Chapter 6 Transforaminal Epidural Block and Selective Nerve Root Block
TFEB requires a lower volume (1-3 mL) of injectate than conventional epidural block achieved by direct injection to the anterior epidural space. This smaller volume can decrease the toxicity from the injectate. No further injection is recommended if the first TFEB was not effective. If the initial response to TFEB is favorable but short-lived, a series of injections (3-6 times per year) or pulsed radiofrequency lesioning of the corresponding dorsal root ganglion (DRG) is recommended (see Chapter 7). The interval for sequential block varies from days to weeks for a series of injections.
Treatment objectives
Transforaminal Epidural Block
The treatment objectives of TFEB are to relieve pain and to increase the quality of life by:
Indications
Transforaminal Epidural Block
Indications for TFEB are as follows [1–10]:
 Radicular pain when urgent surgery either is not indicated or is contraindicated by medical conditions
Radicular pain when urgent surgery either is not indicated or is contraindicated by medical conditionsContraindications
Contraindications to both TFEB and SNRB are as follows [11,16]:
 Therapeutic anticoagulation (aspirin and antiplatelet agent therapy should be stopped 7 days, and warfarin therapy 5 days, before TFEB or SNRB)
Therapeutic anticoagulation (aspirin and antiplatelet agent therapy should be stopped 7 days, and warfarin therapy 5 days, before TFEB or SNRB)Preoperative preparation
History
The history for a patient who is to undergo TFEB or SNRB should include questions about pain characteristics, such as the quality and location of the pain, onset, and any relieving and aggravating factors. Questions should also be asked to identify “red flags”—signs and symptoms that might indicate the presence of cancer, cauda equina syndrome, or infection (Table 6.1).
Table 6.1 “Red Flags” in a Patient to Undergo Spinal Nerve Block: Signs and Symptoms Needing Rapid Evaluation and Operation
| Cancer-related signs | |
| Cauda equina syndrome-related signs | |
| Infection-related signs |
Anatomy and procedures
Cervical Region
Anatomy
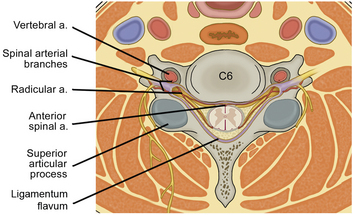
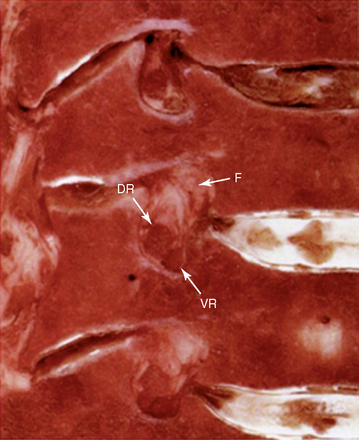
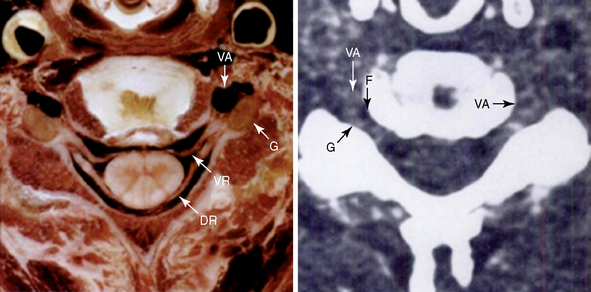
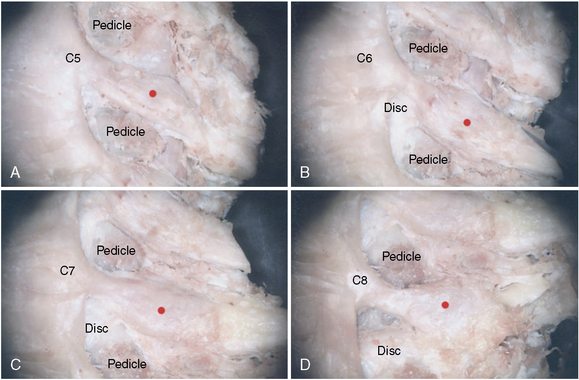
There are seven cervical vertebrae but eight cervical nerve roots. The first cervical nerve root is located between the occiput and the atlas, and each subsequent nerve root is located above its corresponding vertebra. If symptoms correlate with the seventh cervical nerve root, the C6-C7 foramen is the target for the block. The cervical neural foramen is a bony canal 4 to 5 mm long through which the cervical nerve roots pass anterolaterally (at about a 45-degree angle with respect to the coronal plane) and downward (at about a 10-degree angle with respect to the axial plane) (Figs. 6-1 to 6-4). Cervical spinal nerves from C3 to C7 exit the intervertebral foramen in the direction of the posterior, lower half of the foramen (Figs. 6-2 to 6-4). The cervical nerve roots occupy about one quarter to one third of the volume of the foramen and is accompanied by radicular arteries and veins (Figs. 6-1 and 6-2).
The vertebral artery at the caudal portion of the foramen is immediately anterior and medial to the ganglion (Figs. 6-1 to 6-4). In practice, the target points (red dots on Fig. 6-4) should lie directly over the dorsal part of the neural foramen so as to avoid vertebral artery injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree