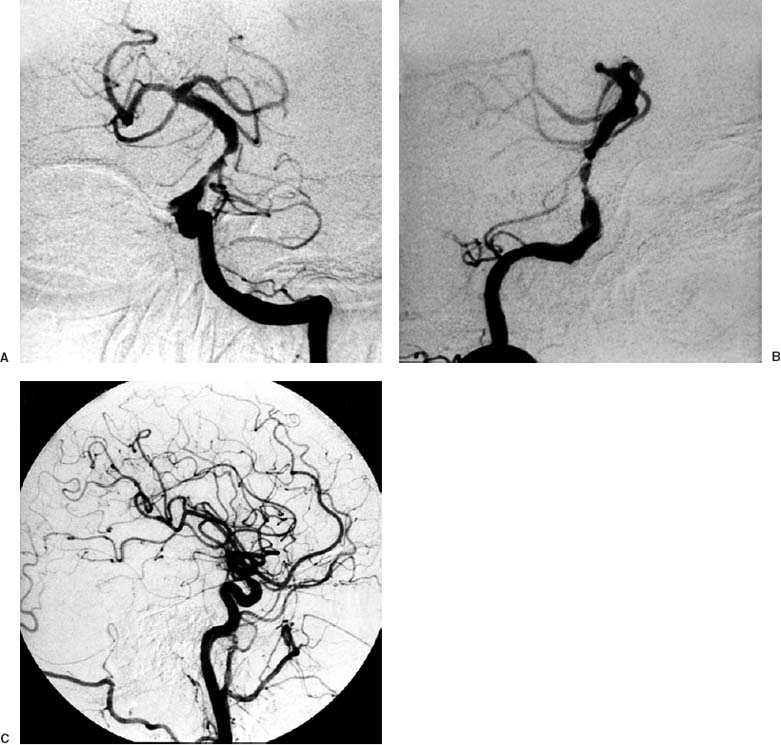
23 Diagnosis Vertebrobasilar Transcent ischemic attacks (TIAs) due to a basilar artery stenosis Problems and Tactics An atherosclerotic stenosis at the midportion of the basilar artery induced frequent vertebrobasilar TIAs despite optimally regulated anticoagulant therapy. Posterior fossa revascularization by the use of microsurgical occipital artery–superior cerebellar artery (OA–SCA) bypass was selected as a therapeutic modality. Keywords Basilar artery stenosis, vertebrobasilar TIA, OA–SCA bypass, sitting position A 72-year-old female suffered from frequent vertebrobasilar TIAs manifested with lacrimation, dysarthria, vertigo, and right sensorimotor brachiofacial hemiparesis despite optimally regulated oral anticoagulation therapy. The patient presented additionally with a diabetes mellitus and paroxysmal atrial fibrillation. Angiography revealed a severe basilar stenosis (supposed to be due to dissection) from the site of vertebral union to the origin of the anterior inferior cerebellar artery (Fig. 23–1A, B). Both of the posterior communicating arteries were not visualized on the carotid angiography. Magnetic resonance imaging (MRI) revealed no ischemic lesions, but the [H2–15O] water positron emission tomographic (PET) study revealed reduced cerebral blood flow with decreased hemodynamic reserves on Diamox® loading. For the augmentation of the posterior fossa circulation, a microsurgical OA–SCA bypass was performed. In the sitting position, the head was fixed with a MayfieldKees apparatus with the face turned to ~20 to 30 degrees to the operating side and the neck flexed to ~20 to 30 degrees. 1. The occipital artery was traced and marked percutaneously with Doppler sonography with reference to the selective external carotid angiography (Fig. 23–1C). This artery is usually detectable at the midportion between the external occipital protuberance and the mastoid process at the level of the superior nuchal line, where the great occipital nerve accompanies the artery. Above the superior nuchal line after having run for ~2 to 3 cm, it terminates into medial and lateral branches. A bigger branch (~1 mm in diameter) should be taken as the bypass graft. FIGURE 23–1 Left vertebral angiography reveals a severe stenosis of the basilar artery. (A) Anteroposterior view. (B) Lateral view. (C) Common carotid angiography showing the running course of the occipital artery, which should be compared with the follow-up angiography. 2. Dissection of the occipital artery followed after a linear incision over the artery. It is advisable to begin with the dissection at the level of the superior nuchal line, in which the crossing great occpital nerve should be cut sharply to dissect the OA. The dissection was then forwarded to the parietal region, taking care of the terminal peripheral branch that runs into the subcutaneous tissue and not subcutaneously. Below the superior nuchal line the OA takes a serpentine course into the depth between muscle layers to the direction of the inner side of the mastoid process. 3. Big Gelpi retractors were used to spread the skin and muscles, this being usually sufficient for hemostasis from the wound surface. The OA was dissected in this way in a length of 10 to 15 cm and was cut at the end after putting a temporary clip. The distal lumen was then irrigated with heparinized saline (1000 IU/100 mL saline) and was put aside at the caudolateral corner of the operating field. After incising the muscle and periosteum, the occpital squama was exposed (Fig. 23–2A).
Occipital Artery–Superior Cerebellar Artery Bypass (Paramedian Supracerebellar Approach) for Vertebrobasilar TIAs Due to a Severe Basilar Artery Stenosis
Clinical Presentation
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree