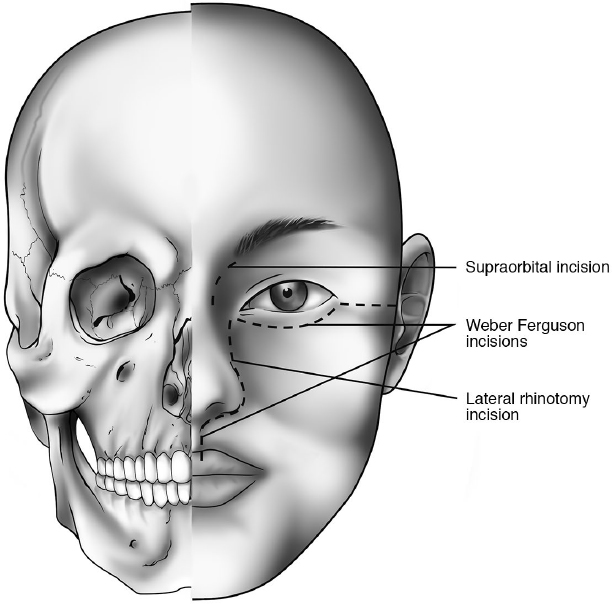
15 Transfacial/Transmaxillary Approaches to the Skull Base The paranasal sinuses and anterior skull base can be approached through external (transfacial/transmaxillary) or endonasal routes. Traditionally, external approaches were the only methods available, but in recent decades the expanded endoscopic approaches have been refined (see Chapter 16). • External approaches generally afford excellent exposure of the nose, paranasal sinuses, and anterior skull base. However, despite the wide exposure, it is sometimes difficult to visualize further into the nose or the sinus cavities, which require additional illumination or magnification. • The standard open transfacial and transmaxillary approaches provide access to the nose, sinuses, and anterior skull base. • Chronic ethmoid or frontal sinusitis • Persistent ethmoid/frontal sinusitis following endonasal sinus surgery • Frontal sinus fractures • Inflammatory complications of acute frontal sinusitis, including mucopyocele, or orbital or intracranial abscess • Repair of anterior cranial cerebrospinal fluid (CSF) leaks • Ligation of the anterior/posterior ethmoidal arteries (e.g., epistaxis) Fig. 15.1 The placement of various transfacial incisions: supraorbital, lateral rhinotomy, Weber-Ferguson. • Injury to the trochlea of the superior oblique (diplopia) • Injury to the supraorbital nerve (temporary or permanent forehead numbness) • Injury to the attachment of the medial palpebral ligament (telecanthus) • Cerebrospinal fluid leak from injury to the roof of the ethmoid/cribriform plate (potential for intracranial infection) • Hypertrophic scarring (reduced with the W-plasty) The osteoplastic flap is used to approach the frontal sinus through down-fracturing or removal of the anterior frontal sinus wall. Down-fracturing and hinging the anterior frontal table forward is preferred with the periosteum still attached to the anterior table to maintain the blood supply.3 • Large mucoceles eroding into the anterior fossa or orbit • Benign or malignant neoplasms involving the frontal sinus • Fractures of the frontal sinus/frontal bone • Reconstruction of defects of the anterior or posterior frontal sinus walls • Repair of frontobasal CSF leakage There are three incisions for performing an osteoplastic flap. The bitemporal coronal incision is preferred. • Bitemporal coronal incision • Mid-forehead incision • Gull-wing incision • The bitemporal coronal incision is preferred because of the wide exposure and the possibility of hiding the incision in the hair or hair line; however, it requires more dissection, and if there is preexisting alopecia (e.g., male pattern baldness), the incision may be noticeable postoperatively. • Alopecia along the incision line postoperatively may occur if the incision is not beveled parallel to the hair follicles or excessive cauterization of the scalp edge is used. • The mid-forehead incision is more direct to the anterior table and requires less dissection but has the potential to leave a visible scar and also has the disadvantage of leaving permanent numbness on the forehead superior to the incision. • The gull-wing incision provides direct exposure to the anterior forehead, but permanently sacrifices the sensory nerve supply to the forehead, and the incision is very noticeable postoperatively. Patients would generally consider the gull-wing incision cosmetically unacceptable, particularly when the other two options are available. There are several methods for outlining the limits of the anterior wall of the frontal sinus.5
 Main Indications
Main Indications
 Supraorbital Approaches (External Ethmoidectomy/Frontoethmoidectomy)1,2
Supraorbital Approaches (External Ethmoidectomy/Frontoethmoidectomy)1,2
Main Indications
 Incisions (Fig. 15.1; see also Chapter 20, Fig. 20.1, page 473)
Incisions (Fig. 15.1; see also Chapter 20, Fig. 20.1, page 473)
 The incision is usually placed equidistant between the medial canthus and the midline of the nasal dorsum.
The incision is usually placed equidistant between the medial canthus and the midline of the nasal dorsum.
 For the ethmoid sinus, the incision is made between the medial canthus and nasal sidewall. It should be placed to preserve the medial palpebral ligament and the lacrimal sac.
For the ethmoid sinus, the incision is made between the medial canthus and nasal sidewall. It should be placed to preserve the medial palpebral ligament and the lacrimal sac.
 For frontal or frontoethmoidal work, the incision runs below the medial portion of the eyebrow and curves downward between the medial canthus and the nasal sidewall to approximately the level of the inferior orbital margin.
For frontal or frontoethmoidal work, the incision runs below the medial portion of the eyebrow and curves downward between the medial canthus and the nasal sidewall to approximately the level of the inferior orbital margin.

 Variation: The incision may be extended further laterally under the eyebrow or inferiorly along the nasofacial groove, depending on the need for exposure.
Variation: The incision may be extended further laterally under the eyebrow or inferiorly along the nasofacial groove, depending on the need for exposure.
 Instead of a linear incision, a W-plasty type of incision along the nasal side-wall usually results in improved cosmesis postoperatively by reducing the risk of hypertrophic scarring.
Instead of a linear incision, a W-plasty type of incision along the nasal side-wall usually results in improved cosmesis postoperatively by reducing the risk of hypertrophic scarring.
 Soft Tissue Dissection
Soft Tissue Dissection
 The skin, muscle layer, and periosteum are incised so the periosteum can be easily elevated from the bone.
The skin, muscle layer, and periosteum are incised so the periosteum can be easily elevated from the bone.
 Bleeding from the angular arteries needs to be controlled by bipolar cautery or ligation.
Bleeding from the angular arteries needs to be controlled by bipolar cautery or ligation.
 The soft tissues are elevated over the lacrimal bone.
The soft tissues are elevated over the lacrimal bone.
 The lacrimal sac is preserved.
The lacrimal sac is preserved.
 If the ethmoid sinus is being accessed, the periorbita is elevated from the lamina papyracea, and the anterior ethmoid artery is identified and ligated as necessary.
If the ethmoid sinus is being accessed, the periorbita is elevated from the lamina papyracea, and the anterior ethmoid artery is identified and ligated as necessary.
 Bone Removal
Bone Removal
 The ethmoid sinus can be entered through the lamina papyracea more inferiorly, staying inferior to the level of the previously identified anterior ethmoid artery.
The ethmoid sinus can be entered through the lamina papyracea more inferiorly, staying inferior to the level of the previously identified anterior ethmoid artery.
 A complete ethmoidectomy can be performed along the skull base.
A complete ethmoidectomy can be performed along the skull base.
 The bony layer covering the anterior ethmoid cells is relatively thin and is easily removed with a punch or cutting bur.
The bony layer covering the anterior ethmoid cells is relatively thin and is easily removed with a punch or cutting bur.
 After the bone has been removed, the individual groups of ethmoid cells are removed piecemeal with standard sinus instruments under direct vision. Critical landmarks are the middle turbinate, the roof of the ethmoid, and laterally the orbital plate of the ethmoid bone.
After the bone has been removed, the individual groups of ethmoid cells are removed piecemeal with standard sinus instruments under direct vision. Critical landmarks are the middle turbinate, the roof of the ethmoid, and laterally the orbital plate of the ethmoid bone.
 For the frontal sinus, the floor of the sinus and its junction with the anterior wall are removed, exposing the lumen of the frontal sinus. Further bone is removed depending on the exposure needed for the pathology. With the “eyeglass” incision, a small bone flap can be created and temporarily removed to provide wider exposure of the frontal sinus.
For the frontal sinus, the floor of the sinus and its junction with the anterior wall are removed, exposing the lumen of the frontal sinus. Further bone is removed depending on the exposure needed for the pathology. With the “eyeglass” incision, a small bone flap can be created and temporarily removed to provide wider exposure of the frontal sinus.
Complications
 Osteoplastic Flap
Osteoplastic Flap
Main Indications4
 Incisions
Incisions
 Hair is removed for 1 to 2 cm along the line of incision.
Hair is removed for 1 to 2 cm along the line of incision.
 The incision starts anterior to the crus of the helix across the forehead to the contralateral side.
The incision starts anterior to the crus of the helix across the forehead to the contralateral side.
 The incision can be placed in front of the hair line (pre-trichal) or within the hair line.
The incision can be placed in front of the hair line (pre-trichal) or within the hair line.
 Bevel the direction of the scalpel in the direction of the hair follicles to avoid cutting across the hair follicles, which minimizes permanent alopecia postoperatively.
Bevel the direction of the scalpel in the direction of the hair follicles to avoid cutting across the hair follicles, which minimizes permanent alopecia postoperatively.
 Minimizing the use of electrocautery on the incision line helps to reduce the risk of alopecia. Bleeding is preferably controlled with bipolar cautery or hemostatic clamps (Raney clips).
Minimizing the use of electrocautery on the incision line helps to reduce the risk of alopecia. Bleeding is preferably controlled with bipolar cautery or hemostatic clamps (Raney clips).
 The lateral limbs of the incision should be placed sufficiently inferiorly to enable adequate mobilization and rotation of the soft tissue flap.
The lateral limbs of the incision should be placed sufficiently inferiorly to enable adequate mobilization and rotation of the soft tissue flap.
 Do not angle the incision anteriorly over the temple to avoid injury to the temporal branches of the facial nerve.
Do not angle the incision anteriorly over the temple to avoid injury to the temporal branches of the facial nerve.
 The incision goes through the skin, subcutaneous tissue, and galea.
The incision goes through the skin, subcutaneous tissue, and galea.
 The supraorbital and supratrochlear nerves are identified by a combination of blunt and sharp dissection near the supraorbital margins and protected.
The supraorbital and supratrochlear nerves are identified by a combination of blunt and sharp dissection near the supraorbital margins and protected.
 The outline of the bone cuts is marked on the anterior table (see below), and the periosteum is incised outside of the bone cut markings and elevated over the markings so that there is still periosteum intact on the anterior table. Some surgeons prefer to remove the anterior table, but this is not always necessary.
The outline of the bone cuts is marked on the anterior table (see below), and the periosteum is incised outside of the bone cut markings and elevated over the markings so that there is still periosteum intact on the anterior table. Some surgeons prefer to remove the anterior table, but this is not always necessary.
 Ideally the mid-forehead incision is placed in a horizontal forehead rhytid.
Ideally the mid-forehead incision is placed in a horizontal forehead rhytid.
 The remaining features are similar to those of the bitemporal coronal incision.
The remaining features are similar to those of the bitemporal coronal incision.
 The incision is placed superior to both eyebrows and joined across the glabella.
The incision is placed superior to both eyebrows and joined across the glabella.
 The supratrochlear and supraorbital nerves are sacrificed.
The supratrochlear and supraorbital nerves are sacrificed.
 The remaining features are similar to those of the bitemporal coronal incision.
The remaining features are similar to those of the bitemporal coronal incision.
Advantages and Disadvantages of the Three Incisions
 Bone Cuts: Surgical Approaches
Bone Cuts: Surgical Approaches
 The traditional method is to use a nonmagnified anterior posterior (6-foot Caldwell) X-ray template; the X-ray is taken preoperatively, and the frontal sinus is cut out, oriented, sterilized, and placed on the anterior table during the operation. The outline of the template is marked on the anterior table (e.g., using methylene blue or a sterile marking pen).6
The traditional method is to use a nonmagnified anterior posterior (6-foot Caldwell) X-ray template; the X-ray is taken preoperatively, and the frontal sinus is cut out, oriented, sterilized, and placed on the anterior table during the operation. The outline of the template is marked on the anterior table (e.g., using methylene blue or a sterile marking pen).6

 An alternate method is to make a small frontal trephination and place an endoscope into the frontal sinus with the operating room lights dimmed. The resulting transillumination outlines the confines of the frontal sinus.
An alternate method is to make a small frontal trephination and place an endoscope into the frontal sinus with the operating room lights dimmed. The resulting transillumination outlines the confines of the frontal sinus.

 A third method uses intraoperative image guidance to localize the frontal sinus walls.7
A third method uses intraoperative image guidance to localize the frontal sinus walls.7
 Steps:
Steps:
 The bone cuts are usually made with powered instruments such as an oscillating saw beveled in toward the frontal sinus to minimize the risk of inadvertent penetration of the posterior table and dura if the markings are slightly off.
The bone cuts are usually made with powered instruments such as an oscillating saw beveled in toward the frontal sinus to minimize the risk of inadvertent penetration of the posterior table and dura if the markings are slightly off.
 Osteotomes may help with the final elevation and down-fracturing of the anterior table of the frontal sinus.
Osteotomes may help with the final elevation and down-fracturing of the anterior table of the frontal sinus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Bilateral supraorbital incisions connected by an incision across the nasal dorsum/glabella (“eyeglass” incision) provide further wide exposure of the undersurface and anterior wall of the frontal sinuses, but the incision across the nasal dorsum is not cosmetically optimal.
Bilateral supraorbital incisions connected by an incision across the nasal dorsum/glabella (“eyeglass” incision) provide further wide exposure of the undersurface and anterior wall of the frontal sinuses, but the incision across the nasal dorsum is not cosmetically optimal.