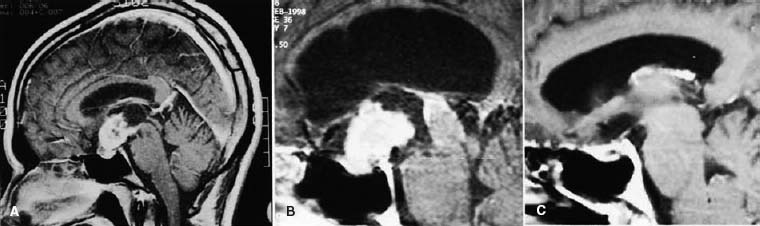
38 Diagnosis Craniopharyngioma Problems and Tactics Despite total removal under the microscope craniopharyngiomas often recur1,2 during long-term follow-up because: (1) attachment of the tumor to the stalk, hypothalamus, and undersurface of the optic chiasm are blinded, and microscopical tumor invasion into these vital structures makes complete removal difficult; (2) the surgeon’s aggressiveness for tumor removal from these structures should be cautiously weighed against postoperative functional deficits. In the present case, a 5-cm retrochiasmatic–third ventricular tumor was totally removed via a bifrontal basal interhemispheric approach. A second surgery was performed at 8 years and a third at 12 years, 4 months after a gamma knife surgery. The tumor was totally or grossly totally removed each time in spite of marked tissue adhesion. Part of the reason is that the patient’s short anterior communicating artery (ACoA) prevented sufficient brain retraction and tumor dissection especially under and lateral part of chiasm under direct vision. Keywords Craniopharyngioma, recurrence, gamma knife, interhemispheric approach This 38-year-old man had presented with loss of libido and mild visual disturbance for the previous 6 months. Magnetic resonance imaging (MRI) showed a 50-mm mixed solid and multicystic tumor in the retrochiasmatic region and third ventricle. Via a bifrontal basal inter-hemispheric approach the tumor was totally removed. The tumor recurred 6 years later and was subtotally (98%) removed 8 years after the first surgery. The tumor again grew during the following 4 years. Four months after gamma knife surgery, rapid tumor growth impinging on the optic apparatus forced a third operation and the tumor was totally removed. The patient returned to his normal daily life without hormonal replacement but with a moderate visual disturbance in the left eye. For a 50 × 26 × 25 mm mixed solid and multicystic tumor (Fig. 38–1) surgery was performed via a bifrontal basal interhemispheric approach.3 A bone flap was made through a coronal skin incision. The nasal portion of the frontal base was removed in one piece with the bone flap. The basal interhemispheric fissure was dissected down to the chiasmal region. Yellow cystic tumor was seen in the prechiasmatic cistern but only a small amount of clear fluid was evacuated. A dark-yellow cyst seen in the lamina terminalis was cut in the midline and cystic fluid was evacuated. Continuous cerebrospinal fluid (CSF) drainage using a thin plastic tube settled in the bottom of the operative field was helpful in keeping the operative field dry and clean and preventing postoperative chemical meningitis and subsequent tissue adhesion. Tumor content was removed by a two-suction technique.3 Serrated suction tips were especially useful in cutting and suctioning the tumor and retracting the cyst wall.4 The tumor boundary was not always clear. The part invading the wall of the third ventricle was bluntly dissected using bipolar forceps by both a pinching and spreading motion of the blades. The upper part of the cyst wall in the posterior third ventricle could be pulled down without difficulty. It is important to remove the tumor in large blocks, and not in tiny pieces, to keep the continuity of the tumor capsule. FIGURE 38–1 (A) Before operation. A 50-mm retrochiasmatic solid and cystic posterior third ventricular tumor that was totally removed. (B) Before second operation. Magnetic resonance imaging (MRI) 8 years later shows a 30-mm retrochiasmatic solid tumor and a separate 20-mm cystic tumor in the pineal region and hydrocephalus. (C) After second operation. Enhanced MRI after the second surgery shows no tumor. The tumor was dissected from the optic chiasm from both above and below using a tip-bent silver dissector. Tension on the optic nerves was reduced by opening the falciform process on both sides, which made visualization of the part of the undersurface of the chiasm possible. The pituitary stalk was seen running under the surface of the tumor on the right side, which could be dissected from the tumor. The ACoA was extremely short and crossing the midline as an X-shape, which limited lateral retraction of the brain (Fig. 38–2C). The lateral part of the under-surface of the chiasm could not be inspected completely even with the use of a small mirror. Here, where it attached most heavily, the tumor had to be dissected blindly; however, the tumor was considered to be totally removed.
Total Removal of a Recurrent Craniopharyngioma
Clinical Presentation
Surgical Technique
First surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree