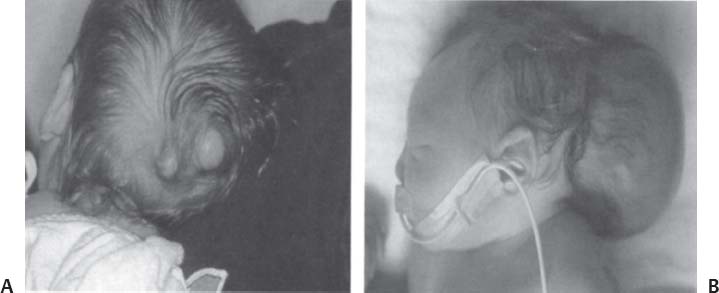
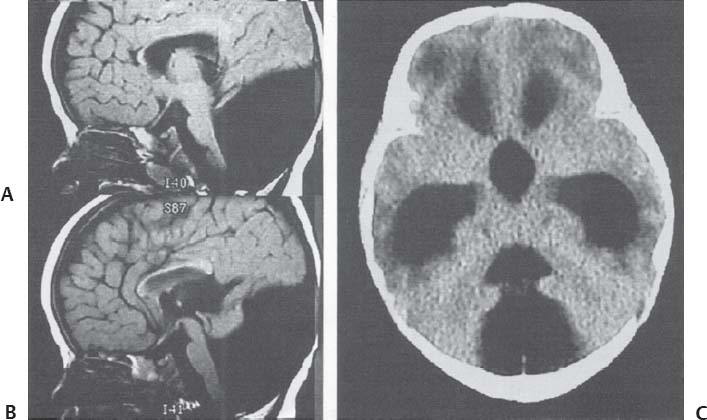
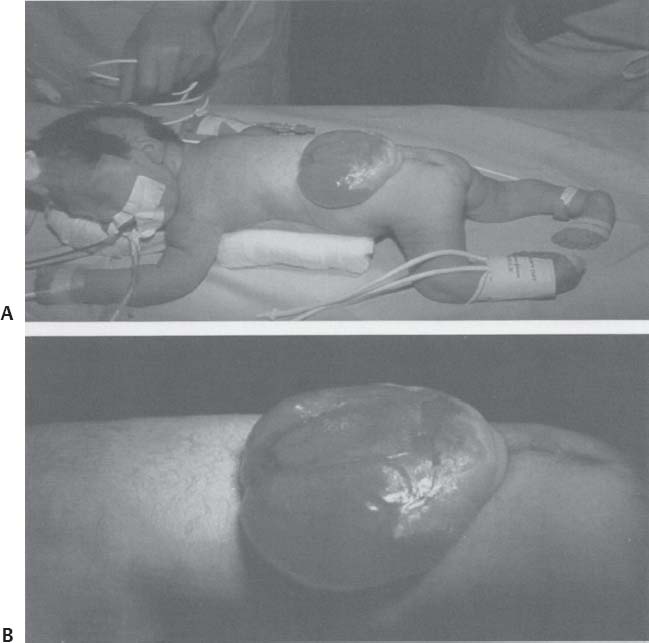
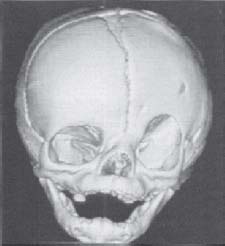
C H A P T E R 11 CONGENITAL AND PEDIATRIC LESIONS I. ARACHNOID CYST—frequently associated with subdural hematomas A. Treatment—only if symptomatic 1. Craniotomy and fenestration into medial CSF casterns (consider a shunt if this fails) 2. Consider endoscopic third ventriculostomy and fenestration for a suprasellar cyst. II. NEURENTERIC CYST—lined by gastrointestinal or respiratory endothelium and usually occurs in the cervical or thoracic spine A. Treatment—resection is required. III. ENCEPHALOCELE—most children do not develop normally. A. Cranial vault (occipital)—most common variety in the Western hemisphere 1. Treatment—excision and closing of dura (Fig. 11.1A,B) B. Sincipital—nasofrontal, nasoethmoidal, and nasoorbital C. Basal—transethmoidal, transsphenoidal, sphenoethmoidal, and sphenoorbital. There is no visible mass. 1. Treatment—combination nasal and subfrontal closure IV. CHIARI MALFORMATION Fig. 11.1 Encephaloceles. (A) Two small occipital encephaloceles. (B) Large occipital encephalocele. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 7, Fig. 4.) A. Type 1—cerebellar tonsil herniation 5 mm below foramen magnum (varies with age); presentation is usually around 40 years. 1. Signs/Symptoms—headaches, paresthesias, or syringomyelia 2. Treatment—suboccipital craniectomy and C1 laminectomy with duraplasty (Fig. 11.2) B. Type 2—always present at birth if the patient has a myelomeningocele (MM) 1. Signs/Symptoms—due to brainstem and cranial nerve (CN) dysfunction (dysphagia, stridor, apnea, and nystagmus) 2. Evaluation—magnetic resonance imaging (MRI) shows vermis herniation with tectal beaking, elongated medulla, hydrocephalus (HCP), and bony abnormalities 3. Treatment—initially with a ventriculoperitoneal (VP) shunt; 20% will eventually require a suboccipital decompression (Fig. 11.3) V. DANDY—WALKER MALFORMATION A. Cause—atresia of the foramen of Magendie and Luschka with agenesis of the vermis and a posterior fossa cyst communicating with a large fourth ventricle Fig. 11.2 Chiari 1 malformation. Sagittal T1-weighted magnetic resonance image demonstrates peglike tonsils extending below foramen magnum with an associated syrinx. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 13, Fig. 11.) Fig. 11.3 Chiari 2 (Arnold-Chiari) malformation. Sagittal T1-weighted magnetic resonance image with tectal beaking, lowlying torcula, and vermian descent. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 13, Fig. 12.) Fig. 11.4 Dandy—Walker malformation. (A,B) Sagittal T1-weighted magnetic resonance images and (C) axial computed tomography scan demonstrate vermian agenesis and connection of fourth ventricle to posterior fossa cyst. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 15, Fig. 15.) B. Signs/Symptoms—associated HCP (90%) as well as cardiac and multiple other abnormalities; 50% of patients have normal IQs. C. Treatment—shunting the cyst (Fig. 11.4A–C) VI. AQUEDUCTAL STENOSIS A. Treatment—VP shunt or third ventriculostomy VII. MYELOMENINGOCELE (Fig. 11.5A,B) A. Facts—80% have HCP, most have Chiari 2 malformation, 80% have normal IQ, and 10% have normal urinary continence B. Prevention 1. Folic acid supplements during the first trimester 2. Avoid valproic acid, saunas, and hot tubs in the first trimester Fig. 11.5 Myelomeningocele. (A) Neural placode noted on center of dorsal aspect. (B) Closeup image. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 7, Fig. 3.) C. Evaluation 1. 3% risk after a prior abnormal birth 2. Maternal serum α fetal protein (AFP), ultrasound, and amniocentesis for AFP 3. Evaluate the child for spontaneous leg movement, scoliosis, hip and knee abnormalities (x-rays) 4. Genitourinary evaluation—15% have abnormalities such as one kidney or a horseshoe kidney; perform a straight catheterization. 5. Cardiac echo—15% have abnormalities such as atrial or ventricular septal defects. 6. Head ultrasound—most have HCP. D. Treatment—85% survival 1. Cover the lesion with Telfa and sponges soaked with normal saline (consider connecting intravenous (IV) tubing running at 5 mL/h to the gauze) 2. Maintain prone Trendelenburg position 3. If ruptured, use nafcillin and gentamicin until 6 hours after closure. 4. If unruptured don’t use antibiotics 5. Closure within 24 hours 6. If no HCP by ultrasound and occipital-frontal circumference (OFC) measurements, repair the MM and shunt in 3 days if needed 7. If there is HCP, operate in the prone position with the head turned a. Shunt the ventricles to the peritoneum via the flank b. Begin MM repair by isolating the placode and removing the tissue between the placode and skin c. Suture the cord into a cylinder d. Close the dura, fascia, and skin e. Complications include shunt malfunction, syrinx, and tethered cord. f. There is no proof that birth by C-section alters outcome. VIII. LIPOMYELOMENINGOCELE—skin-covered lesion A. Signs/Symptoms—most have cutaneous stigmata of spina bifida such as a hair patch, dimple, or red mark B. Evaluation—MRI C. Treatment 1. Untether the cord and debulk the fat 2. Use intraop somatosensory evoked potential (SSEP) and nerve root stimulation 3. Surgical outcome—unchanged (75%), improved (20%), worse (5%) IX. DERMAL SINUS TRACT A. Signs/Symptoms 1. Cutaneous indication is a dimple with hair. 2. Often meningitis B. Evaluation—MRI and x-ray (to find spina bifida) C. Treatment—repair with resection of tract and dural closure X. TETHERED CORD—low-lying conus below L2 with thickened filum or mass; frequently associated with MM; cutaneous manifestations in 50% A. Signs/Symptoms—gait dysfunction (90%), sensory loss (70%), bladder dysfunction (40%), scoliosis, pain B. Evaluation—cystometrogram, x-ray (spina bifida is seen in 98%), MRI C. Treatment—stimulate the filum before sectioning. 1. Filum terminale is whiter than the nerve roots and has ligamentous fibers with a squiggly vessel on the surface. 2. Intraop anal sphincter electromyogram (EMG) XI. DIASTEMATOMYELIA—spinal cord split malformation (SCM) A. SCM type I—two hemicords in separate dural sleeves and separated by osseous septum that has to be removed to untether the cord B. SCM type II—single dural sac with a fibrous band splitting the tethered cord XII. KLIPPEL-FEIL SYNDROME—congenital fusion of at least two cervical vertebrae; associated with multiple systemic anomalies (one kidney, cardiac irregularities, etc.). A. Evaluation—electrocardiogram (ECG), chest x-ray (CXR), and renal ultrasound B. Treatment 1. Fuse from an anterior and posterior approach if unstable after trauma XIII. CRANIOSYNOSTOSIS A. Fontanelles—anterior closes at 18 months; posterior closes at 3 months B. Skull diploë—forms at 4 years in unilaminar bone C. Evaluation 1. Palpate the prominent suture 2. X-ray may fail to demonstrate a normal lucent suture. 3. 3-D computed tomography (CT) reconstruction demonstrates the abnormal shape. D. Sagittal synostosis—most common variety; more often seen in males 1. Signs/Symptoms—dolichocephalic or scaphocephalic shape with decreased biparietal distance 2. Treatment a. Prone position with a strip craniectomy from coronal suture to lambdoid suture 3 cm wide at 3 to 6 months b. Skull remodeling—required after 1 year to make the skull shorter and wider c. Be careful about blood loss and hypothermia E. Coronal synostosis—more common in females 1. Unilateral—plagiocephaly a. Normal side bulges; abnormal side has a harlequin eye due to elevated supraorbital margin (Fig. 11.6) 2. Bilateral—brachycephaly with proptosis and maxillary hypoplasia 3. Crouzon syndrome—bilateral synostosis with midface hypoplasia of sphenoid, orbital, and facial bones Fig. 11.6 Unilateral coronal synostosis (plagiocephaly). Computed tomography reconstruction with harlequin eye on the left. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 17, Fig. 17.) 4. Apert disease—as with Crouzon syndrome syndactyly, HCP, low IQ 5. Treatment—strip craniectomy or frontal craniotomy with lateral canthal advancement at 3 to 6 months with absorbable plates F. Metopic synostosis—trigonocephaly G. Lambdoid synostosis—more common in males and on the right side 1. Evaluation—rule out positional plagiocephaly due to the child lying on one side too much 2. Treatment—molding helmet (if positional) or strip craniectomy at 6 to 18 months XIV. SHUNT INFECTION—50% occur by 2 weeks. A. Causes—most common organisms are Staphylococcus epidermidis and S. aureus and gram-negative rods B. Signs/Symptoms—fever, leukocytosis, and headache C. Treatment—externalization of shunt, vancomycin (until cultures back), and shunt replacement after 10 days of antibiotics when cerebrospinal fluid (CSF) is sterile Helpful Hints
11: CONGENITAL AND PEDIATRIC LESIONS
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree