28
When Should Vagus Nerve Stimulation Be Considered, and What Can It Accomplish?
Introduction
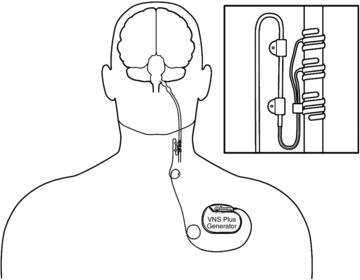
Approximately 70% of people with epilepsy can be successfully treated with one or two antiepileptic agents, but the remaining 20–30% have recurrent seizures and are considered refractory to medications. Although a proportion of these patients are resective epilepsy surgery candidates, many are not. It is this group of patients who may benefit from vagus nerve stimulation (VNS). VNS uses an implantable neuromodulatory device as adjunctive therapy for refractory epilepsy. The device (developed by Cyberonics in Houston, Texas) consists of a small, programmable pulse generator that is placed subcutaneously in the left upper thoracic area and connected by a bipolar lead to the left cervical vagus nerve trunk. The implanted generator delivers intermittent electrical stimulation or pulses to the left vagus nerve at programmed intervals and intensities. Additionally, it can be activated by a magnet that can be used by the patient or family member at the onset of a seizure to help stop or alter the seizure’s natural course. This chapter describes who should be considered for VNS therapy and discusses its effectiveness, technical considerations, and common adverse reactions.
 SCIENCE REVISITED
SCIENCE REVISITEDPatient selection
Vagus nerve stimulation is an adjunctive treatment for patients with medically refractory epilepsy who are not resective surgery candidates. Therefore, patients with epilepsy who have failed adequate trials of several antiepileptic drugs (AEDs) should be considered for nonpharmacological therapies such as VNS – Chapter 14 suggests failure of five or six AEDs as the criterion. The evaluation to determine the appropriateness of VNS should consist of EEG, MRI, and in many cases long-term video–EEG monitoring. The goal of this evaluation is to ensure that the patient is not an appropriate candidate for epilepsy surgery.
Vagus nerve stimulation was initially approved in the USA by the FDA in 1997 for use in medically refractory focal onset (localization-related) epilepsy in people 12 years and older. However, it should also be considered in the treatment of refractory generalized epilepsies. In Lennox–Gastaut syndrome (LGS) and other symptomatic generalized epilepsies, seizure frequency is reduced by more than 50% in about half of the patients. The most dramatic reduction is with generalized tonic–clonic (GTC) and absence seizures. Although there is evidence, albeit from smaller studies, for a similar reduction in seizure frequency for patients with primary or idiopathic generalized epilepsies, VNS for these patients is not universally accepted. Additionally, patients who have undergone epilepsy surgery and have failed to obtain adequate response can be considered for VNS therapy.
In addition to the effectiveness of VNS for the broad spectrum of epilepsies, there is evidence for its effectiveness in the pediatric population younger than 12 years. Evidence shows significant seizure reduction in pediatric epilepsy populations equal to and in some cases better than reduction in the adult epilepsy population. In summary, many patients with refractory epilepsy who either are not good epilepsy surgery candidates or have failed epilepsy surgery can be considered for VNS implantation.
 TIPS AND TRICKS
TIPS AND TRICKSEffectiveness of VNS
Seizure freedom after placement of a VNS is rare (<10%). Almost all patients in whom a VNS is implanted still require continued AEDs to maintain seizure reduction. VNS typically produces a significant (>50%) reduction in seizure frequency for 20–65% of patients. At least 20–25% of patients will have little change in seizures. Other benefits reported with VNS in some patients include a decrease in seizure severity or in the duration of the postictal period. There is also potential for reduction in other severe epilepsy-related clinical events including convulsive status epilepticus, fractures, and traumatic head injuries.
The secondary benefits of VNS that have been shown to occur independent of seizure frequency reduction include a positive effect on mood and improved quality of life.
Device and implantation
The device is titanium encased and small (about 4 cm across), comparable in size to a silver dollar or pocket watch. It includes the pulse generator and a lithium battery. There is an attached lead wire with a flexible spiral end that encircles the left cervical vagus nerve (Figure 28.1).
The surgery is performed under local or general anesthesia. The wires are connected to the left vagus trunk due to concern of the possibility of bradycardia with stimulation of the right vagus nerve. Usually two small incisions are made in the left neck and left upper chest area. The device is implanted superficially below the clavicle, and the tethering or coiling of the electrode around the left vagus nerve trunk is done via the neck incision. The operative time is about 60–90 min. Usually, patients will be discharged on the same day; however, some patients may be kept overnight for observation. Surgical complications such as infection (<~1.6%) are rare. One possible complication is vocal cord paresis or paralysis from temporary or permanent injury during surgery of the recurrent laryngeal nerve, a branch of the left vagus. If this untoward event is noted in the immediate postoperative period, the patient should be reassured that permanent paralysis is unusual (<0.2% of cases) and that the condition is likely to improve with time.
Technical considerations
The VNS system consists of a handheld “wand” connected to a portable display device that can be made to interface with the generator simply by holding the interrogating “wand” over the left chest where the generator is implanted. The system can be turned on in the operating room immediately after the surgery or during the immediate postoperative office checkup. The display device has software for the detection and manipulation of the stimulation parameters. There are several stimulation parameters, five of which can be set and modified by a practitioner (usually a neurologist or supervised nurse practitioner or physician’s assistant) during routine office visits to optimize activation of the vagus nerve. The most common settings that are adjusted are the stimulation amplitude, signal frequency, pulse width, and signal ON and OFF times (duty cycle) (see Table 28.1).
Figure 28.1. Schematic of the impulse generator placed in the superficial left infraclavicular chest with bipolar leads that terminate in spirals around the cervical trunk of the left vagus nerve in the neck. The pulse generator can be palpated and the programming wand placed over the area to interrogate the device. Figure modified from original drawing provided by Cyberonics, Inc., with permission.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


