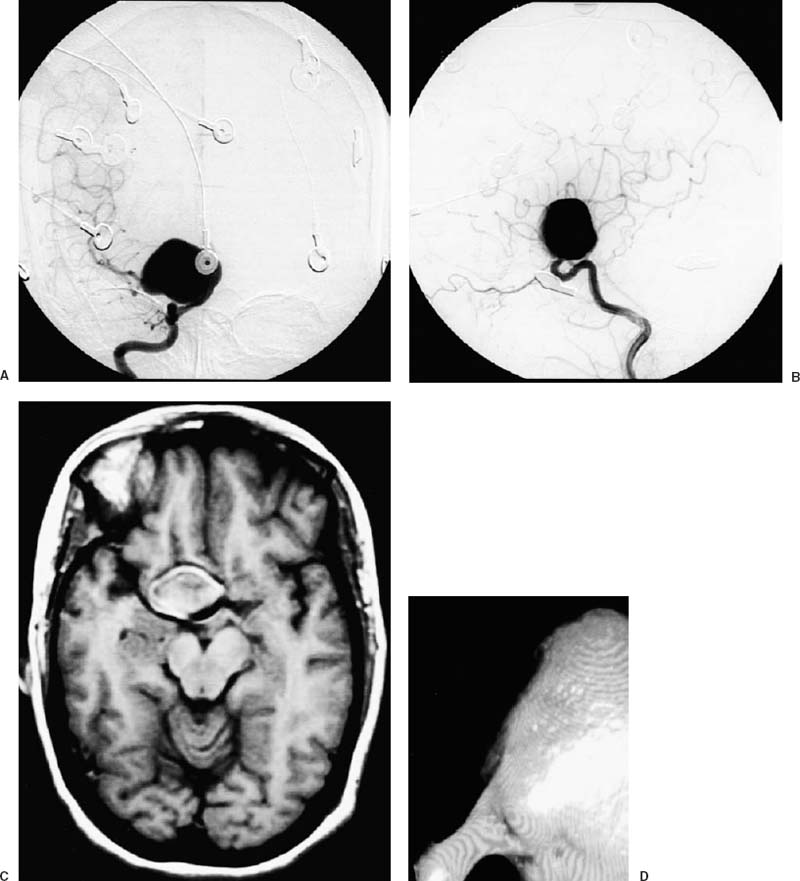
3 Diagnosis Giant paraclinoid carotid aneurysm Problems and Tactics An otherwise healthy middle-aged woman presented with a symptomatic giant paraclinoid carotid aneurysm. Because of the complex aneurysmal morphology and thick, broad-based neck, we utilized preoperative cerebrovascular reserve testing and ultimately prophylactic cerebral revascularization prior to microneurosurgical clip reconstruction. Angiographic exclusion of the aneurysm from the intracranial circulation was demonstrated intraoperatively; however, a postoperative angiogram, obtained shortly thereafter, showed recanalization of the aneurysmal sac through a tiny neck remnant, a finding that mandated reoperation. Because blood had traversed into the subarachnoid space through the surgically opened aneurysm following the initial attempt at thrombus decompression and arterial reconstruction, the patient developed cerebral vasospasm. The hyperdynamic therapy instituted to prevent clinically overt neurological ischemia resulted in two significant hemorrhagic complications, which required additional operative intervention. Despite both the formidable vascular lesion with which our patient initially presented as well as the significant problems encountered during her hospital course, she has recovered completely and returned to her preoperative functional status. Keywords Paraclinoid aneurysm, giant aneurysm, cerebral revascularization, intraoperative angiography, balloon test occlusion A 49-year-old Asian woman with no significant medical history other than mild, right-sided retroorbital pain was found at an outside hospital to possess an incidentally discovered and partially thrombosed giant aneurysm arising from the paraclinoid segment of her right carotid artery on computed tomographic (CT) scan. In addition to the giant aneurysm, her preoperative cerebral angiogram after right internal carotid artery injection (Fig. 3–1A,B) demonstrated the following important findings: isolated filling of the middle cerebral artery (MCA) secondary to a severely hypoplastic or absent A1 segment of the anterior cerebral artery (ACA); absence of a posterior communicating artery (PCoA); and a small, tortuous efferent carotid artery emerging from the aneurysm sac. The patient was transferred to Northwestern Memorial Hospital and admitted under the care of Dr. Batjer for definitive treatment of her complex cerebrovascular lesion. Upon admission, the patient continued to complain of right-sided retroorbital pain, but denied a history suggestive of prior subarachnoid hemorrhage. She was alert and oriented in all dimensions, and her neurological examination was normal. Formal ophthalmologic evaluation failed to reveal any visual field deficits. Both magnetic resonance imaging (Fig. 3–1C) and CT angiography (Fig. 3–1D) were performed to better delineate the anatomy of the aneurysm with respect to the cranial base, the extent of intraaneurysmal calcification and thrombosis, and the proximity of the lesion neighboring vasculature. In view of the wide-based neck and the need for intracranial decompression, clip reconstruction was considered the best therapeutic strategy. FIGURE 3–1 (A) Anteroposterior and (B) lateral cerebral angiograms following right internal carotid artery injection demonstrating the giant aneurysm arising from the paraclinoid segment. (C) Preoperative magnetic resonance imaging of the lesion. (D) Preoperative computed tomographic angiography of the lesion demonstrating the complexity of the aneurysmal neck. After general endotracheal anesthesia was induced and body cooling was initiated, the patient was placed in a supine position with her head rotated ~35 degrees contralaterally and stabilized in the Mayfield-Kees three-point fixation system. Following shaving both the right frontotemporal cranium and the anterolateral neck, these regions were then prepped and draped in the usual sterile fashion. After sharp tissue dissection through the anterolateral neck, the carotid sheath was widely opened, the common facial vein was doubly suture-ligated, and both the internal and external carotid arteries were clearly identified as they originated from the common carotid artery. A vessel loop was then placed under a completely exposed internal carotid artery to definitively establish cervical carotid control.
Surgical Management of a Challenging Giant Paraclinoid Aneurysm
Clinical Presentation
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree