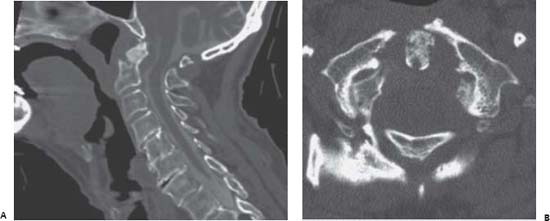
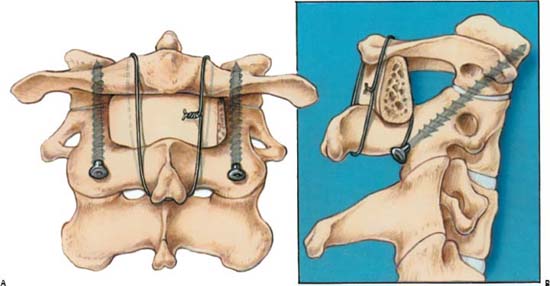
Case 82 Atlantoaxial Instability Fig. 82.1 (A) Sagittal computed tomography (CT) reconstruction with myelographic subarachnoid contrast injection. (B) Axial CT nonmyelogram cut at the level of C1 through the dens. Fig. 82.2 Artist’s rendering of ideal trajectory of C1–C2 transarticular screws with (A) anteroposterior and (B) lateral illustrations. Posterior wiring with interspinous iliac graft is also depicted. Note that the posterior wiring of C1 to C2 may require a structurally intact arch of C1 and may not be feasible in some cases of Jefferson fracture (such as possibly in this case). (From Wolfla CE, Resnick DK. Neurosurgical Operative Atlas. Spine and Peripheral Nerves. New York: Thieme/American Association of Neurological Surgeons; 2006. Reprinted with permission.)
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
82 Atlantoaxial Instability
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


