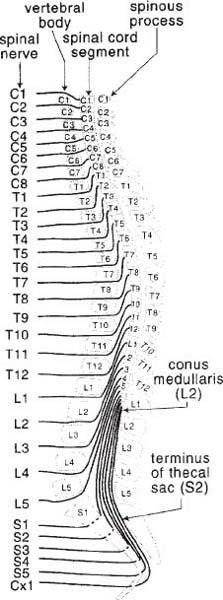
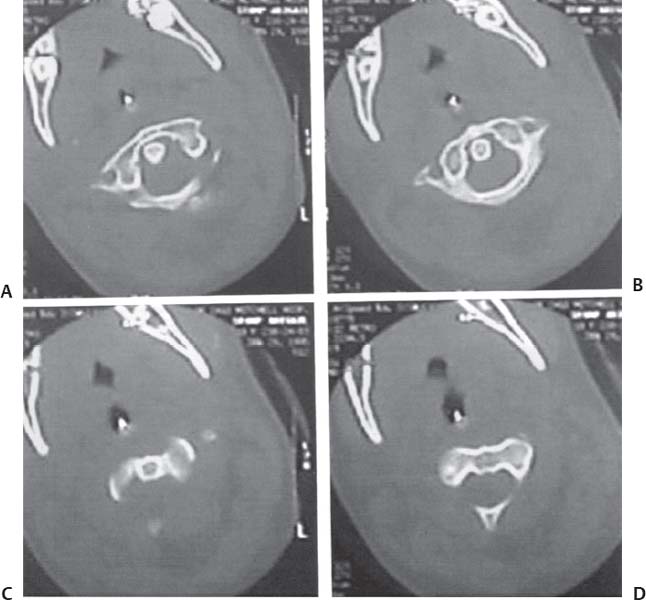
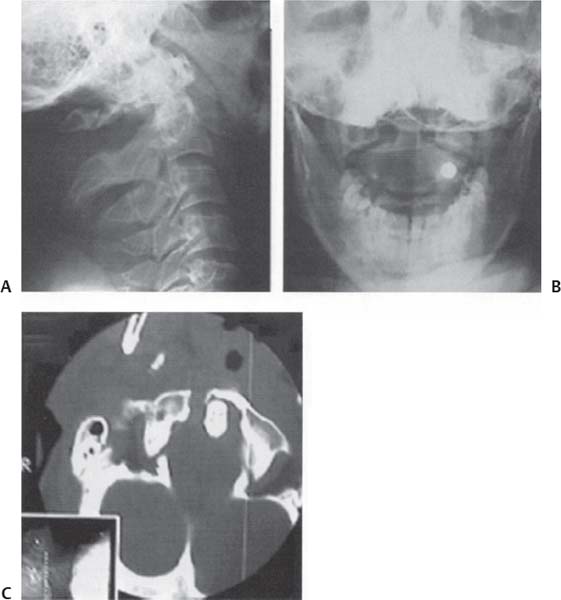
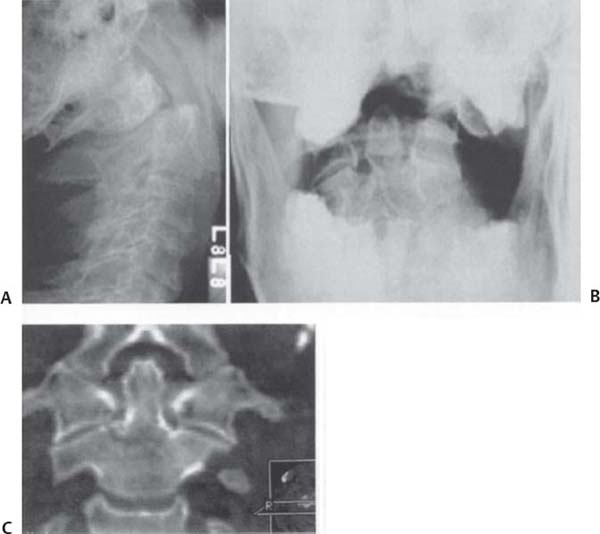
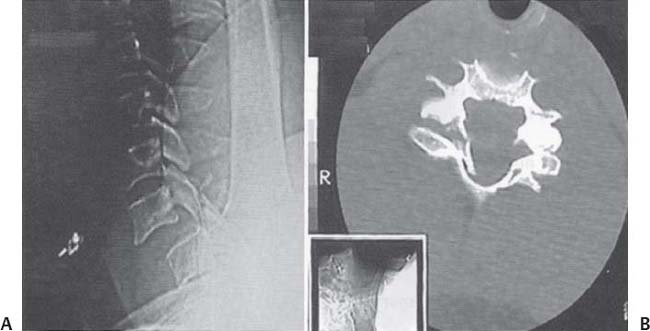
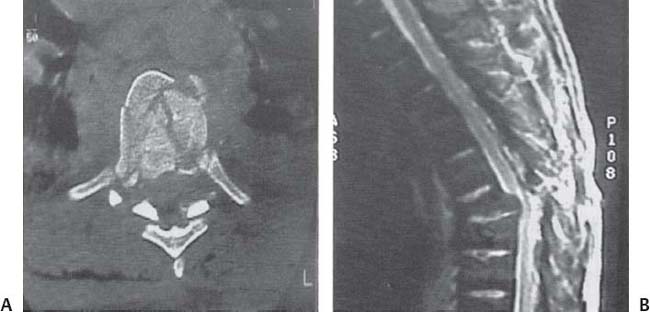
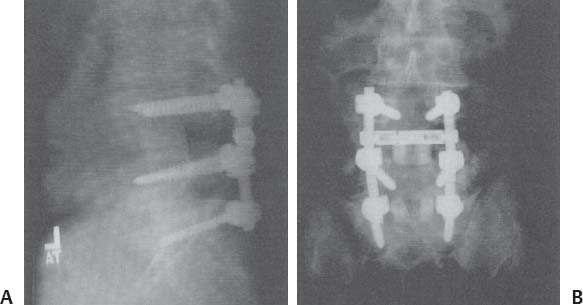
C H A P T E R 2 SPINE TRAUMA A. Loss of sympathetic tone and muscle paralysis cause venous pooling with hypotension (usually occur with injuries above T7) B. Loss of voluntary and reflex movements as well as sensation after a spinal cord injury; may last as long as 2 weeks; priapism is a bad sign II. HYPOTENSION A. Causes—hypovolemia, myocardial dysfunction, or loss of sympathetic tone B. Treatment 1. Loss of sympathetic tone—Levophed (norepinephrine), phenylephrine (may cause reflex bradycardia), or dopamine to maintain systolic blood pressure (SBP) > 90 mm Hg 2. Prevent pulmonary edema from overhydration 3. Use atropine for bradycardia III. INITIAL MANAGEMENT A. Immobilize with cervical collar and backboard B. Address ABCs (airway, breathing, circulation); consider nasotracheal intubation if no suspected cribriform plate trauma C. Insert nasogastric (NG) tube (ileus common), Foley catheter, and A-line D. Initiate deep vein thrombosis (DVT) prophylaxis with TED (thromboembolic deterrent) hose, sequential compression devices (SCDs), and subcutaneous (SQ) heparin or Lovenox E. Watch for hypothermia and electrolyte abnormalities IV. RADIOLOGIC EVALUATION A. Cervical, thoracic, and lumbar spine x-rays; chest x-ray (CXR); KUB (kidney, ureter, bladder); and pelvic x-ray B. No need to perform flexion–extension x-ray if > 3.5 mm subluxation because there is almost certainly instability C. Children < 4 years may have pseudospread of the atlas on anteroposterior (AP) view of 2–8 mm (a fracture must be determined by computed tomography [CT]). D. Children may also have 3 mm of subluxation at C2–3 up to 10 years V. SOLU-MEDROL (METHYLPREDNISOLONE) PROTOCOL A. Traumatic spinal cord dysfunction—medication must be started within 8 hours of injury B. Dose—30 mg/kg over 45 minutes, wait 15 minutes, then 5.4 mg/kg/h over 23 hours C. Third NASCAS study suggests that if steroids are started within 3 hours of injury, they should be continued for 24 hours; if started from 3–8 hours after injury, they should be continued for 48 hours. D. Controversial protocol, so know risks (acute corticosteroid myopathy, pneumonia, hyperglycemia, sepsis) and exclusion criteria (cauda equina syndrome, gunshot wounds, pregnancy, age < 13 years) if using it E. Steroid side effects—avascular necrosis, mood changes, hypertension, glucose intolerance A. Avoid in cases of atlantooccipital dislocation, type 2 or 3 hangman fractures, or children < 3 years B. Consider magnetic resonance imaging (MRI) before initiating traction to make sure there is not a herniated disk that may be pulled into the spinal cord (rare occurrence) C. Place Gardner-Wells tongs with pins 2.5 fingerbreadths above the pinna; for neutral position above the external acoustic meatus (EAM), for flexion 2 cm posterior, and for extension 2 cm anterior. 1. Tighten pins daily for 3 days to 60 lbs (pin indicator 1 cm beyond surface) 2. Avoid using traction weight > 40–50 lbs 3. Obtain frequent x-rays to evaluate alignment and make sure that the disk spaces do not exceed 10 mm and the occipital condyle–C1 lateral mass spaces do not exceed 5 mm 4. Halo pins should be placed while the eyes are closed to 8 lb/inch and the bars tightened to 30 lb/inch. 5. Dislocation reduction is best performed with fluoroscopy to save time. 6. Avoid raising the head preventing the patient from seeing the ground, but avoid overflexion preventing the patient from swallowing 7. Use pin care with half-strength hydrogen peroxide and bacitracin ointment three times daily (t.i.d) VII. SPINAL CORD LEVELS—to determine the location of a spinal cord level in relation to the vertebral level, subtract 2 from T2–10 to be at the spinal cord level A. Bones of T11–L1 are over the spinal cord levels L1–5, S1–5, and Cx1 (Fig. 2.1). Fig. 2.1 Spinal cord levels. (With permission from Greenberg MS. Handbook of Neurosurgery. 7th ed. New York, NY: Thieme Medical Publishers; 2010:944, Fig. 28–1.) VIII. COMPLETE INJURY A. No voluntary movement, sensation, or sphincter control below injured spinal cord level B. Priapism may occur from lack of sympathetic input. C. Watch for hypotension and bradycardia D. Autonomic dysreflexia may occur with an injury above T6; includes an exaggerated sympathetic response with hypertension, sweating, and flushing 1. May be stimulated by bowel or bladder emptying 2. Treatment—head of bed (HOB) elevation, Nipride or phentolamine, Valium, and maintaining an empty bladder and bowel A. Central cord syndrome—the most frequent incomplete injury 1. Cause—hyperextension, usually with preexisting cervical stenosis 2. Signs/Symptoms—weakness (more in the upper extremity [UE] than the lower extremity [LE] because the UE fibers are medial in the corticospinal and spinothalamic tracts), and various sensory and sphincter dysfunction 3. Treatment a. No evidence that early surgery improves outcome b. Decompression performed 1–3 weeks after injury to prevent recurrence and instability B. Anterior cord syndrome 1. Cause—anterior spinal artery cardiovascular accident (CVA) causing decreased motor function and loss of pain and temperature sensation, with sparing of proprioception a. Frequently associated with aortic dissection 2. Prognosis—poor C. Brown-Séquard’s syndrome—hemicord injury with ipsilateral motor and light touch/proprioception deficit with contralateral pain/temperature deficit 1. Cause—usually a penetrating injury 2. Prognosis if the deficit is partial—relatively good D. Posterior cord injury—causes only paresthesias and rarely occurs X. SCIWORA (SPINAL CORD INJURY WITHOUT RADIOGRAPHIC ABNORMALITY) SYNDROME A. Cause—usually occurs in children due to ligamentous flexibility B. Evaluation—inpatient with MRI and flexion–extension x-rays C. Treatment—collar should be worn for 3 weeks and sports avoided for 3 months XI. CERVICAL FRACTURE STABILITY A. Classical classification scheme—by White and Punjabi B. Nondisplaced fracture—assess stability with flexion–extension x-rays 1. Unstable—place in collar (or other orthosis) for 6–12 weeks and assess fusion at that point with another flexion–extension x-ray (various injury types are discussed later) 2. No instability on the dynamic x-ray—no collar needed; however, study may be insufficient because cervical muscle spasm may prevent adequate motion to demonstrate instability 3. Study questionable—keep patient in collar and repeat study in 2 weeks 4. Ligamentous instability—present if > 3.5 mm of subluxation or > 11 degrees of angulation a. These injuries usually require surgical stabilization because only 10–15% heal with immobilization. XII. ATLANTOOCCIPITAL DISLOCATION A. Joint stabilized mainly by tectorial membrane (posterior longitudinal ligament from C2 to occiput) and alar ligaments (from dens to C1 and occiput) (Fig. 2.1) B. Distance from occipital condyle to superior facet of atlas should be < 5 mm. C. Distance from basion to tip of dens should be < 5 mm in adults and < 10 mm in children. D. Power’s ratio—(anterior basion to posterior arch of C1)/(opisthion to anterior arch) > 1—suggests anterior dislocation (most frequent injury) E. Type 1 injury is anterior subluxation, type 2 is distraction, type 3 is posterior subluxation (very rare) Fig. 2.2 Atlantooccipital and atlantoaxial dislocations. Lateral cervical spine x-ray film demonstrates increased distance from the occiput to the atlas and the atlas to the axis. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 211, Fig. 295.) F. Treatment 1. Place patient in a halo immediately 2. Stabilize with occiput—C3 fusion 3. Lateral mass plates with occipital extension may also be used. 4. If a condylar fracture presses on brainstem, the patient should be placed in a halo and treated with transoral decompression followed by posterior fusion. 5. Evaluate for associated vertebral artery dissection with magnetic resonance angiography (MRA); if present treat with heparin/Coumadin for 3 months (Fig. 2.2) XIII. ATLANTOAXIAL DISLOCATION A. Anterior dislocation 1. Cause—transverse ligament injury or dens fracture 2. Treatment a. C1–2 fusion using sublaminar wires (i.e., Brook’s, Gallie, or Sonntag) or transarticular screws (see Chapter 1) b. Brooks technique—sublaminar wires under both C1 and 2 with two cubes of bone between the laminas c. Gallie technique—H-shaped bone graft over C1 and 2 held by a wire sublaminar at C1 and around the spinous process of C2 d. Dickman and Sonntag technique—similar to Gallie technique with the wire sublaminar under C1 only, but the bone graft is U-shaped and lodged between the laminas of C1 and 2 as well as around the spinous process of C2 e. Songer titanium cables should be tightened to 30 lb/inch (Fig. 2.3). Fig. 2.3 Lateral cervical spine X-ray of Brooks fusion. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 128, Fig. 12.4.) 1. Signs/Symptoms—head tilt, flexion, and rotation 2. Evaluation—CT 3. Treatment—attempt reduction with 7–15 lbs of traction a. If reduced—immobilize for 6 weeks and reassess with dynamic studies b. Fuse early at C1–2 if there is anterior subluxation or the transverse atlantal ligament is disrupted (Fig. 2.4A–D) Fig. 2.4 Atlantoaxial rotatory subluxation. (A–D) Axial computed tomography demonstrates the 45-degree rotation of the atlas on the axis. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 212, Fig. 297.) A. Jefferson’s fracture—4-, 3-, or 2-point fractures from axial loading B. Usually unstable C. Evaluation—evaluate with open-mouth-view x-ray and CT 1. According to the rule of Spence, > 7 mm of C1–2 combined overhang on open-mouth x-ray suggests disruption of the transverse atlantal ligament 2. Ligament can usually be visualized on axial MRI and a disruption determined. D. Treatment 1. Fracture of the tubercle connecting the transverse ligament usually heals well with immobilization. 2. If ligament intact—halo or SOMI (sternal occipital mandibular immobilizer) brace 3. If ligament disrupted—perform occiput–C3 posterior fusion or possibly a C1–2 posterior fusion if arch is stable (Fig. 2.5A–C) E. C1 and C2 fractures 1. Treatment—according to C2 injury a. Hangman fracture—halo b. Type 2 dens fracture with < 6 mm displacement—halo and > 6 mm displacement (occiput–C2 fusion or C1–2 transarticular screws) c. Type 3 dens fracture—halo XV. C2 FRACTURE A. Hangman fracture—pars fracture (spondylolisthesis) between the superior facet process (anterior, in line with the occiput–C1 joint) and inferior facet process (posterior, in line with the other cervical facet joints) 1. Cause—Usually from hyperextension and axial loading (not distraction as with judicial hangings of the past) Fig. 2.5 Jefferson’s fracture. (A) Lateral and (B) open-mouth x-ray films. (C) Axial computed tomography demonstrates anterior and posterior arch fractures with prominent right-sided overhang seen in (B). (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 211, Fig. 296.) 2. Usually stable and rarely presents with a deficit (Fig. 2.6) 3. Effendi classification (by C2–3 subluxation at the posterior longitudinal ligament [PLL] line) Type 1—< 3 mm of C2–3 subluxation; treat with SOMI brace for 3 months Type 2—> 4 mm subluxation or > 11 degrees angulation; reduce with traction then place in a halo or Minerva brace (surgery only if unable to maintain reduction) Type 3—C2–3 locked facets with 50% subluxation; treat with an anterior C2–3 fusion or a posterior C1–3 fusion (or C1–2 fusion) Fig. 2.6 Hangman fracture. Lateral cervical spine x-ray film demonstrates the C2 traumatic spondylolisthesis with anterior angulation. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 213, Fig. 300.) B. Dens fracture—C1–2 joint provides 50% of the motion of the cervical spine. 1. Steele’s rule of thirds—at the level of the dens, the spinal canal is filled by thirds of spinal cord, cerebrospinal fluid (CSF), and dens. 2. Anderson and D’Alonzo classification a. Type 1—oblique fracture through the tip of the dens (rare); treat with halo b. Type 2—fracture at base of dens; treat with halo 3 months if < 6 mm displacement or if < 7 years i. Perform fusion if unable to maintain reduction in a halo ii. 30% nonunion rate in a halo, but only 10% if < 6 mm displacement iii. Treatment—Surgical options include anterior odontoid screw (maintains range of motion, requires intact transverse ligament, avoid if fracture > 2 weeks old or if patient has barrel chest), posterior transarticular C1–2 screw (need a CT to determine if screws can be placed without vertebral artery injury), or posterior sublaminar wire fusion (Brook’s, Gallie, or Sonntag as above) (Fig. 2.7A–C) Fig. 2.7 Odontoid fracture (type 2). (A) Lateral and (B) open-mouth cervical spine x-ray films demonstrate the fracture through the base of the dens with posterior dislocation. (C) Coronal tomography of type 3 dens fracture. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 212, Fig. 298.) c. Type 3—fracture through body of axis; stable; treat with a SOMI brace XVI. CLAY SHOVELER FRACTURE—Involves Spinous Process of C7, C6, or T1 A. Stable if no associated ligamentous injury B. No collar needed A. Cause—major flexion injury B. Produces wedge-shaped fracture on anteroinferior aspect of vertebral body C. Usually severe ligamentous injury and instability D. Should be differentiated from a stable compression fracture E. Treatment—anterior and posterior fusion (with lateral mass plates or interspinous wiring), though a single approach may be sufficient XVIII. LOCKED FACETS—May Be Unilateral or Bilateral (with > 50% Subluxation) A. Treatment 1. Reduction with traction starting at 3 lb/level and increasing the weight by 5 lbs every 10 minutes while obtaining X-rays to determine alignment and rule out distraction injury (stop if occipitoatlantal dislocation > 5 mm or disk space > 10 mm) 2. Avoid > 5 lbs per level 3. Muscle relaxants—may help achieve reduction, but keep patient alert and examinable 4. MRI prior to traction to rule out disk herniation 5. Once patient is reduced, lower the weight to 10 lbs 6. Bilateral facet injury—all patients should be stabilized surgically. 7. Unilateral facet dislocation—many patients will heal in a brace, but surgery should be performed in the presence of radiculopathy or failure to maintain reduction. 8. Stabilization can be performed anteriorly (with a plate), but the posterior approach (with lateral mass screws and interspinous wires) is preferred. Fig. 2.8 Bilateral interfacetal dislocation. (A) Lateral cervical X-ray film and (B) axial computed tomography demonstrates the C6–7 injury with bilateral jumped facets. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 214, Fig. 302.) a. Lateral mass screws inserted into middle of lateral mass and angled 10–30 degrees laterally and rostrally per x-ray and 14–20 mm deep per x-ray to be bicortical with 3.5 mm screws b. Remember to prepare patient for iliac bone graft if not using allograft c. After stabilization, patient is placed in a brace for 6–12 weeks. 9. There is often vertebral artery occlusion with facet dislocation (Fig. 2.8A,B). XIX. FLEXION LIGAMENTOUS INJURY WITH POSTERIOR INSTABILITY A. Reduce and fuse posteriorly with sublaminar or interspinous wires or lateral mass plates (Fig. 2.9) XX. EXTENSION LIGAMENTOUS INJURY OR ANTERIOR COMPRESSION FRACTURE A. Fix anteriorly with cervical diskectomy, fusion, and plating. Fig. 2.9 Flexion dislocation. Sagittal T2-weighted magnetic resonance imaging demonstrates the C4–5 subluxation and angulation. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 214, Fig. 303.) XXI. CERVICAL ORTHOTICS A. Philadelphia collar—most effective for decreasing motion in the lower cervical spine (C5–T1) B. SOMI brace—most effective for reducing flexion in the upper cervical spine C. Minerva brace—most effective for midcervical instability D. Halo vest—most effective for instability at C1–2 or C5–T1 XXII. THORACOLUMBAR FRACTURES A. Denis three-column model 1. Anterior column—anterior longitudinal ligament (ALL) and ½ disk 2. Middle column—PLL and ½ disk 3. Posterior column—facets, laminas, spinous processes, and associated ligaments B. Two-column injury considered unstable C. Compression fracture 1. Only anterior column is injured. 2. Considered unstable if vertebral height is decreased > 50% or there is > 30 degrees angulation 3. Treatment—brace (TLSO) or surgical stabilization (anterior or posterior approach) D. Burst fracture 1. Both the anterior and middle columns are injured. 2. Considered unstable if vertebral height is decreased < 50%, the angulation is > 20 degrees, or there is > 50% canal compromise 3. Treatment—TLSO brace (3–6 months) or surgical decompression and stabilization (anterior approach is preferred over a posterior approach) 4. L5 burst fracture is difficult to instrument anteriorly; consider L4–S1 posterior fusion and TLSO brace with thigh cuff in 10 degrees flexion (Fig. 2.10A,B) Fig. 2.10 Burst fracture. (A) Axial computed tomography and (B) sagittal T2-weighted magnetic resonance imaging scans demonstrate angulation with retropulsion at T9. (With permission from Citow JS. Neuropathology and Neuroradiology: A Review. New York, NY: Thieme Medical Publishers; 2001: 215 Fig. 305.) 1. Both the middle and posterior columns are injured. 2. Evaluation—sagittal CT reconstructions 3. Treatment—posterior instrumented fusion 4. Chance fracture—through vertebral bodies F. Fracture-dislocation—three-column injury requiring anterior and posterior stabilization G. Instrumentation 1. Pedicle screws may be placed from C7 through the sacrum 2. Exposure—must extend to tip of transverse processes to allow decortication of transverse processes and lateral facets 3. Entrance site—junction of medial transverse process and superior articulating process 4. Awl is used to open into the pedicle 5. Fluoroscopy is used to place screws (5.5 or 6.5 mm) parallel to end plates and ending 80% into vertebral body 6. Intraoperative monitoring is used to stimulate screws to make sure there is no violation of cortex with pressure on a nerve root. 7. Rod–hook systems may also be used in the thoracic and lumbar spines with pedicle hooks (up only), transverse process hooks (down only), or laminar hooks (up or down). 8. Rod–hook systems may be connected to pedicle screws. 9. Instrumentation should extend three levels above and two levels below the injury. 10. Construct may need to be extended to avoid ending at a transition level (cervicothoracic, thoracolumbar, or lumbosacral) or at a thoracic kyphosis 11. Space lateral to facets should be packed with morselized bone 12. Anterior instrumentation with plates or rods involves bicortical screws (Fig. 2.11A,B). Fig. 2.11 (A) Lateral x-ray of L4-S1 pedicle screw fusion with Tangent bony posterior lumbar interbody fusion (PLIF). (B) Anteroposterior x-ray of L4-S1 pedicle screw fusion with Tangent bony PLIF. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 138, Fig. 12.12.) H. Pathological fractures 1. If mechanism not severe enough to explain the bony destruction, consider a tumor, infection, or osteoporosis 2. Evaluation—MRI, inflammatory markers (ESR, CRP, WBC, cultures), bone scan, and CXR XXIII. OSTEOPOROSIS A. Evaluation—bone mineral density and DXA (dual-energy x-ray absorptiometry) scan of proximal femur and lumbosacral spine 1. Rule out hyperthyroidism, increased parathyroid hormone (PTH), steroids, and tumor B. Treatment 1. Exercise 2. Calcium 3. Estrogen a. Increases DVT risk, possibly increases breast cancer risk, and decreases coronary artery disease b. Add progesterone to decrease endometrial carcinoma risk 5. Calcitonin 6. Fosamax—decreases bone resorption C. Compression fractures 1. Treatment a. Bracing, kyphoplasty, or vertebroplasty—methylmethacrylate injected to decrease pain; also used for pathological fractures and hemangiomas b. Surgery—rarely needed XXIV. GUNSHOT WOUNDS A. Treatment 1. Surgery—useful only for incomplete spinal cord injury, CSF leak, instability (rare), or copper bullets 2. Colon perforation with CSF leak—explore to clean and pack the defect (80% infection rate) 3. Gastric and small bowel injuries are less contaminated. a. Use antibiotics but not steroids 4. Lead from the bullet may rarely cause lead poisoning with neuropathy, encephalopathy, anemia, abdominal pain, and renal dysfunction. Helpful Hints
2: SPINE TRAUMA
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree