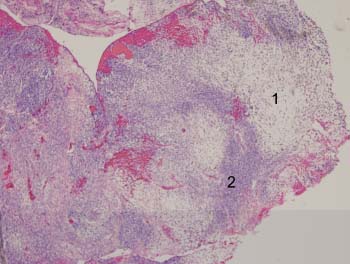
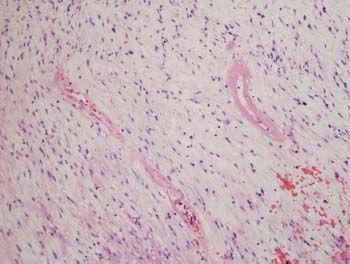
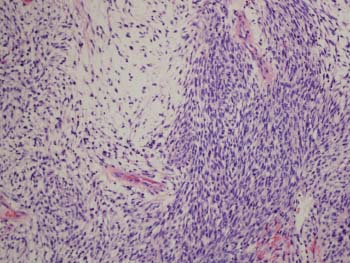
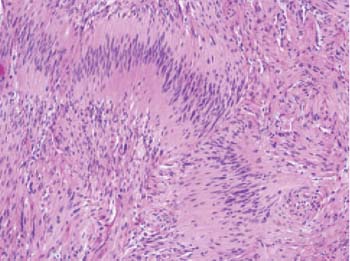
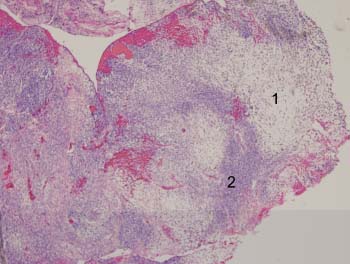
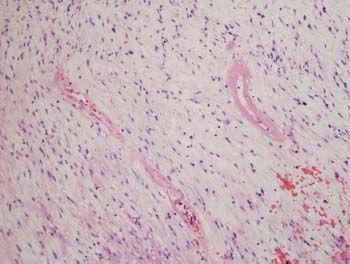
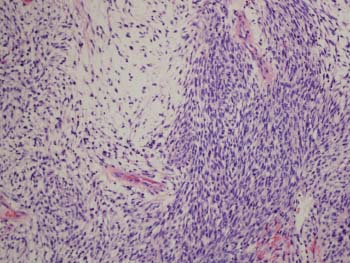
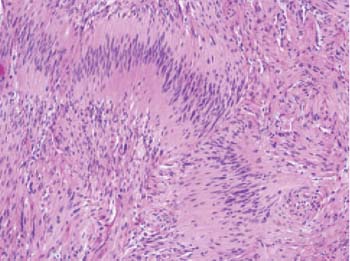
Case 106 Lower Extremity Peripheral Nerve Sheath Tumor Robert L. Tiel Fig. 106.1 T1-weighted contrast-enhanced magnetic resonance image of a schwannoma. Note widening of the nerve. Fig. 106.3 High magnification (200×) of area 1 (H&E) stained). Fig. 106.4 High magnification (200×) of area 2 (H&E stained). Fig. 106.5 High magnification (200×) of tumor pathology (H&E stained).
 Clinical Presentation
Clinical Presentation
 Questions
Questions

 Answers
Answers
106 Lower Extremity Peripheral Nerve Sheath Tumor
Case 106 Lower Extremity Peripheral Nerve Sheath Tumor Fig. 106.1 T1-weighted contrast-enhanced magnetic resonance image of a schwannoma. Note widening of the nerve. Fig. 106.3 High magnification (200×) of area 1 (H&E) stained). Fig. 106.4 High magnification (200×) of area 2 (H&E stained). Fig. 106.5 High magnification (200×) of tumor pathology (H&E stained).
 Clinical Presentation
Clinical Presentation
 Questions
Questions

 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


