Instability of the cervical spine in children can result from a large spectrum of conditions with a wide range of congenital and acquired etiologies. This chapter focuses on the presentation, evaluation, and treatment of cervical spine instability occurring in children following trauma or in association with congenital anomalies of the cervical spine.
Table 37.1 lists and categorizes the most frequently encountered causes of cervical instability.
The cervical spine in children can be divided into the upper cervical spine, extending from the occiput to the C2-C3 disc space, and the lower cervical spine, which extends caudally from C3. Compared to the lower cervical spine, the upper cervical spine is unique in its embryology, developmental anatomy, and biomechanics. At the lower levels, development occurs similarly to the thoracic and lumbar spine (
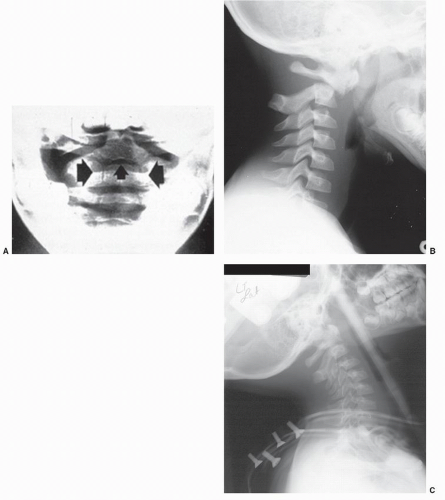
1). In contrast, development at the upper levels, particularly the atlas and axis, is unlike development in any other part of the spine. These distinct developmental features can determine the site and severity of the injuries. For example, the most serious cervical injuries observed in children, particularly those resulting in neurologic injury, occur in the upper cervical spine. This is likely the result of the unique anatomy and biomechanics occurring there. Also, the pediatric spine is continually changing with growth, maturation, and ongoing ossification of vertebral bodies as observed on radiographs. Particularly, during the first decade, the polar growth centers adjacent to the vertebral end plates and the many synchondroses present in the immature skeleton demarcate likely sites of vertebral injury. For example, the basal synchondrosis caudal to the base of the dens is the site of fracture separation in younger children (
2). This susceptibility to injury is covered more completely in the biomechanics section. Besides affecting stability, changes of the immature spine during growth make the radiographic evaluation of children difficult following injury or when presenting with congenital vertebral anomalies. This is particularly a problem for those less familiar with the radiographic appearance of the normal pediatric cervical spine.