Chapter 231 Traumatic Central Cord Syndrome
Early Surgery
Central cord syndrome (CCS) is defined as an acute cervical spinal cord injury (SCI) presenting with a disproportionately greater motor impairment in the upper extremities than in the lower extremities, bladder dysfunction, and a variable degree of sensory loss below the level of injury.1–6 This was first described by Schneider in 1954.5,6 CCS has been reported to occur more frequently among older individuals with cervical spondylosis but has been reported in younger people as well.1,6 CCS is the most common SCI syndrome, accounting for 9% of traumatic SCIs.1,6 It is usually associated with a favorable prognosis including some degree of functional and neurologic recovery. Like other types of SCI, CCS tends to affect men more than women.1 The main cause of CCS is a hyperextension injury in an individual with preexisting chronic spondylosis.1–6 CCS associated with bleeding into the central aspect of the spinal cord portends a less favorable prognosis.1 At the cellular level, CCS is associated with axonal disruption in the lateral columns at the level of injury with relative preservation of the gray matter.
Surgical Management
The role and timing of surgical treatment for traumatic central cord syndrome have been the subjects of multiple retrospective class II and III studies. The timing of surgical decompression remains controversial but is generally accepted to be effective with controlled hemodynamic parameters.3,5 The emerging data from the Surgical Treatment for Acute Spinal Cord Injury Study (STASCIS), the only class I study in this field, shows significantly improved outcome with decompressive surgery within the first 24 hours in patients with isolated SCI.3,7 The continuing data from STASCIS long-term follow up will give us better answers about the effectiveness and timing of surgery for CCS.3,7 Some of the landmark class II and class III studies along with their conclusions and limitations are discussed next.
In their studies, Chen et al. analyzed the effect of time (before and after 4 days) and type (ventral vs. dorsal) of surgery as well as the type of spinal cord pathology on recovery in 49 patients with traumatic central cord syndrome (TCCS).2 The recovery was assessed by American Spinal Injury Association (ASIA) motor scores, the 36-item Short Form Health Survey (SF-36), the Walking Index for Spinal Cord Injury (WISCI), self-reported patient satisfaction (1–5), bladder management scores, presence of spasticity, and presence of neuropathic pain.2 The result of their study showed no correlation between any of the assessed variables and the recovery outcome. Some major limitations of this study include the lack of a comparative control group, the retrospective design of the study, and the arbitrary selection of 4 days to define the early group versus the late group.
However, in another retrospective study, Guest et al.4 reached a conclusion opposite to that of Chen et al.,2 finding early surgery highly effective in improving the outcome in TCCS. The authors analyzed the clinical characteristics, radiographic findings, ASIA score, and length of hospital stay in 50 patients who underwent either early (≤24 hours) or late (>24 hours) surgery.3,4 They found significant improvement in the ASIA score and length of hospital stay (P = .04) in patients with TCCS caused by acute disc herniation or fracture-dislocation who underwent early surgery.3,4 There was not a significant change in ASIA score for CSS secondary to spinal stenosis or spondylosis. The worst outcome was observed in patients older than 60 years in whom initial bladder dysfunction was present.3,4 One reason for the drastic difference in the results between these two studies is that the definition of early surgery was 4 days in the first study and 24 hours in the second study.
In another landmark study, Yamazaki et al. looked retrospectively at 47 patients with CCS.6 They reviewed clinical and radiologic data, including age, Japanese Orthopaedic Association Scale, anteroposterior diameter of spinal canal on CT, signal intensity change on T2-weighted MRI, associated spine diseases, and type of treatment received.6 They concluded that Japanese Orthopaedic Association Scale score on admission, signal changes in the MRI, and associated spine disease were not correlated with patient recovery.6 The only two variables that were found to improve the outcome significantly were the anteroposterior diameter (P = .0402) and the timing of surgery (P < .0001).6 The cut-off time for early versus late surgery was set at 2 weeks, which was considerably later than that in the first two studies. One would expect, on the basis of the Chen et al. study, that a late time setting (i.e., >24 hours) to define early versus late surgery would cause inaccuracy in the outcome and would not support a role for early surgery.2,6 However, possible interaction between multiple limitations such as an inaccurate time setting, a retrospective design, or lack of controlled subjects has resulted in a conclusion that actually favors early surgery. From all the preceding class II and III studies, it becomes obvious that a reliable conclusion could be achieved only if we were to run a prospective systemic study with well-defined and randomized control subjects. The closest to this idealistic goal is the STASCIS, which has released some promising results supporting the role of early surgery in improvement of the outcome in incomplete SCI.
Surgical Treatment for Acute Spinal Cord Injury Study
Run by multiple centers in North America, STASCIS is a long-term prospective study looking at 170 patients with various degrees of SCI.3,7. Of these subjects, 38% had incomplete SCI, 22% were rated ASIA B, and 16% were rated ASIA C.7 The subjects were randomly divided into early (<24 hours) and late (>24 hours) surgery groups.7 The preliminary report at 6 and 12 months follow-up was released in April 2010. The initial results have shown a two-grade improvement in the ASIA score in patients who took the early surgery (24% of subjects) versus late surgery (only 4%) (P = .009).3,7
Case Vignette
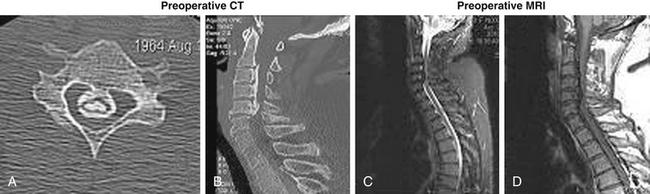
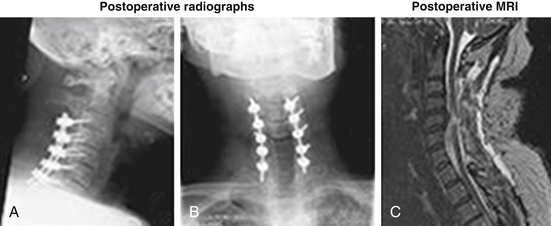
A 45-year-old woman with no significant past medical history had a syncopal episode, struck her head, and became immediately tetraplegic. She arrived in our hospital 6 to 8 hours later. Her neurologic status upon arrival at the emergency room was ASIA A, C6 motor level, T3 sensory level, HR 43/min, BP systolic 108 mm Hg. The preoperative workup included cervical MRI and CT (Fig. 231-1). Methylprednisolone IV infusion was initiated before arrival and was continued over the admission according to the National Acute Spinal Cord Injury Study (NASCIS) II protocol. The patient received dopamine IV continuous drip, keeping her mean arterial pressure over 85 mm Hg, to secure a reasonable blood flow at the injury site. The decompressive surgery (C3-7 laminectomy and dorsal instrumented fusion; Fig. 231-2) was performed in emergency (in the first 10 hours after trauma and the first 2 hours after arrival in our hospital). Some motor activity was noticed on the left side (both upper and lower limbs) very early postoperatively (in the recovery room). The patient’s neurologic status continued to improve, and she was transferred to a rehabilitation facility as an ASIA C patient. At 6 weeks postoperatively, her neurologic status was consistent with that of an ASIA D impaired patient, with a normal motor function on the left side (both upper and lower limbs, except a mild deficit in the hand) but significant motor deficits on the right side. The patient was still using intermittent self-catheterization to void the bladder, but rectal and micturitional sensation was present. Concluding, we assume that all elements from this scenario—early transportation to a medical facility, early diagnosis, early decompressive surgery, a dopamine drip to maintain mean BP over 85 mm Hg, and early administration of methylprednisolone—contributed to this excellent outcome.
Conclusion
The effectiveness and timing for surgery in TCCS have been studied in multiple class II and class III retrospective studies with contradictory conclusions secondary to the limitations of the study designs. The initial data from the ongoing STASCIS projects support a recommendation for early surgery (<24 hours) in hemodynamically stable patients with severe TCCS. On the other hand, the senior author defers surgical treatment in patients with milder TCCS (ASIA D deficits with rapidly improving neurology) for 6 to 8 weeks after injury to allow the posttraumatic edema to resolve. Of note, Bizhan Aarabi at the University of Maryland is spearheading efforts to undertake a prospective randomized controlled trial to examine the timing of surgical intervention for TCCS.1 We await the results of this trial with great interest.
Aarabi B., Koltz M., Ibrahimi D. Hyperextension cervical spine injuries and traumatic central cord syndrome. Neurosurg Focus. 2008;25(5):E9.
Chen A., Yang H., Yang T., et al. Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine. 2009;10:3-8.
Fehlings MG. STASCIS: Early surgery in spinal cord injury improves outcomes, lowers complications. Paper presented at American Association of Neurological Surgeons 76th Annual Meeting: Abstract 600. Presented April 28, 2008.
Fehlings M.G., Arvin B. The timing of surgery in patients with central spinal cord injury. J Neurosurg Spine. 2009;10:1-2.
Guest J., Eleraky M.A., Apostolides P.J., et al. Traumatic central cord syndrome: results of surgical management. J Neurosurg Spine. 2002;97:25-32.
Harrop J.S., Sharan A., Ratliff J. Central cord injury: Pathophysiology, management and outcomes. Spine J. 2006;6:S198-S206.
Yamazaki T., Yanaka K., Fujita K., et al. Traumatic central cord syndrome: analysis of factors affecting the outcome. Surg Neurol. 2005;63:95-100.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree