8
What Can Neuroimaging Tell Us?
Introduction
Brain imaging of patients with epilepsy relies heavily on methods that detail normal brain structure and pathology. Magnetic resonance imaging (MRI) is the modality of choice in both new-onset seizures and chronic epilepsy. Unique MRI imaging techniques and functional brain imaging with both nuclear medicine and fMRI methods are important when considering epilepsy surgery.
Imaging in the initial evaluation of epilepsy
Structural imaging is important for evaluation, management, and treatment of the person with epilepsy. MRI is the imaging modality of choice because of superior anatomic resolution, excellent characterization of pathological processes, and lack of ionizing radiation. Imaging is indicated in most but not all patients with epilepsy. The indications for imaging include clinical or electroneurodiagnostic findings consistent with focal or secondarily generalized seizures, abnormal neurological examination or physical findings, and epilepsy onset in children under 2 years of age. Imaging is not indicated in patients with a normal neurological exam and electroneurodiagnostic findings of certain epilepsy syndromes. These include benign epilepsy of childhood with centrotemporal spikes, childhood absence epilepsy, juvenile absence epilepsy, and juvenile myoclonic epilepsy. Multispecialty practice parameters for obtaining neuroimaging in patients presenting emergently with seizures are presented in Table 8.1.
The role of structural neuroimaging is to detect an underlying cerebral abnormality that may be causally related to the epilepsy or comorbid cognitive, neurological, or psychological impairment. In the pediatric age group, nearly 50% of patients with new-onset focal seizures have abnormal imaging; in 15–20% of the total, the apparent cause of the epilepsy is found. In series of adults with chronic epilepsy, high-resolution MRI enables the apparent cause to be found in more than 50%. By contrast, past studies of CT imaging of patients presenting with first-time seizures in the emergency department have shown that this procedure will demonstrate findings that change acute management in 9–17% of adults and in 3–8% of children. MRI is now recommended as the first-line imaging study in new-onset seizures in children and most adults because of increased availability, better resolution and sensitivity, and increasing concern about the risks of ionizing radiation.
Imaging early in the evaluation of epilepsy is directed at detecting a cause that might require urgent medical or surgical treatment. That is, certain acute or subacute processes such as tumor, acute stroke or hemorrhage, encephalitis, leukodystrophy, hydrocephalus, or findings suggesting a metabolic or neurogenetic disorder will direct further diagnostic evaluations and acute treatments. Central nervous system (CNS) infections from parasitic disorders such as cysticercosis are a common cause of epilepsy in many areas of the world and require concomitant treatment of the infection and epilepsy.
Table 8.1. Guidelines for neuroimaging in patient presenting with emergent seizures.
| Category | First-time seizure | Recurrent seizures |
| Emergent Serious structural lesion suspected Immediate imaging | New focal deficits, persistent altered mental status (with or without intoxication), fever, recent trauma, persistent headache, history of cancer, history of anticoagulation, or suspicion of AIDS | New focal deficits, persistent altered mental status (with or without intoxication), fever, recent trauma, persistent headache, history of cancer, history of anticoagulation, or suspicion of AIDS |
| Also considered if age > 40 years or focal-onset seizure | Also considered if new seizure pattern or seizure type or prolonged postictal confusion or worsening mental status | |
| Urgent Possible structural lesion Imaging appointment included in disposition or before disposition when followup not assured | No clear-cut cause identified (e.g., hypoglycemia, hyponatremia, tricyclic overdose) | No clear-cut cause has been identified (e.g., hypoglycemia, hyponatremia, tricyclic overdose) |
| Not indicated Imaging not performed or scheduled | Typical febrile seizures | Typical febrile seizures or typical recurrent seizures related to previously treated epilepsy |
Reproduced with permission from Quality Standards Subcommittee of the American Academy of Neurology in cooperation with American College of Emergency Physicians, American Association of Neurological Surgeons, American Society of Neuroradiology. Practice parameter: Neuroimaging in the emergency patient presenting with seizure – summary statement. Neurology 1996; 47(1):288–291.
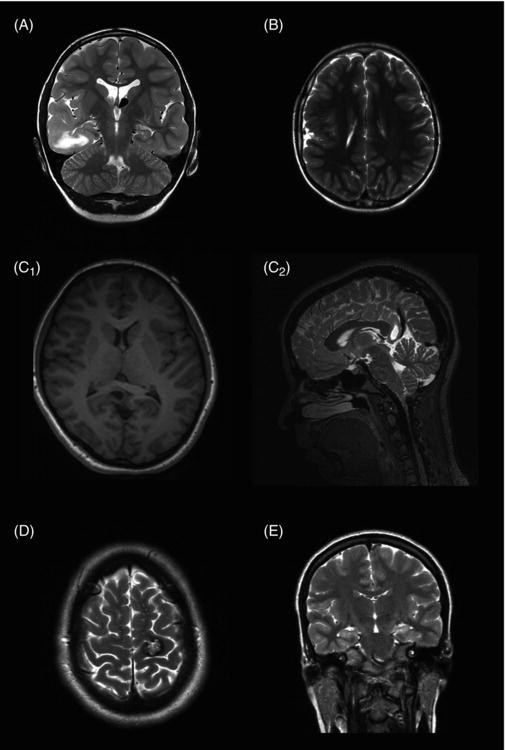
Imaging can also identify chronic symptomatic lesions such as encephalomalacia, porencephalic cysts, and atrophy, which are due to remote traumatic brain injury, stroke, perinatal injury, or CNS infections (Figure 8.1). Other chronic pathologies (Figure 8.1) include malformations of cortical development (MCD), focal cortical dysplasias (FCD), vascular malformations, and mesial temporal sclerosis. More severe malformations such as holoprosencephaly, lissencephaly, schizencephaly (Figure 8.1), and hemimegalencephaly (Chapter 3) often present with severe epilepsy in early childhood. New knowledge about the molecular neurobiology of brain development has resulted in modification of the classification of MCD (Chapter 3) and new molecular diagnostic tests. FCD is secondary to abnormal postmigrational development and can result from injury during later stages of brain development, and it is potentially amenable to epilepsy surgery (Chapter 27). It can also be associated with other vascular lesions and neoplasms, such as gangliogliomas or dysembryoplastic neuroepithelial tumors, and with genetic disorders such as tuberous sclerosis.
Hippocampal sclerosis (HS, Figure 1, Chapter 3) is one of the most important structural abnormalities associated with chronic epilepsy in older children and adults. The MRI shows decreased hippocampal volume with loss of internal architecture and increased signal intensity on T2-weighted images. There is often additional atrophy of adjacent temporal structures (mesial temporal sclerosis). Detection of these findings often requires thin-slice coronal images of the temporal lobes and is important because the epilepsy associated with HS is most often pharmacoresistant but has an excellent chance of control with neurosurgery (Chapter 27).
Figure 8.1. Imaging abnormalities associated with epilepsy. (A) Patient with right temporal lobe epilepsy due to tuberous sclerosis. Coronal T2-weighted image showing large cortical tuber with increase in T2 signal in white matter and distortion of gyral and sulcal pattern of anterior temporal lobe. Also a calcified, subependymal nodule is noted near the foramen of left lateral ventricle. (B) Patient with symptomatic focal motor and secondarily generalized seizures with schizencephaly of right frontoparietal region with polymicrogyria involving region near central sulcus observed on T2-weighted axial image. (C1 and C2) Patient with pharmacoresistant focal seizures with semiology suggestive of temporal lobe seizures showing a cystic lesion in medial parietooccipital region. C1 is a sagittal T2-weighted image demonstrating the cystic lesion arising from the posterior cingulate gyrus and posterior to the splenium of the corpus callosum. C2 is an axial T1-weighted image showing lesion arising from the right hemisphere. The lesion was identified as an oligodendroglioma on pathology following surgical removal. (D) Patient with focal motor seizures due to cavernous vascular malformation seen on axial T2-weighted image. Hemosiderin is observed surrounding the lesion. (E) Patient with focal seizures with oromotor automatisms, behavioral arrest, and irregular motor movements. Image demonstrates mesial temporal sclerosis in left temporal lobe on coronal T2-weighted image demonstrating increase in T2 signal and smaller hippocampus compared to the opposite side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


