Tricyclic and Related Antidepressant Drugs
The use of tricyclic antidepressants
Ever since Kuhn (1958) discovered the antidepressive actions of the archetypal tricyclic antidepressant imipramine, tricyclic antidepressants and related drugs have played an important part in the pharmacotherapy of depression. It was not until the 1980s, with the advent of SSRIs (see Chapter 9) that tricyclic antidepressants and related drugs began to be displaced from their position as the first-line pharmacological treatment for depression. In addition to their use in the treatment of depression, various tricyclic antidepressants are also used in the pharmacotherapy of dysthymia, panic disorder, phobic and obsessional states, childhood nocturnal enuresis, neuralgia, pruritus in eczema, and as an adjunctive treatment of cataplexy associated with narcolepsy.
Dosage
In general, tricyclic antidepressants have long half-lives. This allows for clinically effective once-daily dosing. It may be best to give more sedating antidepressants, such as amitriptyline, as a once-daily bedtime dose, to aid sleep, and to give less sedating ones, such as imipramine, earlier in the day, perhaps even first thing in the morning.
The elderly are particularly vulnerable to the hypotensive and hyponatraemic actions of tricyclic antidepressants. For these reasons, the initial dosage used in elderly patients should be kept low.
Choice
The tricyclic antidepressants include:
dibenzocycloheptanes:
amitriptyline
nortriptyline
iminodibenzyls:
clomipramine
imipramine
trimipramine
others:
dosulepin (dothiepin)
doxepin
lofepramine.
Tricyclic antidepressant-related antidepressants include:
trazodone.
Tetracyclic antidepressants include:
mianserin.
The more sedative tricyclic and related antidepressants include:
amitriptyline
clomipramine
dosulepin
doxepin
mianserin
trazodone
trimipramine.
These are more appropriate for patients suffering from agitation, anxiety, and, if given at bedtime, insomnia.
The less sedative tricyclic and related antidepressants include:
imipramine
lofepramine
nortriptyline.
These are more appropriate for patients suffering from withdrawal or apathy.
The British National Formulary (62nd edition) makes the following important comments on these different antidepressants:
Overdosage Limited quantities of tricyclic antidepressants should be prescribed at any one time because their cardiovascular and epileptogenic effects are dangerous in overdosage. In particular, overdosage with dosulepin and amitriptyline is associated with a relatively high rate of fatality. Lofepramine is associated with the lowest risk of fatality in overdosage, in comparison with other tricyclic antidepressant drugs….
Tricyclic and related antidepressants … have varying degrees of antimuscarinic side-effects and cardiotoxicity in overdosage, which may be important in individual patients. Lofepramine has a lower incidence of side-effects and is less dangerous in overdosage but is infrequently associated with
hepatic toxicity. Imipramine is also well established, but has more marked antimuscarinic side-effects than other tricyclic and related antidepressants. Amitriptyline and dosulepin are effective but they are particularly dangerous in overdosage (see ‘Overdosage’, p.138) and are not recommended for the treatment of depression; dosulepin should only be prescribed by specialists.’
hepatic toxicity. Imipramine is also well established, but has more marked antimuscarinic side-effects than other tricyclic and related antidepressants. Amitriptyline and dosulepin are effective but they are particularly dangerous in overdosage (see ‘Overdosage’, p.138) and are not recommended for the treatment of depression; dosulepin should only be prescribed by specialists.’
Withdrawal
Withdrawal of pharmacotherapy of drugs in this group should, as far as is possible, take place gradually.
Driving and the use of machinery
Most tricyclic antidepressants seriously impair driving performance, even more so than alcohol or benzodiazepines; in contrast SSRIs do not do so (Hale, 1994). Ramaekers (2003) reviewed the major results from studies published between 1983 and 2000 that examined the effects of antidepressants on actual driving performance using a standard test. Adverse changes on that test after acute doses of amitriptyline, imipramine, doxepin, and mianserin were comparable to those seen in drivers conducting this test with a blood alcohol level of at least 0.8mg/mL. Given the potential hazard of these drugs for driving, patients should not drive while taking them. They should also be strongly advised not to operate dangerous machinery.
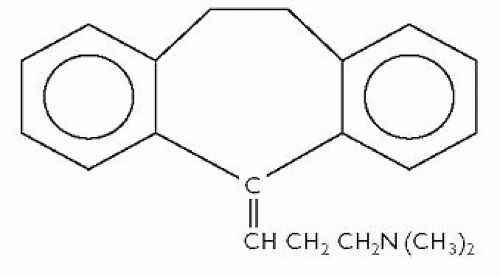
Amitriptyline
As mentioned earlier, amitriptyline is particularly dangerous in overdosage and is not recommended for the treatment of depression. Details of its structure and side-effects are given here for comparison with other tricyclic and related antidepressants.
Tricyclic antidepressants are believed to achieve their antidepressant activity through the following postulated actions:
inhibition of re-uptake of noradrenaline
inhibition of re-uptake of serotonin (5-HT).
This is the reason that tricyclic antidepressants are known as monoamine re-uptake inhibitors (or MARIs for short). The antiadrenergic action gives rise to the side-effect of postural hypotension, to which, as mentioned here, elderly patients are particularly susceptible. The action on serotonin re-uptake gives rise to gastrointestinal side-effects such as nausea and vomiting.
Tricyclic antidepressants also have antimuscarinic (anticholinergic) actions. These cause antimuscarinic side-effects, including:
dry mouth
blurred vision
mydriasis
drowsiness
disturbance of accommodation
increased intraocular pressure
urinary retention
dilatation of the urinary tract
constipation
paralytic ileus
hyperpyrexia.
Other side-effects, given by body systems, include:
cardiovascular:
ECG changes
AV conduction changes
arrhythmias
postural hypotension
tachycardia
palpitations
syncope
heart block
myocardial infarction and stroke have been reported with tricyclic antidepressants
nervous and neuromuscular:
behavioural disturbances
hypomania or mania
confusional states or delirium (particularly in the elderly)
disorientation
headache
convulsions
movement disorders and dyskinesias
paraesthesia
dysarthria
taste disturbance
tinnitus
EEG changes
tremors
haematological:
agranulocytosis
leucopenia
eosinophilia
purpura
thrombocytopenia
allergic:
skin rash
urticaria
photosensitization
oedema of the face and tongue
gastrointestinal:
nausea
vomiting
epigastric distress
stomatitis
rarely hepatitis (abnormal liver function tests and jaundice)
endocrine:
testicular enlargement and gynaecomastia in males
breast enlargement and galactorrhoea in females
changes in libido (increased or decreased)
impotence
blood sugar changes (increased or decreased)
syndrome of inappropriate ADH secretion
hyponatraemia (which may be caused by inappropriate ADH secretion)
other:
sweating
increased appetite
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree