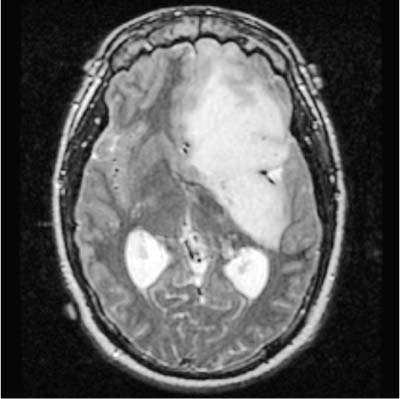
28 Diagnosis Dominant hemisphere insular tumor Problems and Tactics This is a patient with seizure disorder who presented with a large left insular glial tumor. He was operated on using language mapping techniques, neuronavigation, and microdissection. Intraoperative stimulation mapping of subcortical pathways and the use of language mapping techniques are essential during resection of insular tumors to minimize surgical morbidity, especially in infiltrating tumors at this location.1,2 Keywords Insula, dominant hemisphere, tumor, language mapping This patient was an 18-year-old man whose initial complaint was new-onset seizures, with 3 prior. A month later, a left insular World Health Organization Grade III glioma was diagnosed by biopsy. Since then he continued to experience seizures, some of which were generalized. He did not have any additional symptoms. Family history, apart from a cousin with a brain tumor who died at 16 years of age, was not significant. His was neurologically intact except for occasional paraphasic errors. A magnetic resonance imaging (MRI) scan confirmed a large nonenhancing mass in the left frontotemporal area (Fig. 28–1). The patient was taken to the operating room and placed in supine position with a roll under the left shoulder, with limbs partially flexed and all pressure points padded. His head was turned to the right and fixed in the Mayfield tongs. The scalp fiducials were registered with the Stealth station (TM) (Medtronic Surgical Navigation Technologies, Minneapolis, MN) navigation system. The scalp was then scrubbed, prepped, and draped in a sterile fashion. The patient’s previous incision behind the hairline was reopened and then extended posteriorly. The scalp flaps were hooked into place, and then the bone flap was removed. Another temporal bone flap, including a small piece in the frontal area, was removed to obtain adequate exposure. After the dura was opened, cortical stimulation mapping was performed and the location that caused speech in speech arrest at 4 mA and was designated as 10 (Fig. 28–2). There were no sites at 5 or 6 mA for naming or reading, and we did not find any areas that when stimulated resulted in motor movements. The overlying cortex was coagulated up to Broca’s area and over the superior and middle temporal gyri. We began the dissection in the frontal area and entered a very large and slightly vascular lesion, which was easily resected with the Cavitron Ultrasonic Surgical Aspiration System (CUSA). The resection continued down through the frontal lobe until we entered the ventricle, where a small piece of Gelfoam was placed. Further resection was done inferiorly toward the sylvian fissure and the insular branches were preserved. At this point resection through the temporal lobe was performed down into the temporal horn, using the microscope so as not to injure any of the middle cerebral vessels underlying the resected superior temporal gyrus or the inferior insular surface. FIGURE 28–1 Axial T2-weighted magnetic resonance scan showing a large dominant insular tumor.
Dominant Hemisphere Insular Tumor
Clinical Presentation
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree