continued evolution of spinal instrumentation and surgical techniques, medical decision making in spine trauma remains controversial.
A number of classification systems have been developed in an attempt to better define thoracolumbar trauma and aid treatment decision making. These systems are typically based on either anatomical structures (the Denis three-column system) or on proposed mechanisms of injury (Ferguson and Allen).52,53
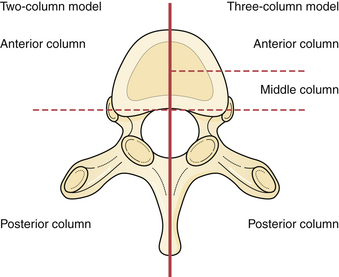
One of the earliest classifications of spinal fractures was by Watson-Jones in 1931, which was based primarily on diagnosis and treatment of flexion injuries.54 This was followed by Nicholl55 who developed the first detailed thoracic and thoracolumbar spinal fracture classification scheme and attempted to define unstable versus stable fractures after trauma in a series of flexion and flexion-rotation injuries.55 Later, Holdsworth56 (Fig. 24.3) further studied the importance of the spinal ligamentous complexes after thoracolumbar junction injuries and classified fractures according to their mechanism of injury into four main types: flexion, flexion and rotation, extension, and compression. Holdsworth56 further classified these fractures as unstable if the posterior ligamentous complex, consisting of the intervertebral disk, spinous ligaments, facet capsules, and the ligamentum flavum, was disrupted.57
Kelly and Whiteside58 reported that without dislocation of the dorsal elements of the spinal column neurological injuries rarely occur. They classified fractures based on structural criteria and considered the spine to consist of not one, but rather two separate supportive columns. The primary ventral column is composed of the vertebral bodies, and a second structural column consists of the posterior neural arches and ligaments. Later, Louis59 further modified this structural classification scheme by proposing a third column. Louis’ three-column concept consisted of one ventral column and two dorsal columns involving each facet articulation.
Denis used the enhanced CT imaging techniques, along with in vitro biomechanical data, to further modify the spinal column theories into a different three-column classification scheme (see Fig. 24.3). In this classification the ventral column consists of the ALL, the anterior annulus fibrosis, and the anterior half of the vertebral bodies. The middle column consists of the PLL, the dorsal annulus fibrosis, and the dorsal half of the vertebral bodies. Lastly, the posterior column, analogous to what Holdsworth defined as the dorsal ligamentous complex, consists of the bony neural arch, posterior spinous ligaments, and ligamentum flavum, as well as the facet joints. According to the Denis classification scheme, rupture of the dorsal ligamentous complex creates instability only if and when there is concurrent disruption of at least the PLL and dorsal annulus.53
Denis defined failure of the anterior column alone under compression (compression fracture) with an intact posterior column as a stable fracture. Burst fractures were defined as being generated through an axial compressive load, and involved failure of the anterior and middle columns. Severe tensile injuries resulted in seat-belt fracture or flexion-distraction injuries, which involve a disruption of the posterior and middle columns with an intact anterior column that serves as a fulcrum or hinge. The last category in Denis’ scheme is fracture dislocations, which are defined as a mechanical failure of all three columns, which makes them extremely unstable injuries (see Fig. 24.3).
McCormack and co-workers60 created a classification system based on a load-sharing principle that uses a graded point system based on the integrity of the vertebral bodies or anterior and middle column. Points are based on the amount of vertebral body comminution, spread of fragments at the fracture site, and the amount of corrected traumatic kyphosis.61,62 This classification scheme assists the surgeon in deciding if ventral spinal support is necessary after dorsal instrumentation, based on the premise that inadequate anterior column support will result in excessive loads being transferred to the dorsal elements (and instrumentation), thus increasing the risk for failure.
Vaccaro and associates63 proposed the thoracolumbar injury severity score (TLISS) in 2005, designed to simplify the classification of thoracolumbar injury and increase consistency of treatment among surgeons. This system helped address many of its predecessor’s limitations.64–67 The TLISS system defines injuries according to injury morphology, and now for the first time combined with both the PLL status and the neurological status of the patient.
The TLISS was designed to aid in medical decision making by providing both diagnostic and prognostic information with a weighted injury severity score. Stable injury patterns (TLISS < 4) may be treated nonoperatively with brace immobilization and active patient mobilization. Unstable injury patterns (TLISS > 4) may be treated operatively with the guiding principles of deformity correction, neurological decompression if necessary, and spinal stabilization followed by active patient mobilization.64,67
So far, the TLISS system has shown good to excellent intra- and interobserver reliability in a number of countries, among spine surgeons, and throughout a spectrum of spine treatment providers with varying levels of experience.64 A study of 71 cases of thoracolumbar traumatic fracture was given to five spine surgeons, along with details of the TLISS and instructions for scoring, finding a 96.4% agreement among surgeons.63 Furthermore, use of the TLISS has yielded more than a 90% agreement in the management of thoracolumbar trauma across a number of providers.68
Although the TLISS system has demonstrated success, there are inherent limitations. To date, many of the investigations into the TLISS system have been performed by individuals involved with its development.69 Additionally, a prospective application of the TLISS system and severity score to the treatment of spinal injuries is needed to define any improvements in care and patient outcomes compared with conventional systems.