Case 105 Ulnar Nerve Compression at the Elbow
Stephen M. Russell
Fig. 105.1 A patient with severe left ulnar nerve entrapment at the elbow with clinical signs shown in (A–C). See Answer section for further description.
- A 50-year-old woman presents with 6 weeks of elbow pain localized to the left medial epicondyle.
- It began after a prolonged period of holding the telephone with the affected hand.
- A few days later she woke one morning with complete numbness in the small finger.
- Then over the ensuing weeks, she developed progressive hand atrophy, weakness, and incoordination.
- Her examination reveals dense numbness to light touch and pinprick on the hypothenar eminence (including the dorsum of the hand in this area), as well as the small finger and adjacent half of the ring finger.
- Severe atrophy of most hand intrinsic muscles is noted.
- Tapping in the retrocondylar groove causes paresthesias to occur in the small finger. Figure 105.1 illustrates the patient’s hands.
- She has no neck pain and no Spurling sign.
< div class='tao-gold-member'>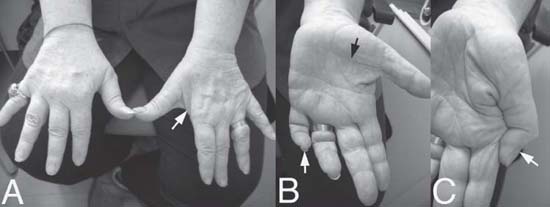
 Clinical Presentation
Clinical Presentation Questions
Questions Answers
Answers


