♦ Preoperative
Operative Planning
- Review imaging (magnetic resonance imaging [MRI])
Equipment
- Major craniotomy tray
- Mayfield head holder
- High-speed drill
- Frameless stereotaxy (optional)
Operating Room Set-up
- Headlight
- Loupes (optional)
- Bipolar cautery and Bovie cautery
- Microscope
Anesthetic Issues
- Degree of intracranial pressure elevation is communicated to anesthesiologist
- Hyperventilation to pCO2 = 25 to 30 mm Hg
- Intravenous dexamethasone and antibiotics (i.e., oxacillin 2 g or vancomycin 1 g for adults) should be given 30 minutes prior to incision
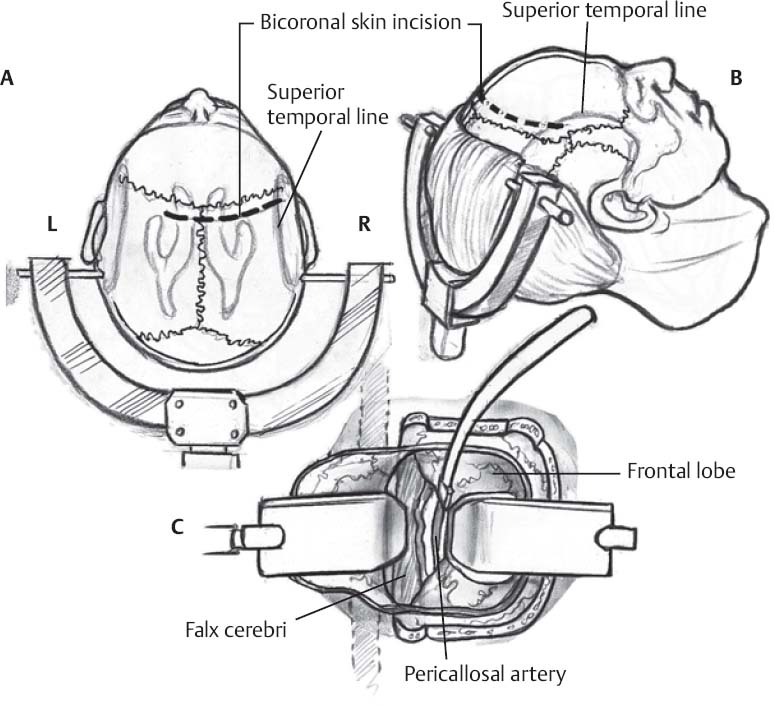
♦ Intraoperative (Fig. 10.1)
Positioning
- Patient supine with head straight in Mayfield head holder
- Neck is extended 10 degrees and the head of the operating table slightly elevated
Minimal Shave
- Use disposable razor
- Three-cm wide strip along planned incision is shaved
Sterile Scrub and Prep
- See Chapter 2, General Craniotomy Techniques
Incision
- Bicoronal skin incision
- Begun on right side 1.5 cm superior to zygoma and 1 cm anterior to external auditory canal
- Incision is continued across the midline 2 to 3 cm anterior to the coronal suture and ends ~4 cm superior to the zygoma and 1 cm anterior to the external auditory canal on the left side
- Begun on right side 1.5 cm superior to zygoma and 1 cm anterior to external auditory canal
- The anterior and posterior scalp flaps are reflected to expose 4 cm anterior and 2 cm posterior to the coronal suture, respectively
Burr Holes and Craniotomy
- The sagittal suture is identified
- Bone flap is planned to be centered two-thirds anterior and one-third posterior to the coronal suture and extended for no more than 2 cm posterior to the coronal suture
- At least 3 cm on the right and 1 to 2 cm on the left of midline exposure is desired so that the craniotomy is ~6 cm in length and 5 cm in width
- Slots are placed with a large, round burr at the anterior and posterior margins of the anticipated craniotomy directly over the superior sagittal sinus until dura on either side of the sinus is exposed and can be dissected from overlying bone
- The craniotome is used to cut bone from the right lateral aspect of the anterior slot to that of the posterior slot, and from the left lateral aspect of the posterior slot to that of the anterior slot; avoid injury to superior sagittal sinus with the craniotome
- Bone flap is elevated while stripping dura, with special care in the sinus region
- Bleeding points near the sagittal sinus are controlled with Gelfoam
- Slots are placed with a large, round burr at the anterior and posterior margins of the anticipated craniotomy directly over the superior sagittal sinus until dura on either side of the sinus is exposed and can be dissected from overlying bone
Dural Opening
- U-shaped dural flap based medially along sagittal sinus
- During elevation of the dura, microdissection is used to preserve pial integrity and avoid injury to cortical draining veins and pacchionian granulations
- The dural flap is reflected over the midline but not overturned, and then loosely secured with tacking sutures so that sagittal sinus occlusion is avoided
- Place ventricular drain into lateral ventricle through middle frontal gyrus if hydrocephalus is present
Approach to Corpus Callosum
- Protective Telfa strips are placed over the cortical surface
- The arachnoid in the interhemispheric fissure is opened sharply
- Irrigating bipolar cautery is used to divide arachnoid adhesions between the hemisphere and sagittal sinus
- Small bridging veins are judiciously divided to facilitate hemispheric retraction
- The optimal trajectory to the lesion is considered, based on the MRI, and identified, based on the location of the coronal suture
- Dissection is continued inferiorly along the falx; brain retractors are placed to maintain the interhemispheric corridor
- The callosomarginal and pericallosal arteries are encountered during the approach to the corpus callosum; although it is not necessary to identify the callosomarginal arteries, they should not be mistaken for the pericallosal arteries
- The pericallosal arteries are separated to each side or moved together to one side; the corpus callosum is easily identified by its pearly white color
- The self retaining retractors are checked to prevent excessive retraction of the sagittal sinus or cingulate gyri
Corpus Callosotomy
- Irrigating bipolar coagulation and suction are used to develop a callosotomy measuring ~1 × 2 cm
- The layers of the corpus callosum are successively traversed with cauterization and suction until the gray ependymal lining of the lateral ventricle is reached; the vessels of the ependymal lining are thoroughly cauterized to prevent bleeding into the ventricles
Entry into the Lateral Ventricle
- The cauterized ependymal layer is opened for entry into the lateral ventricle
- The brain retractor is repositioned just beyond the inferior callosal margin
- Orientation of entry into either the right or left lateral ventricle is confirmed by the configuration of the choroid plexus and thalamostriate vein, which course anteriorly in a medial direction to reach the foramen of Monro. Access to the right lateral ventricle after inadvertent entry into the left lateral ventricle is accomplished by further lateral resection of the corpus callosum or fenestration of the septum pellucidum.
- Release of cerebrospinal fluid (CSF) following entry into the lateral ventricle may result in a pressure gradient that displaces the septum pellucidum to the ipsilateral side; obstruction of the operative field is prevented by a generous fenestration and coagulation of the septum
Entry into the Third Ventricle
- Foraminal entry via the foramen of Monro, especially if it has been dilated by the presence of hydrocephalus, is the least traumatic; the choroidal fissure can be opened posteriorly to enlarge the foramen of Monro further
- If the lesion is inaccessible via foraminal entry, interforniceal approach is used
- The interforniceal approach is facilitated by a callosotomy that is as close to the midline as possible
- Identification of the interforniceal raphe is critical; this is accomplished by division of the septal leaves or, if they are fused, coagulation of the septum down to the level of the forniceal bodies
- The interforniceal raphe is sharply divided from the foramen of Monro posteriorly for a maximum distance of 2 cm to avoid damage to the hippocampal commissure
- The interforniceal approach is facilitated by a callosotomy that is as close to the midline as possible
Closure
- The resection cavity and ventricles are irrigated and filled with warm saline
- Patency of CSF drainage pathways is confirmed by passage of a microinstrument through the foramina of Monro and inspection of the third ventricular outlet into the cerebral aqueduct
- Meticulous hemostasis at each successive tissue layer from the ventricle to the hemisphere is achieved with bipolar cautery; hemostatic materials are minimized
- A ventricular catheter may be left in the lateral ventricle and tunneled under the flap
- Dura is closed in a watertight fashion with 4–0 silk sutures
- A central dural tenting suture is placed and dura is covered with dural substitute duraplasty (Duraform/DuraGen)
- The bone flap is secured with titanium microplates
- Galea is closed with inverted 3–0 Vicryl sutures
- Skin is closed with staples
- Xeroform and head wrap are applied
Postoperative
- Steroid taper begins on postoperative day 1
- Continue antibiotics until external ventricular drain is removed
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue