Hermann Stefan
O. Carter Snead III
Orvar Eeg-Olofsson
Introduction
The first clinical description of generalized absence seizures was by Poupart, in a report to the Académie Royale des Sciences in 1705: “At the approach of an attack the patient would sit down in a chair, her eyes open, and would remain there immobile and would not afterward remember falling into this state. If she had begun to talk and the attack interrupted her, she took it up again at precisely the point at which she stopped and she believed she had talked continuously.” Later in the eighteenth century, Tissot used the terms grands accès (“great attacks”) and petits accès in describing a 14-year-old child whose intervals between generalized convulsive seizures were punctuated with “a movement of the eyelids which at first seemed to be a tic, but which was soon recognized as convulsive.”15,115 Adie1 later described the characteristic features of a form of epilepsy with a good prognosis occurring in children. Neurophysiologic investigations in patients with epilepsies and impairment of consciousness by Gibbs and Gibbs42 proved for the first time that spike-and-wave paroxysms were the electroencephalographic (EEG) correlate of absence seizures. The clinical correlates of absence seizures during spike-and-wave paroxysms in the EEG also were described by Lennox and Davis.65 Although the terms petit mal and absence have been used interchangeably to describe this distinctive seizure type since the early part of the nineteenth century, it has been only with the advent of video-EEG (V-EEG) monitoring and careful studies utilizing that technique87 that the clinical spectrum of the absence seizure has come to be understood.
Definitions
Generalized absence seizures may be defined as a paroxysmal loss of consciousness of sudden onset and sudden end that is associated with bursts of bilaterally synchronous spike-and-wave discharges recorded on the EEG. Behaviorally, absence seizures are characterized by a sudden clouding of consciousness, usually associated with a motionless stare and cessation of ongoing activities. The beginning and end of the seizure are abrupt, and no aura or postictal state is observed. In addition to the clouding of consciousness, mild motor and automatic symptoms may occur. Brief absences may be detected only by cognitive testing during the seizure itself. Frequency of seizures in absence epilepsy varies from daily to weekly.
Absence seizures may be “typical” or “atypical.” Typical absence seizures are the most common, and are characterized by a loss of consciousness that is time-locked with bursts of bilaterally synchronous 3 cycles per second spike-and-wave discharges (SWD). Little if any cognitive impairment is observed with typical absence seizures, which generally respond well to pharmacologic treatments. This is in contrast to atypical absence seizures, which are less common, respond poorly to treatment, and are often associated with severe neurologic impairment.7,16 Although the pharmacologic profile of the two absence types is the same,25 four features may be used to distinguish typical from atypical absence seizures. The first is the neural circuitry involved in the SWD. In typical absence seizures, the epileptiform activity is constrained within thalamocortical circuitry.6,101 In contrast, there are experimental,21 clinical,41,53,91 behavioral,19 and neuroimaging36 data for the involvement of both thalamocortical and limbic circuitry in atypical absence seizures.
The second defining feature relates to the frequency of the spike-and-wave discharge. In typical human absence epilepsy, the frequency of the SWD is 3 Hz, while in atypical absence epilepsy the frequency is typically 1- to 2-Hz, and the background rhythms are slow for age.81 In rodent experimental models of typical and atypical absence epilepsy, the SWD frequency is similarly disparate, being 7- to 9-, and 4- to 6-Hz, respectively.20,21,22,101
The third major difference concerns voluntary behavior during the ictus. The ictal behavior in typical absence has an abrupt onset and offset that is time-locked with the spike-wave discharges. In contrast, voluntary movement and at least partial consciousness is maintained during the ictus in atypical absence seizures, in which the ictal behavior is gradual in onset and offset and is not time-locked to the spike-wave discharge.7,16,21,39,53,68,81,101
The final distinguishing feature is that a major difference in outcome occurs between children with typical versus atypical absence seizures. Children with typical absence seizures generally have a good outcome and are spared major cognitive deficits. This may relate to the restriction of the SWD to the thalamocortical circuitry in typical absence epilepsy. In distinct contrast, atypical absence seizures are associated with a severely abnormal cognitive and neurodevelopmental outcome in children.35,81 Similar cognitive deficits are observed in experimental models of atypical absence seizures.19 Therefore, whether absence seizures are typical or atypical is often used as a predictor of outcome in children with absence epilepsy.
Epidemiology
The annual incidence rate of absence seizures has been estimated to be 1/10,000.49 The estimation of the prevalence of absence seizures varies from 2.3%65 to 37.7%.64 Cavazzuti17 observed absence seizures in about 8% of epileptic children of school age. In absence epilepsies among children, absences are more frequent in girls than in boys. Absence seizures are
more often seen in childhood epilepsy, and predominantly occur in children of school age;84 however, absence seizures also are seen in adults,32 albeit less commonly.
more often seen in childhood epilepsy, and predominantly occur in children of school age;84 however, absence seizures also are seen in adults,32 albeit less commonly.
A family history of epilepsy is found in 15% to 44% of patients with generalized absence seizures,65 and an inherited factor in human absence seizures was first recognized by Metrakos and Metrakos.77 Genetic factors play a predominant role in the etiology of idiopathic generalized epilepsies with typical absence seizures.11,66,67 Because the concordance for absence seizures in monozygotic twins does not reach 100%, acquired factors also probably play a role in the causation of this type of seizure.10,11 Myoclonic absence is a rare seizure type with a male preponderance. The mean age of onset is 7 years (range: 9 months to 12 years).
Recently, the γ-aminobutyric acid (GABA)A receptor γ-2 subunit mutation R43Q has been reported to be an autosomal dominant mutation associated with childhood absence epilepsy and febrile seizures.62,71 This mutation appears to impair GABAA receptor function by compromising GABAA receptor trafficking and reducing surface expression.62
Anatomic Pathways and Pathophysiology
The current thinking about the pathogenesis of absence seizures dates to the landmark experiments of Jasper and Droogleever-Fortuyn,58 who demonstrated that electrical stimulation of the midline and intralaminar nuclei of the thalamus in cats at a frequency of 3 cycles per second could produce bilaterally synchronous spike-and-wave discharges in the cortical EEG of those animals. The relevance of this finding to human epilepsy was demonstrated in 1953, when Williams,120 utilizing depth-electrode recordings from the thalamus of a child with absence seizures, demonstrated that bilaterally synchronous spike-and-wave discharges with a frequency of 3 cycles per second arose from that structure. During the next 20 years, a debate ensued in the literature as to which region was preeminent in controlling the bilaterally synchronous spike-and-wave discharges characteristic of absence seizures: the cortex,3,70,116 the thalamus,88 or both.43 During the last 10 years, studies using several available animal models of generalized absence seizures coupled with sophisticated in vitro electrophysiologic techniques that allow investigation of cortical and thalamic networks have begun to shed light on the basic neurobiologic mechanisms of generalized absence seizures.
In 2002, Mereen et al., using the WAG/Rij rodent model of typical absence seizures, showed that a functionally intact thalamocortical network is required for the generation of spike-and-wave discharges.75 By investigating the corticothalamic interrelationships in this model with nonlinear association signal analyses of multiple SWDs, those authors showed a consistent focus within the perioral region of the somatosensory cortex. From this focal activity, generalization took place rapidly over the cortex. During the first cycles of the seizure, the cortex appears to drive the thalamus, followed by the cortex and thalamus driving each other, thus amplifying and maintaining the rhythmic discharge.76
The fundamental underlying mechanism of absence seizures involves thalamocortical circuitry and the generation of abnormal oscillatory rhythms from that particular neuronal network.28,29,38,73,74,77 Biochemical mechanisms operative within thalamocortical circuitry during this neuronal oscillation seem to entail phase-locked inhibition mediated by GABAB (γ-aminobutyric acid) alternating with glutamate-mediated excitation. The basic cellular mechanism operative within this tension between excitation and inhibition appears to involve low-voltage activated or T-type calcium (Ca2+) currents, activation of which within thalamocortical circuitry plays a critical role in the development of the thalamocortical network oscillations that underlie absence seizures.23,73 Of the three α1-subunits of the T-type Ca2+ channels, the α1G-subunit is critical to the genesis of spontaneous absence seizures.102,122
Local circuitry within the thalamus may influence the oscillatory rhythms that characterize absence seizures by GABAA-mediated inhibition.55 Pharmacologic factors that play a role external to the thalamocortical circuitry in the genesis of absence seizures include cholinergic, dopaminergic, and nor-adrenergic mechanisms.72 Pathways utilizing these various neurotransmitters project onto the thalamus, cortex, or both from sites distant to those structures and may modulate the process either up or down. Perturbation of one or more of these neuronal networks, particularly those involving the basal ganglia27,99 and the superior colliculus,79 may lead to abnormal neuronal oscillatory rhythms within the thalamocortical circuitry, with resultant generation of the bilaterally synchronous SWDs that characterize generalized absence seizures.100
Although these mechanisms may explain the alteration of consciousness that occurs with absence seizures, the pathophysiologic mechanisms of the motor symptoms that so often accompany absence seizures are not as clear. Many of the mild motor phenomena of absences consist of turning and rotating movements around the vertical body axis, raising and lowering of extremities, or even episodes of decreased tone. These movements belong to the motor activity controlled by the phylogenetically old system that mediates posture and locomotion, the so-called eneirismatic motor system.51 Hassler48,49 has shown that different brainstem structures are involved in the performance of this kind of motor activity. The brainstem, truncothalamic projecting pathways and extrapyramidal cortical areas, supplementary motor area, and anterior part of the gyrus cinguli are all known to play a major role in inciting and coordinating complex movements such as those seen in some types of absence seizures.3,112
Table 1 Clinical features of absence seizures | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
Clinical Features
Ictal
V-EEG split-screen studies of generalized absence seizures show that, in addition to cognitive impairment, staring and a change of facial expression occur in 94% of investigated absence seizures108 (Table 1). Therefore, cognitive impairment, staring, and a change of facial expression represent the most common and important signs of absence and are common to all types of this seizure disorder (Table 1). In an attempt to differentiate absence seizures based on ictal clinical symptomatology, two types have been suggested: type 1 (ocular motor productive) was described in 89% of all absence seizures, and type 2 (nonocular sporadic motor absence) in 11%. The typical ocular motor productive absence seizure was characterized by predominantly ocular motor activity at the beginning of or during the seizure. The motor activity consisted of mild, rhythmic lid or eye clonic activity, tonic retropulsion of the eyes and head, or both. Oral automatisms were often combined with the ocular activity, and if the duration of the absence seizure was prolonged, nonoral (gestural) automatisms sometimes occurred. The motor activity often showed a “march” from ocular or facial regions to the extremities (Fig. 4). The atypical nonocular sporadic motor absence seizure was associated with sporadic myoclonic jerks, primarily of the head and extremities, and occasional oral automatisms.108
In addition to the phenomenologic description of clouding of consciousness during absence seizures, Janz57 described subtle motor symptoms and differentiated absences according
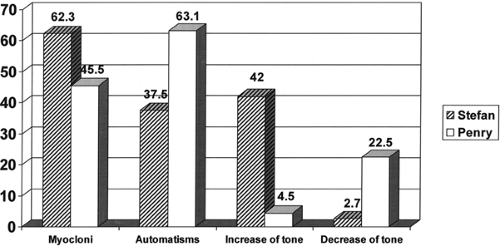
to the direction in which these motor symptoms progressed: retropulsive, propulsive, and adversive absences; those with no predominant direction; and those with no motor symptoms. Up to this time, automatisms had rarely been noted. However, subsequent investigations8,24,40,87,90,103 showed that automatisms were not an uncommon occurrence in absence seizures. Penry et al.87 took a further important step by using V-EEG monitoring to analyze the frequency of different absence components according to the criteria of the International Classification of Epileptic Seizures. V-EEG analysis of absence seizures showed clearly that absences with impairment of consciousness only, so-called simple absences, were rare.53,86,87,107 For example, in 59 patients with 528 absences, only two cases of simple absence were recognized.107 During a simple absence seizure, no ocular movements occur. Absences with ocular movements show mild tonic or clonic movements. In addition to upward ocular movements during an absence seizure, adversive movements of the eyes may occur (mild tonic, clonic, or both). An analysis of ictal signs in typical absence seizures has shown that mild myoclonic or clonic phenomena and automatisms are a common adjunct to clouding of consciousness. The studies of Penry et al. and Stefan et al. are compared in FIGURE 1.
to the direction in which these motor symptoms progressed: retropulsive, propulsive, and adversive absences; those with no predominant direction; and those with no motor symptoms. Up to this time, automatisms had rarely been noted. However, subsequent investigations8,24,40,87,90,103 showed that automatisms were not an uncommon occurrence in absence seizures. Penry et al.87 took a further important step by using V-EEG monitoring to analyze the frequency of different absence components according to the criteria of the International Classification of Epileptic Seizures. V-EEG analysis of absence seizures showed clearly that absences with impairment of consciousness only, so-called simple absences, were rare.53,86,87,107 For example, in 59 patients with 528 absences, only two cases of simple absence were recognized.107 During a simple absence seizure, no ocular movements occur. Absences with ocular movements show mild tonic or clonic movements. In addition to upward ocular movements during an absence seizure, adversive movements of the eyes may occur (mild tonic, clonic, or both). An analysis of ictal signs in typical absence seizures has shown that mild myoclonic or clonic phenomena and automatisms are a common adjunct to clouding of consciousness. The studies of Penry et al. and Stefan et al. are compared in FIGURE 1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree