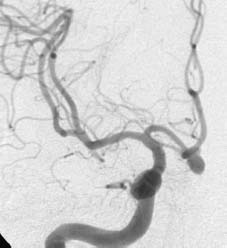
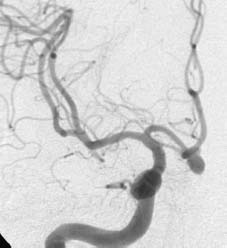
Case 30 Subarachnoid Hemorrhage and Vasospasm Qasim Al Hinai, Claude-Edouard Chatillon, David Sinclair, and Denis J. Sirhan Fig. 30.1 Computed tomography of the head axial cut through basal cisterns. Fig. 30.2 Cerebral angiogram, anteroposterior view, right carotid injection. Fig. 30.3 Cerebral angiogram, antero-posterior view, right carotid injection, performed 6 days later, after a therapeutic intervention. The patient was admitted to the intensive care unit (ICU) and underwent a therapeutic procedure for the fnding on the previous angiogram. Six days later, the patient developed dysphasia and right-sided hemiparesis (right leg is weaker than right arm). A CT of the head reveals a right frontal hypodensity with surrounding mild edema.


 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
30 Subarachnoid Hemorrhage and Vasospasm
Case 30 Subarachnoid Hemorrhage and Vasospasm Fig. 30.1 Computed tomography of the head axial cut through basal cisterns. Fig. 30.2 Cerebral angiogram, anteroposterior view, right carotid injection. Fig. 30.3 Cerebral angiogram, antero-posterior view, right carotid injection, performed 6 days later, after a therapeutic intervention.


 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


