60 Trauma to the Spine and Spinal Cord
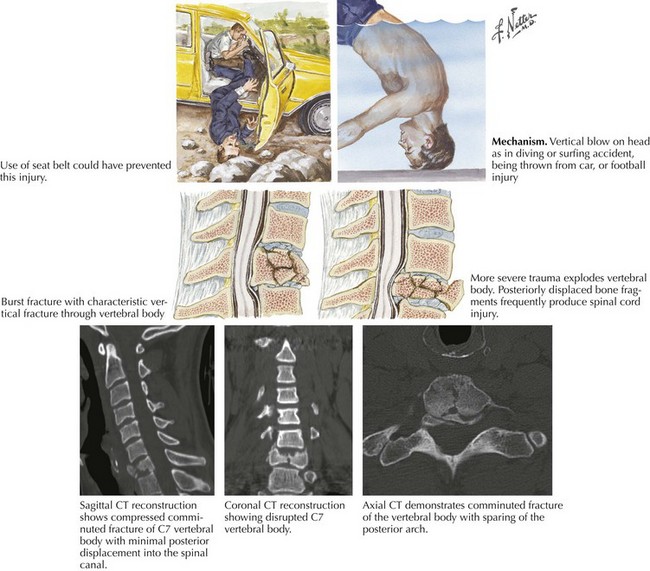
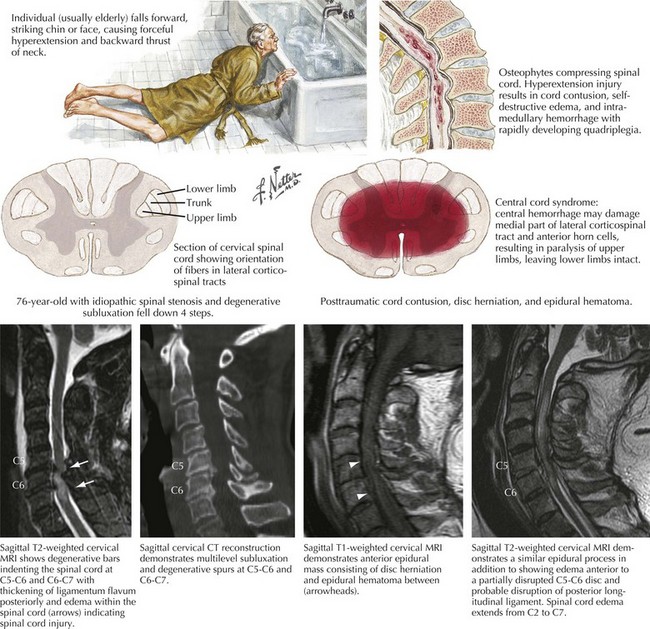
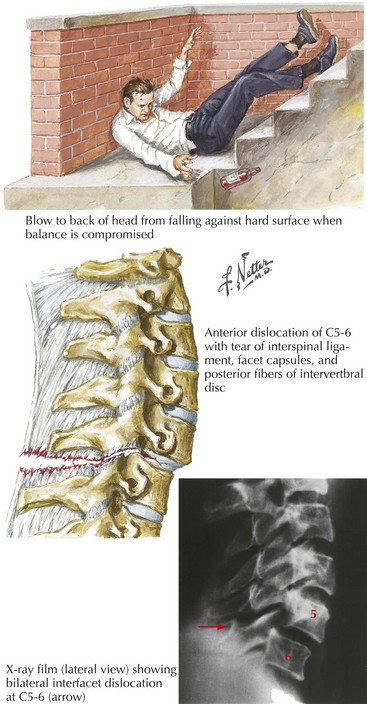
Major trauma centers evaluate two to three TSCI individuals out of every 100 patients brought to their emergency departments. The very high mortality (50%) associated with TSCI occurs mainly at the initial accident scene. Most often, these patients are accidentally injured while in an automobile (Fig. 60-1) or on a motorbike, particularly motorcycles. This type of injury also predisposes the patient to multiple-organ damage, for example, brain shear injury and/or intracerebral or subdural/epidural hematoma, cardiac tamponade, or a ruptured aorta, often leading to their very substantial fatality rate. In contrast, nonvehicular spinal cord injuries often occur with falls in (Fig. 60-2) or near the home (Fig. 60-3).
These patients have a 16% mortality rate if they survive to get to the hospital. Young men sustain 85% of TSCI, and thus there is a high correlation with alcohol, motor vehicle accidents, or athletic injuries usually from contact sports or on occasion skiing, diving, or trampolines. In the older population, individuals having significant predisposing cervical spinal spondylosis and/or stenosis are much more likely to develop TSCIs, a central cord injury (Fig. 60-2), from relatively simple falls on stairs or precipitously while navigating icy walkways.
Pathophysiology
Different types of trauma can lend themselves to severe spinal cord injury. One of the most well-known, particularly among adolescents, is that related to diving or vehicular trauma leading to compression damage to the spine and concomitantly the spinal cord (see Fig. 60-1). The more senior population is primarily subject to TSCI in relation to seemingly simple falls in the home (see Fig. 60-2); similarly, alcoholics or abusers of other drugs are also at significantly increased risk of spinal cord trauma (see Fig. 60-3).
In addition to the various types of trauma to the vertebrae per se (Fig. 60-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree