CHAPTER 92 VIRAL MENINGITIS AND ENCEPHALITIS
Acute viral infections of the central nervous system (CNS) are normally classified into two clinical syndromes, meningitis and encephalitis, which reflects the anatomical localization of the infection. They are inflammatory conditions of the leptomeninges and brain, respectively. In general, both are caused by the same viral agents, although there is often a propensity for an agent to be more associated with one condition than with the other. Many of these infections are related to neuroinvasion during the course a systemic infection (e.g., arbovirus and enterovirus infections), and only a small subset of patients with the infection actually develops either meningitis or encephalitis. In contrast, rabies virus produces encephalomyelitis and does not cause systemic infection.
EPIDEMIOLOGY
Viral Meningitis
The incidence of aseptic meningitis has been estimated at 10.9 per 100,000 people per year.1 Viral meningitis is more common in men and boys, with a male-to-female ratio of at least 1.5. For reasons that are unclear, the disease is relatively uncommon among people older than 40. There is a striking seasonal incidence, with peak incidence during the months of July, August, and September, which reflects the dissemination of both enteroviruses and arboviruses (see the following sections).
Specific Viral Etiologies
Enteroviruses are ubiquitous, infect individuals of all ages, and cause a wide spectrum of clinical illnesses. Humans are infected by multiple enteroviruses during their lifetime. There is a predominance of enterovirus infections during the summer and fall, although sporadic cases occur all year. Enteroviruses belong to the family Picornaviridae and include the polioviruses, coxsackieviruses, echoviruses, and the numbered human enteroviruses 68 to 71. The enteroviruses are the most common cause of viral meningitis and are responsible for more than 80% of cases in which a specific etiology can be identified.2 Less commonly, enteroviruses cause encephalitis. The enteroviruses replicate in the gastrointestinal tract and are transmitted via the fecal-oral route. Most enteroviral infections are asymptomatic, and gastrointestinal symptoms are usually absent. Recognized cases of viral meningitis represent only a small fraction of enteroviral infections.3 Patients with agammaglobulinemia may develop chronic enterovirus meningitis, and therapy with intravenous immunoglobulin has proved useful in these patients.4,5
Mumps virus was at one time responsible for more cases of viral meningitis than any other single virus. Mumps virus is transmitted via the respiratory route. Outbreaks of mumps peak in the late winter and early spring in northern temperate climates, and major outbreaks traditionally occur at intervals of 2 to 7 years. Mumps virus infection confers lifelong immunity. Mumps virus infection may be associated with parotiditis, orchitis, and deafness. In mumps meningitis, mumps virus may frequently be isolated from the cerebrospinal fluid (CSF). Mumps meningitis has become much less common in the United States since the introduction of live attenuated mumps vaccine in the late 1960s. The Jeryl-Lynn strain of mumps vaccine, which is in trivalent vaccines currently used in the United States, has not been associated with neurological complications. However, the Urabe strain of mumps vaccine, which has been used in other countries, is associated with occasional cases of meningitis.6
Lymphocytic choriomeningitis virus is an arenavirus that causes inapparent infection in rodents and is present in their excreta, and direct contact may result in human infection. In humans, a biphasic illness is common: a mild systemic illness with fever, malaise, and myalgias that improves before the onset of meningitis. Lymphocytic choriomeningitis infection may be associated with severe respiratory symptoms, with pulmonary infiltrates, parotitis, orchitis, or rash.7 Although most cases of lymphocytic choriomeningitis virus infection manifest with meningitis, encephalitis may also occur.
Herpes simplex virus (HSV) type 2 is associated with viral meningitis, particularly at the time of an initial episode of genital herpes infection and especially in girls and women. Meningitis may be preceded by genital or pelvic pain. A minority of these patients go on to have recurrent episodes of meningitis, which may meet the criteria for Mollaret’s meningitis, in which the virus usually cannot be cultured from CSF, but HSV type 2 (occasionally type 1) DNA can often be detected in CSF with polymerase chain reaction (PCR) amplification.8,9
With regard to other viruses, viral meningitis is associated with primary infection with human immunodeficiency virus (HIV) in 5% to 10% of patients, which usually occurs just before the time of seroconversion. Cranial nerve palsies, particularly involving cranial nerves V, VII, and VIII, are more common in HIV meningitis than in viral meningitis with other causes.10 Varicella-zoster virus (VZV) may produce meningitis associated with chickenpox or shingles and rash may not be associated.11,12 PCR amplification is useful in the diagnosis of varicella-zoster virus CNS infections.
Viral Encephalitis
Although many of the same viruses cause viral meningitis and encephalitis, the relative frequencies of the two conditions are different. The incidence of encephalitis has been estimated at 7.4 per 100,000 people per year.1 More than 100 viruses are known to cause acute viral encephalitis, and specific etiological viral agents vary in frequency from year to year13 (Table 92-1). After thorough investigation, one study demonstrated a confirmed or probable viral agent in only 9% of cases of encephalitis, which included those with nonviral causes.14
TABLE 92-1 Significant Causes of Viral Encephalitis in the United States
Adapted from Griffin DE, Inouye RT: Acute viral encephalitis. In Schlossberg D, ed: Current Therapy of Infectious Disease, 2nd ed. St. Louis: Mosby, 2001, pp 270-276.
Specific Viral Etiologies
HSV type 1 is the most common cause of sporadic encephalitis and herpes simplex encephalitis has been identified in about 5% to 10% of cases of acute viral encephalitis in the United States15 with an estimated incidence of about 1 per 250,000 to 500,000 people per year.16 There is no seasonal preponderance or gender predilection. There is a bimodal age distribution in which about one third of cases occur in patients younger than 20 and one half in patients older than 50; this may reflect the occurrence of primary infections in younger individuals and reactivation of latent infections in older patients.17,18 About 90% of cases of herpes simplex encephalitis are caused by HSV type 1, and 10%are caused by HSV type 2.19 Familial herpes simplex encephalitis has been reported infrequently.20
Arboviral infections have a seasonal (usually in the summer and early fall) and geographical distribution that depends on complex ecological cycles between arthropod vectors (mosquitoes and ticks) and their natural hosts. The arboviruses are a biological classification of viruses based on transmission by hematophagous arthropod vectors, and they include viruses in different families, including togaviruses, flaviviruses, bunyaviruses, and reoviruses. Most arboviral infections produce a subclinical or mild clinical illness and go undiagnosed. A minority of patients develop a febrile illness, and a much smaller minority develop encephalitis or, less commonly, meningitis. Epidemics of eastern equine encephalitis are relatively small, with fewer than 35 human cases, and they usually occur in the coastal regions of the eastern United States. Western equine encephalitis occurs in the western United States and in Canada. Venezuelan equine encephalitis has occurred in large outbreaks in Central and South America, and in 1971, a large epidemic in Mexico crossed the Texas border.21 In Venezuelan equine encephalitis, horses are important amplifying hosts, whereas in eastern and western equine encephalitis, horses, like humans, are dead-end hosts. St. Louis encephalitis occurs in both urban and rural outbreaks, and it is an important cause of epidemic encephalitis in North America. In 1975, an epidemic of St. Louis encephalitis included cases in 30 states and in Canada.22 About 25 sporadic cases of Powassan encephalitis have occurred in the northern United States and Canada (Ontario and Quebec).23,24 Powassan virus is transmitted by Ixodes ticks. Most cases of California serogroup encephalitis are caused by La Crosse virus and occur in the central United States. Japanese encephalitis is the most common cause of epidemic encephalitis in the world. Large summer epidemics and endemic disease in Asia are responsible for an estimated 50,000 cases and 15,000 deaths annually.25 Japanese encephalitis virus is transmitted by the mosquito Culex tritaeniorhychnus that breeds in rice fields. Water birds are natural hosts, and pigs may be important amplifying hosts in many countries. In 1999, West Nile virus was responsible for an outbreak of encephalitis in New York City and neighboring counties. The mechanism of introduction of the virus into North America is unknown. The virus has quickly moved across the North American continent. In the United States during 2003, there were 2866 cases of West Nile virus infection causing meningitis or encephalitis and 264 deaths26 (Fig. 92-1). Elderly and immunosuppressed patients are particularly at risk for disease and a fatal outcome. Transmission of West Nile virus may also occur by organ transplantation, infected blood products, and breast milk.
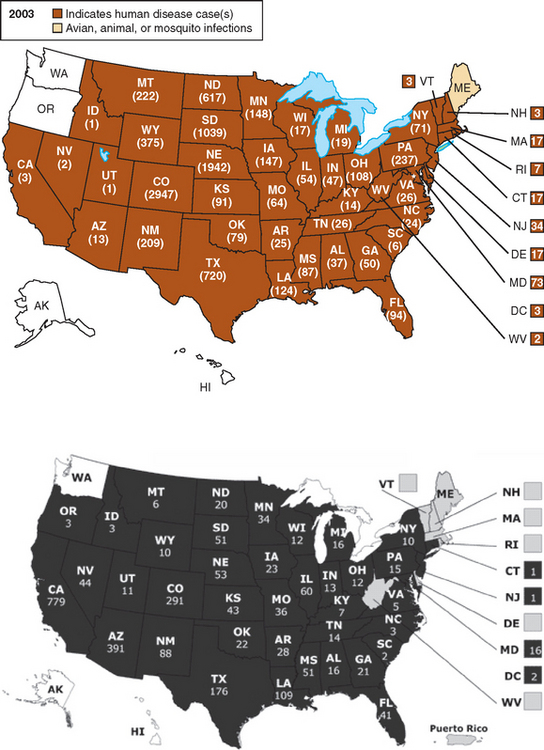
Figure 92-1 Distribution of human cases of West Nile virus infection by state in the United States during 2003 and 2004.
(From the Centers for Disease Control and Prevention, http://www.cdc.gov/ncidod/dvbid/westnilel)
Nipah virus was associated with an epidemic of encephalitis in pig farmers and abattoir workers in Malaysia in 1998 and 1999, which affected 265 people and killed 105.27 Two species of large fruit bats (flying foxes) are the natural hosts of the virus.28 Infected pigs developed respiratory disease and transmitted the virus to humans via the respiratory route, but subsequent outbreaks of Nipah virus encephalitis in Bangladesh and India have not been traced to pig infections.
CLINICAL FEATURES AND INVESTIGATIONS
The diagnosis of viral meningitis or encephalitis can often be made on the basis of the clinical evaluation without specific laboratory or imaging investigations. Patients with viral meningitis have fever, headache, and neck stiffness and rigidity. There is an inflammatory response involving proinflammatory cytokines that play a role in producing fever. The leptomeninges are pain-sensitive structures that account for headache and neck pain and stiffness. Patients may have mild drowsiness, but the level of consciousness is not severely altered, and there are no seizures, focal neurological signs, or other clinical evidence of involvement of the brain parenchyma. In contrast, patients with viral encephalitis have one or more of these features. Some patients with encephalitis have prominent focal features, including hemiparesis or aphasia, whereas others have diffuse brain involvement with depression in the level of consciousness without lateralizing signs. Specific arboviruses are associated with regional involvement of the CNS, including the basal ganglia with Japanese encephalitis virus, the rhombencephalon with West Nile virus, and the spinal cord with tickborne encephalitis virus and West Nile virus.
Examination of the CSF is the mainstay of diagnosis in viral meningitis and encephalitis. In viral meningitis, there is typically mild mononuclear pleocytosis, a normal or mildly elevated protein concentration, and a normal or mildly decreased glucose concentration. In meningitis arising from mumps and lymphocytic choriomeningitis virus infections, the CSF cell counts may be in the thousands. Polymorphonuclear leukocytes may predominate in the CSF, particularly early in the illness. In this case, a repeat examination several hours later usually shows a shift to mononuclear cells.29 Viruses may be cultured from the CSF, or nucleic acids may be detected with PCR amplification techniques. Serological testing may also be helpful for making a specific etiological diagnosis in viral meningitis. Patients with encephalitis should also undergo brain imaging, preferably magnetic resonance imaging (MRI), and CSF examination if there is no concern about brain herniation or other contraindications to lumbar puncture.
Specific Clinical Syndromes
Enteroviral meningitis manifests with fever, headache, and nuchal rigidity, and nausea, vomiting, and photophobia are common. Young children or neonates may exhibit irritability and nonspecific findings. Exanthemata, hand-foot-and-mouth disease, herpangina, pleurodynia, myocarditis, pericarditis, and hemorrhagic conjunctivitis are associated with enterovirus infections. The duration of illness is usually about 1 week, but some symptoms may persist for several weeks, particularly in adults. Serological testing is of only very limited value in enteroviral meningitis because of the large number of enteroviral serotypes. Enteroviruses may be cultured from the oropharynx and stool and also in blood, CSF, urine, and tissues. However, viral growth in culture may take 4 to 8 days, and some enterovirus serotypes grow poorly.30 PCR amplification on CSF for enteroviruses has proved diagnostically superior to viral cultures and has an important effect in reducing the use of antibiotics and in shortening hospitalizations.31 Enteroviruses can also cause encephalitis. In 1998 there was an enterovirus 71 epidemic in Taiwan with many cases of rhombencephalitis.32
Epstein-Barr virus meningitis may occur with or without an infectious mononucleosis syndrome, and meningitis is the most common neurological manifestation of Epstein-Barr virus infection. Encephalitis is less common, and its prognosis is fairly good. Atypical lymphocytes may be present in peripheral blood specimens or in CSF. Epstein-Barr virus is rarely cultured from CSF. PCR amplification may reveal Epstein-Barr virus DNA in the CSF, but the sensitivity and specificity of the test have not yet been determined.33 Serological tests may show evidence of acute Epstein-Barr virus infection with immunoglobulin M (IgM) antibody to viral capsid antigen or with antibody to the diffuse component of the early antigen in association with the absence of antibody to nuclear antigen.34
Herpes simplex encephalitis is characterized by headache, fever, and alteration of consciousness, which may develop over a period of hours or more slowly, over days. Headache is usually a prominent early symptom, and fever is almost always present. Focal neurological features are frequently present, including aphasia, hemiparesis, and visual field defects (superior quadrant). Focal or generalized seizures and olfactory or gustatory hallucinations may occur as well. Behavioral disturbances (sometimes bizarre), personality changes, or psychotic features may occur and be prominent, and psychiatric disease is sometimes suspected. Signs of autonomic dysfunction are also often present. Papilledema is present in a minority of patients. Mild or atypical forms of herpes simplex encephalitis have been recognized without focal features, and they have been associated with both HSV types 1 and 2 infections, immunosuppression with corticosteroids or coexisting HIV infection, or disease predominantly involving the nondominant temporal lobe.35,36 Herpes simplex encephalitis may occur with unusual clinical features, including the anterior opercular syndrome.37
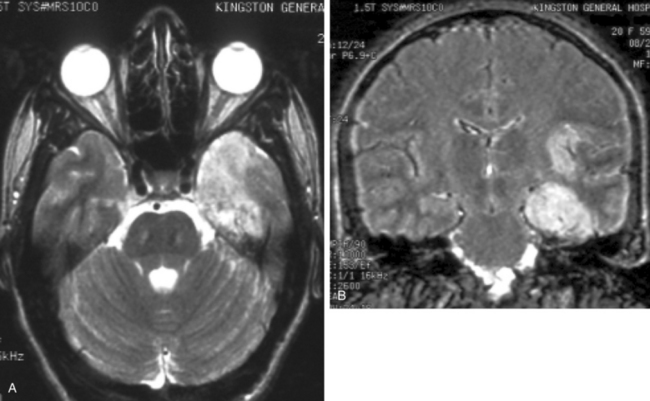
Focal electroencephalographic abnormalities are present in about 80% of cases of herpes simplex encephalitis.38 Sharp- and slow-wave activity is usually localized to the temporal region, and periodic complexes may be present.39 Brain imaging studies, particularly MRI, usually reveal abnormalities in involved areas, including the frontal and temporal lobes, although rare patients with normal MRI studies have been reported.40 Computed tomography reveals hypodense lesions in the temporal lobe and orbitofrontal region, which may demonstrate mass effect, regions of hemorrhage, and irregular contrast enhancement. On MRI, hyperintense signal intensities are typically seen on T2-weighted images in typical sites (Fig. 92-2A), including one or both inferomedial temporal lobes, insular cortex, inferior frontal lobes, cingulate gyrus, and thalamus, with foci of hemorrhage caused by the presence of degradation products of hemoglobin, whereas T1-weighted images show hypointense signal in the same areas, and meningeal enhancement may be demonstrated after administration of gadolinium.41 Fluid-attenuated inversion recovery imaging sequences demonstrate superior definition of temporal lobe abnormalities in comparison with standard T1- and T2-weighted images36 (see Fig. 92-2B). Diffusion MRI studies may also be useful for early detection of lesions.42,43
A lumbar puncture may reveal an elevated opening pressure. CSF examination usually demonstrates a mononuclear cell pleocytosis with mildly elevated protein and normal glucose levels. Pleocytosis is present is about 97% of cases,38 but it may be absent in either immunocompetent44 or immunosuppressed45,46 patients. Leukocyte counts exceeding 500 cells/μL are found in fewer than 10% of patients. Erythrocytes in the CSF in a nontraumatic lumbar puncture are present with similar frequency in patients with encephalitis of other causes.38 HSV can be cultured from CSF in only about 4% of cases.47 A number of reports have demonstrated high sensitivity and specificity of PCR amplification assays for the detection of HSV DNA in the CSF of patients with suspected herpes simplex encephalitis. Primers from a HSV sequence that is common to both HSV types 1 and 2 (either the glycoprotein or HSV DNA polymerase) identify HSV DNA in the CSF.48 CSF specimens from patients with brain biopsy–proved herpes simplex encephalitis and from those with other proved diseases have a diagnostic sensitivity of 98% at the time of clinical presentation, as well as a specificity that approaches 100%.49 False-negative results may occur when there is contamination of CSF by medical or laboratory staff or by the presence of inhibitors. Inhibitory activity for the Taq polymerase used in PCR amplification can be assessed by assays after “spiking” CSF specimens with multiple copies of HSV DNA.49 Inhibitory activity may result from porphyrin compounds from degradation of hemoglobin, or it may be present without any evidence of hemolysis of erythrocytes in the CSF.50,51 The specificity of positive PCR assays can be confirmed with restriction enzyme analysis, hybridization, and sequencing; false-positive results may be a problem in some laboratories.52 If a PCR assay for HSV DNA yields negative results on the first or second day of illness, it should, if clinical suspicion is high, be repeated because results that are initially negative may be followed by positive results on testing of a subsequent CSF specimen.53 The CSF remains positive for HSV DNA by PCR in more than 80% of patients at the end of one week of antiviral therapy.49 Before the development of PCR technology and widespread use of MRI, brain biopsy was an important diagnostic test for herpes simplex encephalitis. The utility of diagnostic brain biopsy for the management of encephalitis is currently controversial, especially in view of empirical antiviral drugs and rivaling sensitivity and specificity of PCR-based assays. At present, diagnostic brain biopsy is normally reserved for only a minority of cases of undiagnosed encephalitis that fail to respond to initial therapy.
Arboviral encephalitis occurs in a minority of patients with arboviral infections, and the majority of patients have inapparent infections or mild nonspecific illnesses. Meningitis is less common than encephalitis. Focal signs are occasionally prominent in arboviral encephalitis. Patients may also have evidence of spinal cord involvement.54,55 Muscle weakness has been noted in patients with West Nile encephalitis, and ventilatory support may be required.56,57 Many cases with muscle weakness have ventral horn cell involvement as a result of the viral infection,55 and rare patients have features of an atypical Guillain-Barré syndrome.58 Movement disorders may occur in Japanese encephalitis59 and West Nile encephalitis.60 Seizures and raised intracranial pressure may be common causes of death.61 Clinical illness usually develops with arboviral infections a few days after transmission of the arbovirus from a mosquito or tick vector. There is a wide range in the severity of encephalitides caused by arboviruses, from mild to severe and fatal. The frequency and severity of neurological sequelae are also variable. Certain arboviruses typically cause more severe disease and higher fatality rates than do others. For example, eastern equine encephalitis virus causes a severe encephalitis with a mortality rate of about 70%. In contrast, La Crosse virus causes a relatively mild encephalitis (California serogroup encephalitis) with a low fatality rate. Arboviruses may cause disease in certain age groups. Encephalitis caused by La Crosse virus usually occurs in children, although infection can occur at any age. Adults in epidemic areas seldom develop Japanese encephalitis because they have developed immunity from childhood infection. Infants often have severe sequelae from western equine encephalitis,62 and elderly patients are more likely to have more severe disease in St. Louis encephalitis63 and West Nile encephalitis. In West Nile encephalitis, there is an associated broad spectrum of neurological involvement, including meningitis, cerebellar disorder, myelitis, and parkinsonism and other movement disorders.60
Computed tomography or MRI scans have demonstrated lesions in the basal ganglia, thalamus, and brainstem in eastern equine encephalitis.64 MRI scans in Japanese encephalitis show lesions in the thalami in most patients and also lesions in the basal ganglia, midbrain and pons, cerebral cortex, and cerebellum.65,66 MRI lesions may be present in the thalamus, basal ganglia, and brainstem in tickborne encephalitis.67 A minority of patients with West Nile encephalitis have MRI abnormalities, and these often involve the basal ganglia, thalamus, and brainstem.60 There is usually pleocytosis with a modest number of leukocytes that are predominantly mononuclear cells. CSF protein levels are often elevated, but the CSF glucose level is usually normal. Viral cultures on CSF for arboviruses usually yield negative results, although Japanese encephalitis virus may be isolated from CSF in up to one third of patients.68 Venezuelan equine encephalitis virus, tickborne encephalitis viruses, and Colorado tick fever virus may be isolated from blood.69,70 Arboviruses may be cultured from the brain and spinal cord in fatal cases. In rare cases, a diagnosis may be made by using brain biopsy.71 Most arboviral infections are diagnosed serologically. A serological diagnosis is commonly made on the basis of a fourfold or greater rise (or fall) in the titer of viral antibodies (immunofluorescent, hemagglutination inhibition, complement fixation, or neutralizing) during the infection. Both acute and convalescent sera should be obtained, the latter 2 to 6 weeks after the first. Serological cross-reactions can occur in areas where closely related viruses (e.g., flaviviruses) circulate or when patients have been vaccinated against a closely related virus.28 This problem can be resolved by parallel serological testing against the closely related viruses or by further assessment at a specialized laboratory with plaque reduction neutralization assays. The presence of viral specific serum IgM indicates primary infection, although IgM may remain present for many weeks. A diagnosis may be made at the time of admission to the hospital or soon afterward by demonstration of virus-specific IgM in the CSF by capture enzyme immunoassay.72,73 About one half of patients with West Nile encephalitis have IgM in CSF on admission to the hospital, and the majority develop IgM by the seventh day of admission; patients who do not develop IgM are more likely to have West Nile virus isolated and are more likely to die of the illness.74 Assays with PCR amplification may be useful in detecting viral RNA from arboviruses in CSF or brain tissues.75–77 In West Nile encephalitis, real-time PCR, the most sensitive of PCR techniques, is positive in only about one half of cases.74
Nipah virus encephalitis in Malaysia was characterized by fever, altered mental status, segmental myoclonus, seizures, cerebellar ataxia, and brainstem and cervical spinal cord signs, and there was a high mortality rate.78 T2-weighted MRI revealed multiple small, hyperintense lesions in brain white matter.79 CSF demonstrated pleocytosis and elevated protein levels.78 Pathological studies revealed infection of endothelial cell and neurons and microinfarctions caused by small vessel vasculitis in both the gray and white matter.80,81
Rabies usually develops 1 to 3 months (or, rarely, a few days or more than a year) after exposure, which is most often from an animal bite. However, there may be no history of an animal bite, particularly in association with transmission from bats. Patients with rabies often have distinctive clinical features,82 but physicians must have a high index of suspicion. Prodromal symptoms, including fever, chills, malaise, fatigue, insomnia, anorexia, headache, anxiety, and irritability, may last for a few days. About one half of patients develop pain, paresthesias, or pruritus at or close to the bite site, which may reflect infection in dorsal root ganglia. About 80% of patients develop an encephalitic (also called furious) form of rabies, and 20% develop a paralytic form. In the encephalitic form, patients have episodes of generalized arousal or hyperexcitability, which are separated by lucid periods.83 They may have aggressive behavior, confusion, and hallucinations. Fever is common, and signs of autonomic dysfunction, including hypersalivation, sweating, and piloerection, may be present. Nuchal rigidity and seizures may occur. About one half of patients develop hydrophobia, a characteristic manifestation of rabies (Fig. 92-3). Patients may initially experience pain in the throat or have difficulty swallowing. On attempts to swallow, they experience contractions of the diaphragm and other inspiratory muscles, which last for about 5 to 15 seconds. Subsequently, the sight, sound, or even mention of water (or of any liquids) may trigger the spasms. A draft of air on the skin may have the same effect (aerophobia). The disease may progress through paralysis, coma, and multiple organ failure, and eventually it causes death. In paralytic rabies, flaccid muscle weakness develops early in the course of the disease, and patients may survive longer.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree