CHAPTER 59 TRIGEMINAL AUTONOMIC CEPHALALGIAS: CLUSTER HEADACHE AND RELATED CONDITIONS
The trigeminal autonomic cephalalgias (TACs) are a grouping of headache syndromes recognized in the second edition of the International Headache Society (IHS) classification.1 The term was coined to reflect the underlying pathophysiology of a prominent part of the phenotype of the acute attacks: namely, the excessive cranial parasympathetic autonomic reflex activation in response to nociceptive input in the ophthalmic division of the trigeminal nerve.2 The TACs are classified in section III of the second edition of the IHS classification1 and include cluster headache,3 paroxysmal hemicrania, and shortlasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) (Table 59-1).4 In an early draft, hemicrania continua was included5 but this was finally classified in Section IV, which is appropriate, given the availability of newer brain imaging data.6 This chapter covers the shared physiology of these disorders and then the clinical aspects of each one in turn. Agents that are useful for these disorders are discussed. More detail on older clinical trials and agents that are used but are not particularly effective can be found elsewhere.4
TABLE 59-1 Differential Diagnosis of Trigeminal Autonomic Cephalalgias (TACs)
| Primary TACs | Similar Secondary Headaches | Secondary TACs |
|---|---|---|
AVM, arteriovenous malformation; SUNCT, shortlasting unilateral neuralgiform headache attacks with conjunctival injection and tearing.
PATHOPHYSIOLOGY OF TRIGEMINAL AUTONOMIC CEPHALALGIAS
Any explanation of the pathophysiology of TACs must account for the two major shared clinical features that are characteristic of the conditions: trigeminal distribution pain and ipsilateral cranial autonomic features.2 The pain-producing innervation of the cranium projects through branches of the trigeminal and upper cervical nerves7,8 to the trigeminocervical complex,9 from which nociceptive pathways project to higher centers.10 A reflex activation of the cranial parasympathetic outflow provides the efferent loop.
Experimental Studies
In the cat, stimulation of the trigeminal ganglion produces cranial vasodilation and release of neuropeptides, notably calcitonin gene–related peptide and substance P.11 The dilation is mediated by antidromic activation of the trigeminal nerve, which accounts for 20% of the effect, and orthodromic activation through the cranial parasympathetic outflow via the facial cranial nerve (VII), which accounts for the other 80%.12 The afferent pathway of the trigeminal-parasympathetic reflex traverses the trigeminal root,12 synapses in the trigeminal nucleus, and then projects to neurons of the superior salivatory nucleus in the pons.13 There is a glutamatergic excitatory receptor in the pontine synapse14 and projection via the facial nerve15 without synapse in the geniculate ganglion. The greater superficial petrosal nerve supplies classic autonomic preganglionic fibers to the sphenopalatine (pterygopalatine in humans) and otic ganglia.16 The sphenopalatine synapse involves a hexamethonium-sensitive nicotinic ganglion.16 Cranial nerve VII activation is associated with release of vasoactive intestinal polypeptide (VIP)17 and blocked by VIP antibodies.18 Blood flow changes in the brain depend on the frequency of stimulation19,20 and are independent of cerebral metabolism.21 VIP is found in the sphenopalatine ganglion,22 as is nitric oxide synthase, which is also involved in the vasodilator mechanism.23
Human Studies
The basic science implies an integral role for the ipsilateral trigeminal nociceptive pathways in TACs and predicts some degree of cranial parasympathetic autonomic activation. The ipsilateral autonomic features monifest clinically, such as lacrimation, rhinorrhea, nasal congestion, and eyelid edema, are consistent with cranial parasympathetic activation and sympathetic hypofunction (ptosis and miosis). The latter is likely to be a neurapraxic effect of carotid wall swelling24,25 with cranial parasympathetic activation. Cranial autonomic symptoms to some degree are, therefore, normal physiological responses to cranial nociceptive input.26–28 Indeed, other primary headaches, notably migraine,29 or secondary headache, such as trigeminal neuralgia,30 or trigeminal dysesthesias31 would be expected to have cranial autonomic activation, and they do. The distinction between the TACs and other headache syndromes is the degree of cranial autonomic activation, not its presence alone.32 This is why some patients with migraine have minor cranial autonomic activation, which is termed cluster migraine, whereas most such patients have migraine with cranial autonomic activation. This reflex also explains the curious report of a sense of aural fullness that patients with these syndromes may report if asked specifically and that has been reported clearly.33
Permitting Trigeminal-Parasympathetic Activation
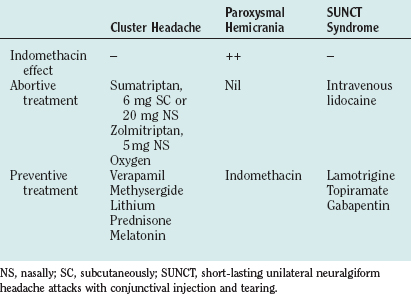
What is the basis for the prominence of cranial autonomic symptoms in the TACs? Is it a result of a central disinhibition of the trigeminal-autonomic reflex?32 Evidence from functional imaging studies—positron emission tomography studies in cluster headache34–36 (Fig. 59-1), and paroxysmal hemicrania36a and functional magnetic resonance imaging (MRI) studies in SUNCT (Fig. 59-2)37,38—have demonstrated ipsilateral posterior hypothalamic activation. Posterior hypothalamic activation seems specific to these syndromes and is not present in episodic39–41 or chronic42 migraine or in experimental ophthalmic trigeminal distribution head pain.43 Of interest is that in hemicrania continua, there is contralateral posterior hypothalamic activation, in contrast to substantially ipsilateral activation in cluster headache, and additional pontine and midbrain activation.6 There are direct hypothalamic-trigeminal connections,44 and the hypothalamus is known to have a modulatory role on the nociceptive and autonomic pathways, specifically trigeminovascular nociceptive pathways.45 Hence, the TACs involve abnormal activation in the region of the hypothalamus with subsequent trigeminovascular and cranial autonomic activation. Cranial autonomic features are not invariably linked with trigeminal pain and may persist after trigeminal nerve lesions.46
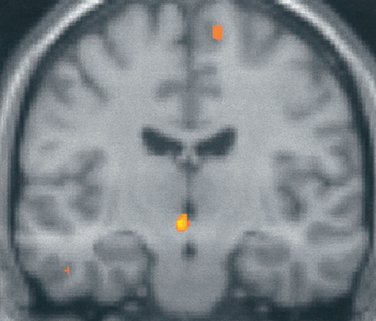
Figure 59-1 Brain imaging of cluster headache. Changes in the posterior hypothalamic gray area are revealed with positron emission tomography in patients with chronic cluster headache34 imaged during an acute attack triggered by nitroglycerin.
(From May A, Bahra A, Buchel C, et al: Hypothalamic activation in cluster headache attacks. Lancet 1998; 352:275-278.)
DIFFERENTIAL DIAGNOSIS OF TRIGEMINAL AUTONOMIC CEPHALALGIAS
The primary TACs need to be differentiated from secondary TAC-producing lesions, from other primary headaches, and from each other (see Table 59-1). The differentiation from secondary causes is not a problem if patients undergo imaging, but it can be extremely difficult if they do not. MRI of the brain with attention to the pituitary fossa and cavernous sinus reveals most secondary causes. In view of the rarity of paroxysmal hemicrania and SUNCT, MRI is a reasonable part of the initial evaluation of such patients. The situation is more complex for cluster headache. There are no studies with clear findings. The impression from a cohort that now exceeds 700 (the National Hospital for Neurology and Neurosurgery, Queen Square, London) is that MRI would detect no more than 1 per 100 cases of lesions in episodic cluster headache (ECH), and so its routine use cannot be recommended. For chronic cluster headache (CCH), MRI seems reasonable, in view of the very difficult nature of the long-term management and developments in neuromodulation as a treatment,47 which then make brain imaging more complex.
Among other primary headaches, migraine is the biggest problem in the differential diagnosis of cluster headache. Migraine can cluster, and despite the best descriptions of the IHS classification committee, short attacks do occur. Cranial autonomic symptoms are well reported,29 and the neuropeptide changes are substantially similar48 to those in cluster headache.49 The occurrence of attacks together does not seem to have the seasonal preponderance that is so typical of cluster headache,50,51 and this fact can be a useful differential diagnostic feature. This author regards the term cluster migraine as unhelpful and has yet to see a convincing case of a distinct biological entity usefully described by this name. Migraine could occur by chance in up to one third of cluster headache sufferers, in view of the peak female migraine prevalence and the generally accepted dominant inheritance pattern of migraine. The criterion for the effect of movement was added to the IHS description of cluster headache to sharpen the difference from migraine. The IHS committee hoped that this would draw attention to the fact that most patients with cluster headache feel restless or agitated,52 whereas most migraine patients are quiescent, as recognized in the first edition of the IHS classification.53 In clinical practice, this symptom and the periodicity are extremely helpful in establishing the differential diagnosis. The other feature of cluster headache, which is a feature of TACs in comparison with migraine, is that patients with TACs more often complain of unilateral, homolateral photophobia. In addition, triggering of headache quickly with alcohol, within 30 minutes, is more typical of cluster headache, whereas alterations in sleep patterns, eating, stress, or menses do not generally affect cluster headache. Warm environments seem to be a trigger in cluster headache, whereas barometric pressure change is a trigger of migraine.54
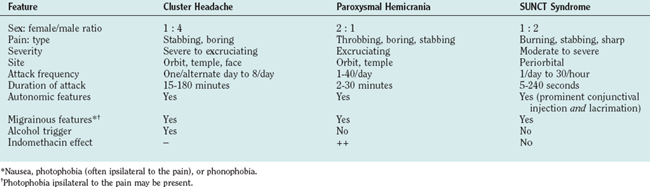
The TACs themselves (Table 59-2) can often be differentiated by the length of attack. This is certainly true when cluster headache is compared with SUNCT. The IHS criteria for TACs does betray an uncomfortable biological naivety with regard to the timing. The A, C, D, and E criteria are rather similar for each TAC (Tables 59-3 to 59-5). It would be easy to classify the attacks if those in SUNCT were up to 4 minutes long, those in paroxysmal hemicrania were 2 to 30 minutes long, and cluster headaches were 15 minutes and longer. The overlap then seems minimal. This seems wrong in absolute terms, because biology rarely provides such clear-cut rules, but it does provide a useful way to identify cases of sufficient similarity to make biological studies meaningful.
TABLE 59-3 Diagnostic Criteria for Cluster Headache
TABLE 59-4 Diagnostic Criteria for Paroxysmal Hemicrania
D. Attacks have a frequency of more than five per day for more than half the time, although periods with lower frequency may occur |
TABLE 59-5 Diagnostic Criteria for Short-Lasting Unilateral Neuralgiform Headache Attacks with Conjunctival Injection and Tearing (3.3)
B. Attacks of unilateral, orbital, supraorbital, or temporal stabbing or pulsating pain lasting 5 to 240 seconds |
CLUSTER HEADACHE
Cluster headache is a form of primary headache that is almost always unilateral and occurs in association with cranial autonomic features. Most patients report a striking circannual and circadian periodicity. It is an excruciating syndrome and is probably one of the most painful conditions known to humans; affected women have described the attacks as being worse than childbirth.
Epidemiology
The prevalence of cluster headache is estimated to be 0.4%,55 slightly higher than that of multiple sclerosis in the United Kingdom.56 The male/female ratio is 3.5 : 1 to 7 : 1.52,57 The male/female ratio has changed in case series since the early 1990s, with a trend toward a decreasing male preponderance; this is likely to be an ascertainment issue and not a real shift in female incidence. Cluster headache can begin at any age, although the most common age at onset is the third or fourth decade of life. Children as young as 4 years of age have been affected, but this is unusual.
Clinical Features
The Cluster Attack
With very few exceptions, cluster attacks are strictly unilateral, although the headache may alternate sides. The pain is excruciating. It is located mainly around the orbital and temporal regions, although any part of the head can be affected. The headache usually lasts 45 to 90 minutes, but the duration can range from 15 minutes to 3 hours. The onset and cessation are abrupt. Some patients experience interictal pain or discomfort.58
The signature feature of cluster headache is the association with autonomic symptoms, and it is extremely unusual for these not to be reported. According to the IHS diagnostic criteria,1 the attacks are accompanied by at least one of the following, which are present on the painful side: conjunctival injection, lacrimation, miosis, ptosis, eyelid edema, rhinorrhea, nasal blockage, forehead or facial sweating, or a sense of restlessness or agitation (see Table 59-2). The autonomic features are transient, lasting only for the duration of the attack, with the exception of partial Horner’s syndrome; in rare cases, ptosis or miosis may persist, especially after frequent attacks.
The full range of typical migrainous symptoms are reported in a significant proportion of patients with cluster headache.52,59,60 Premonitory symptoms (tiredness, yawning), associated features (nausea, vomiting, photophobia, phonophobia), and aura symptoms have all been described in relation to cluster attacks. However, in contrast to migraine, cluster headache sufferers are usually restless and irritable, preferring to move about, looking for a movement or posture that may relieve the pain.52
The cluster attack frequency varies between one every alternate day to three daily, although some sufferers have as many as eight daily, and clinical experience suggests that even more are possible. The condition can have a striking circadian rhythmicity; some patients report that the attacks occur at the same time each day. Alcohol, nitroglycerin, exercise, and elevated environmental temperature are recognized precipitants of acute cluster attacks. Alcohol induces acute attacks, usually within an hour of intake, in most sufferers, in contrast with migraine sufferers, who generally have headache some hours after alcohol intake. Alcohol triggers attacks during a cluster bout but not in a remission. Allergies, food sensitivities, reproductive hormonal changes,52 and stress do not appear to have any significant role in precipitating attacks.
Natural History
Although there is a paucity of literature on the long-term prognosis of cluster headache, the available evidence suggests that it is a lifelong disorder in most patients. In one study, in about 10% of patients with ECH, the condition evolved into CCH, whereas in one third of patients with CCH, it transformed into ECH.61 An encouraging piece of information for cluster headache sufferers is that a substantial proportion of them can expect to develop longer remission periods as they age.62
Treatment
The management of cluster headache includes offering patients advice on general measures and treating them with abortive agents, preventive agents, and, in rare cases, surgery (Table 59-6).
Abortive Agents
Triptans
Sumatriptan
Subcutaneous sumatriptan, 6 mg, is the drug of choice in the abortive treatment of a cluster attack. A randomized, placebo-controlled, double-blind, crossover study of 39 patients63 showed that headache severity was reduced at 15 minutes in 74% of attacks in which sumatriptan was administered, in comparison with 26% who received placebo. Of patients who took sumatriptan, 36% were pain free within 10 minutes, in comparison with 3% who took placebo. Sumatriptan was well tolerated, and there were no serious adverse events. A further study demonstrated no significant advantage to doubling the dose to 12 mg, although there were more side effects.64 Two large clinical trials show that long-term subcutaneous sumatriptan administration is well tolerated by patients who have cluster headache with no evidence of tachyphylaxis.65,66
A randomized, placebo-controlled, double-blind, crossover study of 86 patients67 showed that the severity of the headache at 30 minutes was reduced in 56% of attacks in which sumatriptan nasal spray, 20 mg, was administered, in comparison with 26% for which placebo was given. This formulation offers the prospect of effectively treating up to three attacks in 24 hours, in comparison with the subcutaneous 6-mg injection, for which the indicated dosing schedule is two doses in 24 hours.
Zolmitriptan
A double-blind, placebo-controlled trial compared the efficacy of oral zolmitriptan, 5 mg and 10 mg, to treat acute attacks in ECH and CCH.68 With headache response defined as a 2-point reduction on a 5-point pain intensity scale, 30-minute response rates in ECH were 29%, 40%, and 47% after placebo and 5 mg and 10 mg of zolmitriptan, respectively. The difference reached statistical significance only for 10-mg zolmitriptan in comparison with placebo. The efficacy of oral zolmitriptan in ECH is modest and does not approach the efficacy or speed of subcutaneous sumatriptan or oxygen; therefore, its utility in clinical practice is limited. It may be considered for patients who cannot tolerate subcutaneous or intranasal sumatriptan and oxygen or for those who desire oral medications. The intranasal formulation of zolmitriptan might be more appropriate for acute cluster headache because of its better overall pharmacokinetics,69 and a recent controlled trial has demonstrated its efficacy.
Oxygen
Oxygen inhalation is a safe and effective method for the acute treatment of cluster headache. Its mechanism of action remains unclear. Horton was the first to discover that inhaling 100% oxygen at the onset of attacks alleviates cluster headache pain.70 Kudrow71 noted a significant relief from cluster pain in 75% of 52 randomly selected outpatients treated with 100% oxygen administered through a facial mask at a rate of 7 L/minute for 15 minutes. Oxygen at 6 L/minute for 15 minutes was compared with air inhalation in a double-blind crossover study of 19 sufferers.72 Eleven patients used both gases. Of 16 patients who used oxygen, 9 (56%) perceived complete or substantial relief in 80% or more of their cluster attacks, in comparison with only 1 (7%) of 14 patients who used air.
Inhalation of 100% oxygen at 7 to 12 L/minute is usually rapidly effective in relieving pain. It should be inhaled continuously for 15 to 20 minutes through a non-rebreathing facial mask. Patients need to be informed that they should cover any apertures on the facial mask. When oxygen inhalation is initiated as soon as the attack starts, the attack is often aborted rapidly and entirely,71 although some patients find oxygen completely effective if taken when the pain is at maximal intensity.73 Up to 25% of patients note that oxygen simply delays the attack for minutes to hours rather than completely aborting it.71
Topical local anesthetics: lidocaine (lignocaine)
Kittrelle and colleagues74 first reported that lignocaine solution applied topically to the region of the pterygopalatine fossa alleviated the pain of the cluster attack. In an open-label trial of intranasal lignocaine 4% solution, four of five patients obtained rapid relief of nitroglycerin-induced cluster headache. Lignocaine was also effective in relieving spontaneous attacks. Robbins75 reported on the use of 4 to 6 sprays of lidocaine 4% in the nostril ipsilateral to the painful side in an open-label trial in 30 patients. Lidocaine (10%) applied bilaterally for 5 minutes was reported to be effective in aborting nitroglycerin-induced cluster attacks in a double-blind, placebo-controlled study in nine patients.76
Ergotamine and dihydroergotamine
Oral ergotamine is absorbed too slowly to be useful. It was widely recommended before the advent of the triptans, but it has little practical use in the modern treatment of acute cluster headache. Parenteral dihydroergotamine has been considered an effective abortive agent for cluster headache for some time.77,78 There are no controlled trials of injectable dihydroergotamine; however, clinical experience has demonstrated that intravenous administration provides prompt and effective relief of cluster headache within 15 minutes.79 Because of the frequency and the rapid peak intensity of cluster attacks, intravenous dihydroergotamine is not a feasible long-term solution. The intramuscular and subcutaneous routes of administration provide slower relief, although they have the advantage of being able to be self-administered. Dihydroergotamine nasal spray, 1 mg, has been studied in a double-blind, placebo-controlled, crossover trial in 25 patients.80 There was no difference in headache frequency or duration, but the pain intensity was significantly reduced with dihydroergotamine in comparison with placebo. The dosage used (1 mg) was lower than the recommended dosage for migraine (2 mg) and less than the currently available preparations of dihydroergotamine nasal spray (4 mg).
Somatostatin receptor antagonists
Intravenous somatostatin (25 μg/minute for 20 minutes) was compared with ergotamine (250 μg intramuscularly) or placebo in a double-blind trial comprising 72 attacks in eight patients.81 Infusion of somatostatin significantly reduced the maximal pain intensity and the duration of pain in comparison with placebo and, to a degree, was comparable with intramuscular ergotamine. In another randomized, double-blind study, subcutaneous somatostatin was compared with ergotamine.82 Five patients were treated for three attacks by each of the drugs. Subcutaneous somatostatin and ergotamine were equally beneficial with regard to effects on maximal pain intensity and the pain area, but somatostatin was less effective in reducing the duration of pain. Matharu and associates compared subcutaneous octreotide (100 μg), a somatostatin receptor agonist, with a matching placebo in acute cluster headache.83 The primary endpoint was the headache response, defined as very severe, severe, or moderate pain becoming mild or nil at 30 minutes. Fifty-seven patients were recruited, of whom 46 provided efficacy data on attacks treated with octreotide and 45 with placebo. The headache response rate with subcutaneous octreotide was 52%, whereas the response with placebo was 36%. When the treatment outcome was modeled as a binomial in which response was determined by treatment and period effect, sex, and cluster headache type were other variables of interest, subcutaneous octreotide, 100 μg, was significantly superior to placebo (P < 0.01). More work in this area may produce a novel non-vasoconstrictor approach to the treatment of acute cluster headache.
Preventive Treatments
Verapamil
Verapamil was first reported to be an effective preventive agent for cluster headache by Meyer and Hardenberg.84 In an open-label trial with verapamil at doses of 160 to 720 mg/day in five CCH patients, a reduction in the mean monthly headache frequency was reported in all patients. In another open-label trial with verapamil at doses of 240 to 600 mg/day for ECH and 120 to 1200 mg/day for CCH, an improvement of more than 75% was noted in 33 (69%) of 48 patients.85 A double-blind, crossover trial in which verapamil, 360 mg/day, was compared with the then standard prophylactic drug, lithium, 900 mg/day, each given for 8 weeks, demonstrated equivalent effects in the 24 CCH patients who completed the trial.86 Verapamil and lithium were superior to placebo. Verapamil caused fewer side effects and had a shorter latency period. In a double-blind, placebo-controlled trial, the efficacy of verapamil, 360 mg/day over a 2-week period, was evaluated in 26 patients with ECH.87 A statistically significant reduction in headache frequency and analgesic consumption occurred in the verapamil-treated patients, with a greater reduction in the second week of treatment.
Verapamil is the preventive drug of choice for both CCH and ECH, the latter when the bout is sufficiently long to establish a suitable dose. Clinical experience has clearly demonstrated that higher doses are needed for cluster headache than for cardiological indications. Dosages commonly employed range from 240 to 960 mg/day in divided doses. Verapamil can cause heart block by slowing conduction in the atrioventricular node,88 as demonstrated by prolongation of the A-H interval.89 In observing for P-R interval prolongation on the electrocardiogram, clinicians can monitor potential development of heart block, although it is a coarse measure. No formal guidelines are available. After obtaining a baseline electrocardiogram, the author and colleagues start patients on 80 mg three times daily, and the total daily dose is increased in increments of 80 mg every 10 to 14 days. An electrocardiogram is obtained before each increment and at least 10 days after the last dose change. The dosage is increased until the cluster attacks are suppressed, side effects intervene, or the maximum dose of 960 mg/day is achieved. It is unproved clinical experience that standard preparations of verapamil are more effective than the modified-release formulations.58,90
Constipation is the most common side effect, but dizziness, ankle swelling, nausea, fatigue, hypotension, and bradycardia may also occur. Gingival enlargement is a recognized problem that needs prompt attention from a dentist.91 β Blockers should not be given concurrently.
Lithium
The effectiveness of lithium in psychiatric conditions of a cyclical nature, such as manic-depressive psychosis and seasonal affective disorder, led Ekbom92,93 to try this agent in five patients with cluster headache, three of whom had CCH and clearly benefited from lithium. Open-label trials have been reviewed.94 Collectively, in more than 28 clinical trials involving 468 patients, good to excellent results were found in 236 (78%) of 304 patients with CCH. The response to lithium in patients with ECH was less robust than in those with CCH; good efficacy was obtained in 103 (63%) of a total of 164 patients treated. In most unblinded trials, a lithium dose ranging from 600 to 1200 mg/day was used. Lithium was often effective at serum concentrations of 0.4 to 0.8 mEq/L, less than those usually required for the treatment of bipolar disorder. Some patients eventually become resistant to lithium.95
Lithium has also been evaluated in two randomized, double-blind trials. A double-blind, crossover trial in which verapamil, 360 mg/day, was compared with lithium, 900 mg/day, each given for 8 weeks, demonstrated equivalent effects in the 24 patients with CCH who completed the trial86; verapamil and lithium were superior to placebo. In a double-blind, placebo-controlled, randomized, parallel-group trial of sustained-relief lithium with 27 patients with ECH, 13 received 800 mg/day, and 14 received placebo. Efficacy was assessed 1 week after treatment was begun.96 Cessation of attacks occurred in two patients in each group, and substantial improvement was noted in 6 (43%) of 14 patients taking placebo and 8 (62%) of 13 patients taking lithium. Lithium treatment was associated with a subjective improvement rate, but this was not statistically significant in comparison with placebo. The authors made an assumption at the onset of the trial that the placebo response would be zero. This is clearly incorrect for both acute attack and preventive treatment approaches in cluster headache.97
Lithium is an effective agent for cluster headache prophylaxis, although the response is less robust in ECH than in CCH. Most patients benefit from dosages between 600 and 1200 mg/day. Lithium has the potential for many side effects and has a narrow therapeutic window. Side effects include weakness, nausea, thirst, tremor, slurred speech, and blurred vision. Toxicity is manifested by nausea, vomiting, anorexia, diarrhea, neurological signs of confusion, nystagmus, ataxia, extrapyramidal signs, and seizures. Hypothyroidism and polyuria (nephrogenic diabetes insipidus) can occur with long-term use. Polymorphonuclear leukocytosis may occur and be mistaken for occult infection. Renal and thyroid function tests should be performed before and during treatment. The author and colleagues start patients on 300 mg twice per day and then titrate the dosage up until the cluster headaches are suppressed, side effects intervene, or the serum lithium level is in the upper part of the therapeutic range. The serum concentrations should be measured 12 hours after the last dose and should not exceed the upper level of the therapeutic range. Drug withdrawal at least once annually is advised, to detect the patients in whom CCH has transformed to ECH. The concomitant use of NSAIDs, diuretics, and carbamazepine is contraindicated.
Methysergide
Methysergide is an ergot alkaloid that is an antagonist at 5-hydroxytryptamine 2A (5-HT2A), 5-HT2B, and 5-HT2C receptors and an agonist at 5-HT1B/5-HT1D receptors. Methysergide was first reported to be effective in cluster headache by Sicuteri.98 Several authors subsequently confirmed this observation in open-label trials.99–105 The open-trials were reviewed by Curran and associates,106 who noted that methysergide, 3 to 12 mg/day, was effective in 329 (73%) of 451 patients with episodic cluster headache and chronic cluster headache.
For treatment of cluster headache, methysergide is indicated in dosages up to 12 mg/day, if tolerated. To minimize side effects, patients can start with a low dosage and increase the dosage gradually. The author and colleagues start patients on 1 mg once daily and increase the daily dose by 1 mg every 3 days in a three-times-daily regimen until the daily dose reaches 5 mg; thereafter, the dosage is increased incrementally by 1 mg every 5 days. Common short-term side effects include nausea, vomiting, dizziness, muscle cramps, abdominal pain, and peripheral edema. Uncommon but troublesome side effects are caused by vasoconstriction (coronary or peripheral arterial insufficiency), which usually necessitate cessation of the drug. Prolonged treatment has been associated with retroperitoneal, pulmonary, pleural, and cardiac fibrotic reactions, although these are rare.107 Ideally, the drug should be used only by patients with short cluster bouts, preferably less than 3 to 4 months. If prolonged use is intended, the risk of fibrotic reactions can be minimized by taking the drug for 6 months, followed by a 1-month holiday before starting the drug again. To avoid a sudden increase in headache frequency when methysergide is stopped, the patient should be weaned off over a 1-week period. Some authorities administer methysergide continuously with careful monitoring, which includes auscultation of the heart and yearly echocardiogram, chest radiograph, and abdominal MRI. All patients receiving methysergide should remain under the supervision of the treating physician108 and should be examined regularly for the development of visceral fibrosis or vascular complications.
Contraindications to methysergide use include pregnancy, peripheral vascular disorders, severe arteriosclerosis, coronary artery disease, severe hypertension, thrombophlebitis or cellulitis of the legs, peptic ulcer disease, fibrotic disorders, lung diseases, collagen disease, liver or renal function impairment, and valvular heart disease.109
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree