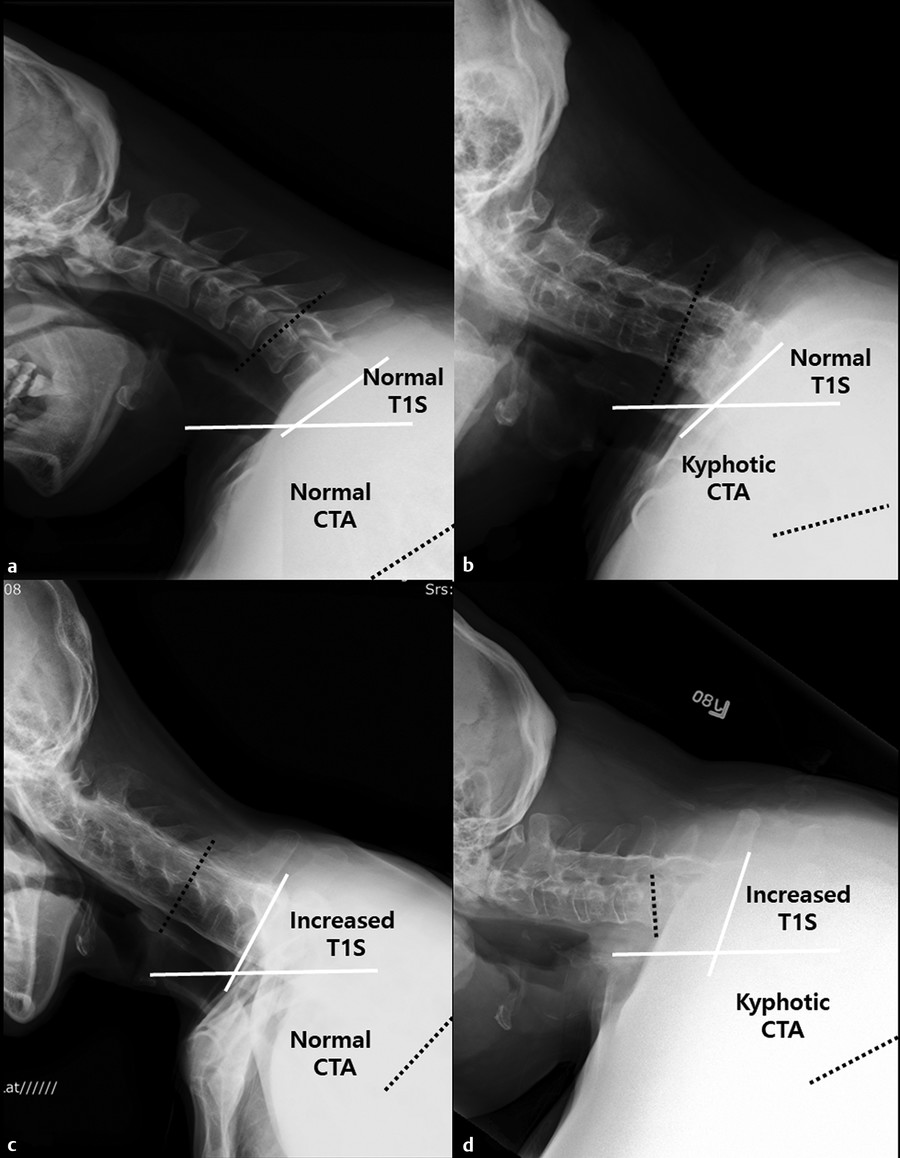
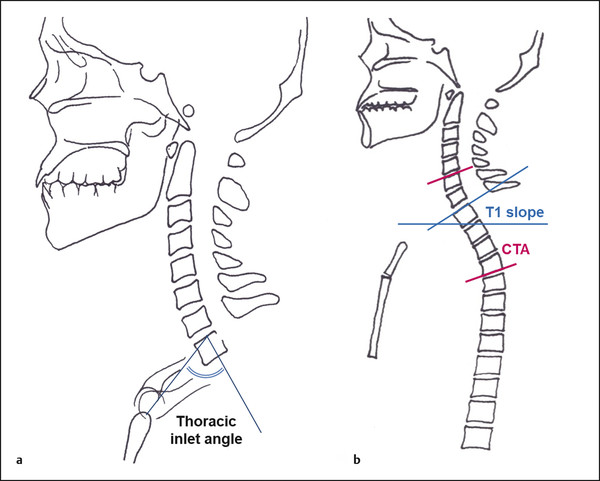
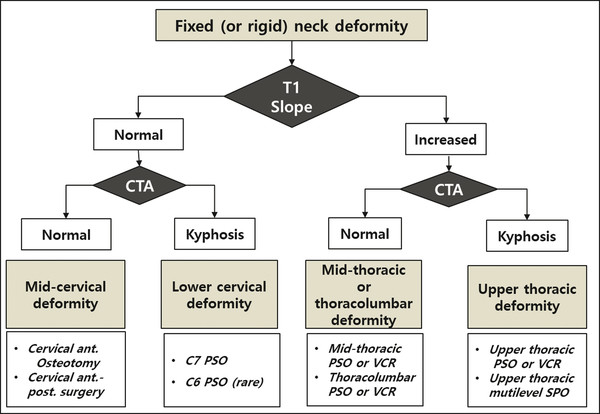
Upper thoracic osteotomy, which is less common than cervical and thoracolumbar osteotomy, can be performed for correction of cervicothoracic junction (CTJ) kyphosis and proximal junctional kyphosis (PJK) after thoracolumbar fusion. Osteotomy at the upper thoracic spine may provide more effective correction of sagittal balance than cervical osteotomy in selected cases and may be performed from T1 to T5, depending on the deformity. 1,2,3,4 The definition of the CTJ varies. It is typically considered the region from C7 to T1 but can be extended to include C6–T4. 5,6,7,8 Compared with kyphotic deformity in the cervical spine, CTJ kyphosis causes greater sagittal imbalance of the cervical spine and more severe clinical problems, including chronic neck pain, inability to achieve a horizontal gaze, and difficulty maintaining hygiene and swallowing. Conventional approaches to CTJ kyphosis correction are lengthening of the anterior column and/or shortening of the posterior column. Although the anterior approach to the cervical spine is easier and safer (to avoid spinal cord and nerve root injuries), access is challenging because of the complex vascular and bony anatomy of the CTJ. In addition, the anterior approach may be impossible in patients with severe kyphotic deformity in the CTJ. Another indication for upper thoracic osteotomy is PJK. Patients with previous thoracolumbar fusion extending to the upper thoracic spine may have PJK and an associated variable degree of cervical spine deformity caused by global sagittal imbalance, spinal compensation mechanisms, underlying cervical spine conditions, and flexibility of the cervical spine. In these cases, upper thoracic osteotomy can correct PJK and the secondary cervical deformity. There are few studies of upper thoracic osteotomy. In addition, there is no consensus on the optimal osteotomy level (lower cervical or upper thoracic spine) and method (three-column osteotomy, including pedicle subtraction osteotomy [PSO]; vertebral column resection [VCR]; or posterior column osteotomy [multilevel Smith-Petersen osteotomy, SPO]). The first case series on upper thoracic osteotomy was reported by Samudrala et al in 2010. 3 They reported the outcomes of osteotomy for surgical correction of CTJ kyphosis. Their cases consisted of PSO at T1 in five patients, at C7 in one patient, at T2–T3 in one patient, and anterior-posterior surgery in one patient. They reported a mean correction of 36 degrees, with excellent clinical outcomes. McClendon et al 2 reported a mean correction of 31 degrees for proximal junctional angles after multilevel SPO for PJK of the upper thoracic spine. Their series consisted of multilevel SPO in six cases and VCR in one case. In a 2015 multicenter study, Theologis et al 4 compared lower cervical osteotomy with upper thoracic osteotomy (T1-T5) for CTJ deformity in 48 patients. They performed PSO or VCR in 24 patients each, C7 osteotomy in 15 patients, and upper thoracic osteotomy in 33 patients (at T1 in 4 patients, T2 in 7, T3 in 9, T4 in 9, and T5 in 4). They reported significant improvements in cervical sagittal vertical axis (SVA), cervical lordosis (CL), Neck Disability Index score, and Scoliosis Research Society domains in both groups, with no significant differences between groups. Reoperation rates were also similar between groups. Indications were not specified. The mean correction of the C2-T1 angle was 44 degrees in the C7 PSO group and 26 degrees in the upper thoracic osteotomy group. Compared with the C7 PSO group, the upper thoracic group had significantly higher changes in T1 slope (20 vs. 3.6 degrees) and SVA correction (2.5 vs. -1.3 cm). Traditionally, the ideal level of osteotomy was considered to be the apex of the deformity. However, spinal osteotomy outside the deformity may be considered for the following reasons: (1) to achieve safer correction at a level where the spinal canal is wider (e.g., C7 or T1 PSO instead of C5 or C6 PSO) or at the level of cauda equina rather than a level of the spinal cord (e.g., L2 or L3 PSO instead of T11, T12, or higher PSO); (2) to achieve more correction angle with the same amount of bone resection (e.g., larger correction angle in SVA at L3 or L4 vs. L1 or L2); or (3) to achieve correction when the deformity involves a transitional area such as the cervicothoracic, thoracolumbar, or lumbosacral segments. Osteotomy in the upper thoracic spine (between T1 and T5) is less commonly indicated than osteotomy in the cervical spine because the apex of cervical deformity is typically at the mid or lower cervical spine segments, and correction is possible within the cervical spine given most cervical deformity is not fixed. However, osteotomy in the upper thoracic spine is an option in the following cases: (1) rigid or fixed cervical deformities with upper thoracic kyphosis (TK), high T1 slope, and/or high thoracic inlet angle (TIA); and (2) cervical deformity combined with upper thoracic PJK in patients with thoracolumbar fusion. In this chapter, we will discuss evaluation of upper thoracic spinal alignment, surgical planning for upper thoracic osteotomy, and surgical techniques. All patients should undergo detailed preoperative radiographic imaging studies, including standing 36-inch anteroposterior and lateral radiographs, as well as routine cervical, thoracic, and lumbar spine radiographs. An additional lateral radiograph including the chin–brow line is needed for patients with severe sagittal imbalance. Computed tomography (CT) and magnetic resonance imaging (MRI) are necessary to evaluate ossification, fusion, and possible spinal canal stenosis with foraminal stenosis. Like all cervical spine deformities, global spinal alignment, including C7 SVA and chin–brow vertical angle (CBVA) should be evaluated. If the cervical deformity is not fixed, C7 SVA and CBVA are less important because compensatory changes will occur in the cervical spine after corrective osteotomy. However, when the patient’s cervical spine has been fused surgically or by ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis, measuring the preoperative CBVA is critical. Overcorrection of the cervical deformity can result in an upward gaze, which is less favorable than undercorrection for activities of daily living such as eating, reading, and walking down stairs. 9 TK, typically measured from the T4 upper endplate to the T12 lower endplate, is one of the baseline angles of thoracic spine alignment. The normal range for TK is 20 to 70 degrees, depending on the patient’s age and lumbopelvic alignment, including lumbar lordosis (LL), pelvic incidence (PI), and sacral slope. 10,11 T1 slope is the angle created by the upper endplate of T1 and the horizontal plane; it is one of the most important parameters, providing the mechanical base of the cervical spine. Patients with a high T1 slope require more CL to obtain a horizontal gaze, and vice versa. Normal values range from 22 to 31 degrees. 12,13 Cervicothoracic angle (CTA) includes both lordotic segments of the lower cervical spine and kyphotic segments of the upper thoracic spine. Normal values of CTA, which is measured from the C6 upper endplate to the T4 lower endplate, have been reported as ranging from 3.9 to 7.2 degrees, with a mean of 4.9 degrees of kyphosis in the middle-aged population; CTA can increase to 23 degrees in those older than 75 years. 7,8 If a patient has cervical kyphosis with normal T1 slope, the deformity is located within the cervical spine. When the cervical deformity is combined with a high T1 slope, high TK, and a kyphotic CTA, an upper thoracic osteotomy is a good option for correction of the deformities in the cervical and thoracic spine (▶ Fig. 14.1a,b). If the deformity shows a high T1 slope, high TK, and a normal CTA, it means the apex of the deformity is in the midthoracic spine. Midthoracic osteotomy below T5 may be considered (▶ Fig. 14.1). However, if the deformity shows high T1 slope but normal TK, it means the deformity is located in the thoracolumbar or lumbar spine, which is an indication for thoracolumbar osteotomy (see ▒Chapter 15░). Fig. 14.1 Radiographs showing four types of fixed cervical kyphosis with similar chin–brow vertical angle and C2–C7 sagittal vertical axis, with different T1 slope (T1S) and cervicothoracic angle (CTA). (a) Patient shows normal T1S and CTA. (b) Patient shows normal T1S and kyphotic CTA. (c) Patient shows increased T1S and normal CTA. (d) Patient shows increased T1S and kyphotic CTA. Surgical treatment strategies would differ in the four patients on the basis of T1S and CTA, even though they have similar chin–brow vertical angles and C2–C7 sagittal vertical axis. Based on the concept of T1 slope, T1 slope minus CL (or C2–C7 angle) is another parameter that reflects the balance between CL and T1 slope to provide information on cervical spine sagittal balance. 12,13,14 It is similar to the concept of PI minus LL in lumbopelvic balance. In the same way that high PI requires a more lordotic lumbar spine to achieve sagittal balance, high T1 slope requires more CL to achieve a horizontal gaze and balanced SVA. Several studies report the ideal value of T1 slope minus CL as 15 degrees and define cervical spine deformity as T1 slope minus CL greater than 20 degrees. 12,14 C2–C7 SVA influences health-related quality-of-life and patient-reported outcomes after surgical treatment. C2–C7 SVA less than 4 cm is associated with disability according to the Neck Disability Index (▶ Fig. 14.2). 12,14,15 Although many studies have analyzed the importance of T1 slope to cervical spine alignment, there are several alignment parameters unexplained by T1 slope alone. First, T1 slope is the angle between the upper end of T1 and the horizontal plane, but is not a constant parameter because it is influenced by global posture. When the patient is sitting, leaning, supine, or prone, TK and T1 slope cannot be used as a predictive parameter for CL. In other words, T1 slope, like sacral slope, is a changing parameter rather than a constant parameter. Anatomically and biomechanically, the cervical spine and cranium are placed on the TIA, a bony circle without range of motion consisting of the T1 vertebral body, the first ribs on both sides, and the upper part of the sternum. The sagittal balance of the cranium and cervical spine, integral to maintaining an upright posture and horizontal gaze, is influenced by the shape and orientation of the TIA in a similar manner to PI in the pelvis. Moreover, important musculature of the neck, including sternocleidomastoid, scalenes, and strap muscles, inserts on the thoracic inlet and several other important cervical paraspinal muscles. TIA is a constant parameter, unaltered by changes in TK. Normal TIA is 70 to 80 degrees. 8,13,16 Upper thoracic osteotomy is an appropriate surgical option for patients with a high TIA and kyphotic CTA. Lower cervical osteotomy is a better option for patients with a normal TIA and kyphotic CTA (▶ Fig. 14.3). Fig. 14.2 Schematic drawing of radiographic measurements of (a) thoracic inlet angle and (b) T1 slope and cervicothoracic angle (CTA). Fig. 14.3 A flowchart for surgical strategy to treat rigid neck deformity using T1 slope and cervicothoracic angle (CTA), which is measured from the C6 upper endplate to the T4 lower endplate. Ant., anterior; post., posterior; PSO, pedicle subtraction osteotomy; SPO, Smith-Petersen osteotomy; VCR, vertebral column resection.
14.2 Indications for Upper Thoracic Osteotomy for Cervical Deformity
14.3 Evaluation of Upper Thoracic Spine Alignment
14.3.1 Global Spinal Alignment and Fusion Status of the Cervical Spine
14.3.2 Thoracic Kyphosis, T1 Slope, and Cervicothoracic Angle
14.3.3 T1 Slope minus Cervical Lordosis, C2–C7 SVA, Thoracic Inlet Angle, and Neck Tilting
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


