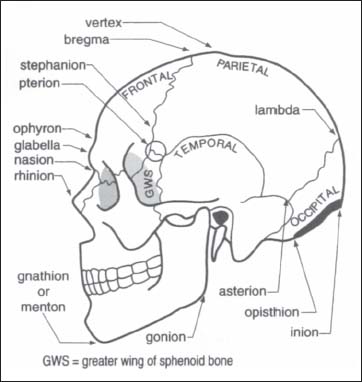
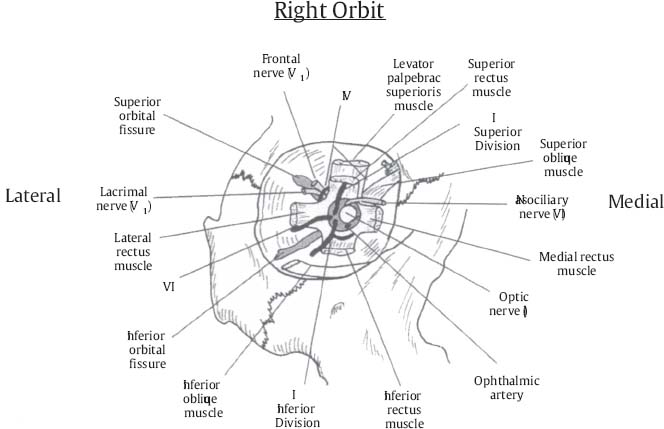
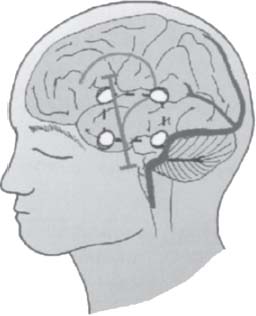
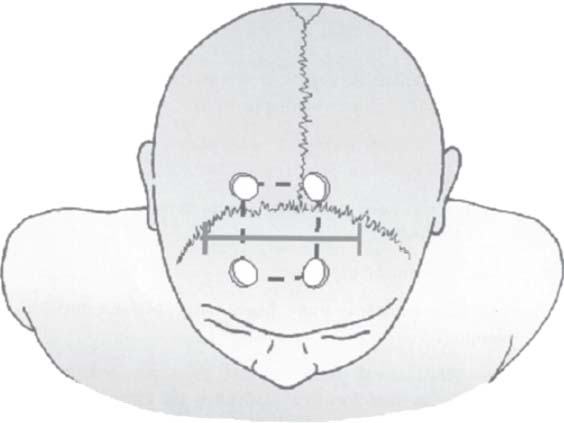
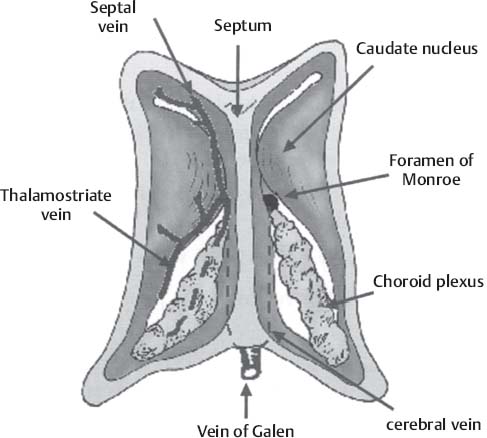
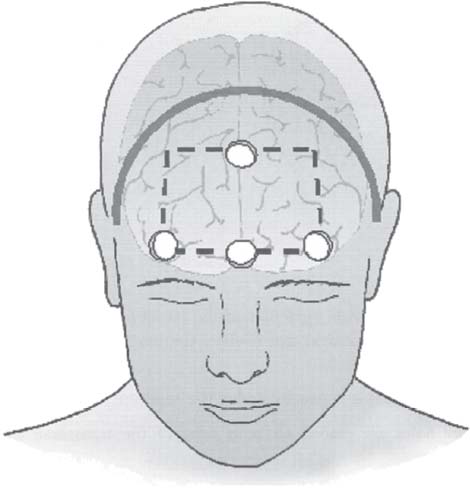
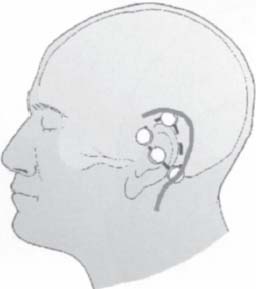
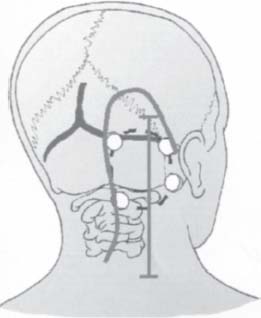
C H A P T E R 6 CRANIAL ANATOMY AND APPROACHES I. PTERION A. Junction of frontal, parietal, temporal, and greater wing of sphenoid bones B. Located two fingerbreadths above the zygomatic arch and two finger-widths behind the frontal process of zygoma (Fig. 6.1) II. ASTERION A. Junction of lambdoid, parietomastoid, and occipitomastoid sutures B. Located over the transverse–sigmoid junction Fig. 6.1 Craniometric points. (With permission from Greenberg MS. Handbook of Neurosurgery. 7th ed. New York, NY: Thieme Medical Publishers; 2010: 86, Fig. 5–4.) A. Junction of coronal–sagittal suture IV. FRANKFORT PLANE A. From inferior orbit to top of external acoustic meatus (EAM) V. POSTERIOR EAR LINE A. Midmastoid up rostrally perpendicular to baseline (Frankfort plane) VI. SYLVIAN FISSURE A. Lateral canthus to ¾ of nasion–inion line and ending at posterior ear line VII. MOTOR STRIP A. 4–5 cm behind coronal suture; top is at posterior ear line and direction is 45 degrees from Frankfort baseline VIII. CENTRAL SULCUS A. Top is 2 cm behind ½ nasion–inion line (3–4 cm behind coronal suture); bottom is 5 cm above EAM IX. ANGULAR GYRUS A. Located just above the pinna; caps the superior temporal sulcus B. The Wernicke receptive speech area also includes the supramarginal gyrus that caps the sylvian fissure. X. BROCA AREA A. Expressive speech center located in inferior frontal gyrus pars opercularis (behind the pars orbitalis and triangularis) XI. SUPERIOR ORBITAL FISSURE CONTENTS A. Cranial nerves (CNs) III, IV, V1 (all three branches: nasociliary, frontal, and lacrimal) B. Sympathetic fibers from the internal carotid artery (ICA) plexus C. Superior orbital vein D. Orbital branch of the middle meningeal artery E. Recurrent meningeal branch of the lacrimal artery XII. INFERIOR ORBITAL FISSURE A. CN V2 B. Zygomatic nerve C. Pterygopalatine branch of the maxillary nerve D. Infraorbital artery and vein E. Inferior ophthalmic vein XIII. ORBITAL TENDINOUS RING (ANNULUS OF ZINN) A. Structures passing above it include the lacrimal nerve, the frontal nerve, and CN IV. B. Structures passing through it include the superior and inferior divisions of CN III, the nasociliary nerve, and CN VI. C. Mnemonic—l uscious (lacrimal) F rench (frontal) t arts (trochlear) / s tand (superior division III) n aked (nasociliary) i n (inferior division III) a nticipation (abducens) (Fig. 6.2) XIV. CIRCLE OF WILLIS A. Complete in only 20% of the population XV. FETAL CIRCULATION A. ICA supplies the posterior circulation (occurs in 25% of the population) Fig. 6.2 Tendinous ring. (With permission from Citow JS. Comprehensive Neurosurgical Board Review. New York, NY: Thieme Medical Publishers; 2000: 76, Fig. 1–41) A. Enters the foramen transversarium at C6 B. Distal to the C1 foramina transversarium, it curves posteromedially toward the lamina of C1 and then pierces the dura to move anterosuperomedially toward the anterior brainstem. XVII. SURGICAL APPROACHES A. Temporal lobe lesions 1. Key Points a. Consider a lateral or supine patient position b. Skin incision may be horseshoe anterior and posterior to the ear, question mark extending posterior to the ear (gives widest exposure), or linear (for anterior lesions) (Fig. 6.3) c. Enter through the inferior or middle temporal gyrus and spare the superior temporal gyrus d. Safe to remove 5 cm of the dominant side and 7 cm of nondominant side (larger resection into optic radiation causes “pie in the sky” visual field cut) e. Be careful with the uncus (preserve medial arachnoidal plane near tentorium to avoid CN3 and PCA) and middle cerebral artery (MCA) branches in the sylvian fissure (stay in a subpial plane) B. Lateral ventricle atrium (trigone)—patient in lateral position; enter through the middle temporal gyrus, lateral temporoparietal cortex, or the superior parietooccipital region C. Frontal horn of lateral ventricle—patient in supine position; enter through the middle frontal gyrus D. Body of lateral ventricle—patient in supine position; transcallosal approach E. Third ventricle—patient in supine position; transcallosal approach (less seizure risk than with transcortical approach). 1. We prefer a linear incision to a horseshoe incision in this and most procedures. Fig. 6.3 Temporal Lobe exposure. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 78, Fig. 9.7.) 2. Be careful with superior sagittal sinus retraction, the surrounding veins, and the fornix. 3. Incise only 2.5 cm of the anterior corpus callosum. 4. Disconnection syndrome more likely with posterior incision through the splenium 5. Fenestrate the lateral ventricle and then proceed into the third ventricle via an interforniceal approach or extend the foramen of Monro posteriorly by opening the choroidal fissure, but avoid anteriorly through fornix (some say one fornix can be removed with little memory deficit). 6. Prepare both sides of the head in case interhemispheric veins are prohibitive for interhemispheric approach (craniotomy is positioned 1/3 behind coronal suture and 1/3 over midline; perform strip craniotomy over sinus separately (Figs. 6.4 and 6.5). F. Anterior fossa skull base—for olfactory groove meningiomas, etc. 1. Patient in supine position Fig. 6.4 Transcallosal exposure. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 80, Fig. 9.8.) Fig. 6.5 View inside the lateral ventricles. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 80, Fig. 9.9.) 2. Bicoronal incision is made connecting the two zygomatic arches (Soutor incision allows easier skin closure). 3. The scalp flap should be dissected forward above the pericranium to provide a vascularized flap for closure. 4. Dissection over the temporalis muscles should be in the interfascial plane or below the fascia when the fat pads are reached to avoid injuring the frontalis branch of the facial nerve. 5. Burr holes are placed at the keyholes and around the anterior superior sagittal sinus; bone flap is turned. 6. Anterior 1/3 of the sinus may usually be sacrificed when needed. 7. Frontal sinus should be cranialized by removing the posterior wall and removing the mucosa. 8. Frontal ostium should be plugged with muscle. 9. Blood supply is usually under the lesion; try to ligate as early as possible (preop embolization for meningiomas!). Fig. 6.6 Bicoronal craniotomy incision. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 81, Fig. 9.10.) 10. At closure, the pericranial flap should be placed over the base of the anterior fossa and sutured to the planum sphenoidale dura. 11. Outer dura should then be closed in a water-tight fashion. 12. Cerebrospinal fluid leak (CSF) should be treated with a lumbar drain and intermittent skull x-rays to watch for pneumocephalus. 13. Complications—injury to CNs I (almost always) and II, brain injury (cognitive impairment and seizures), anterior cerebral artery injury, and infection (Fig. 6.6). G. Transpetrosal approach—used to expose anterior or lateral lesions from the midbrain to the lower pons (i.e., cavernous malformation, clivus chordoma, and petroclival meningioma) (Fig. 6.7). 1. Patient positioned with falx parallel to floor (usually lateral). 2. Horseshoe incision is fashioned from the base of the mastoid, around the pinna, to the zygoma. Fig. 6.7 Transpetrosal craniotomy. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 82, Fig. 9.11.) 3. Zygoma, mastoid, and external auditory canal are identified. 4. Locate the asterion (junction of the parietomastoid, occipitomastoid, and lambdoid sutures) that overlies the junction of the transverse and sigmoid sinuses. 5. Transverse sinus is usually under the superior nuchal line. 6. Burr holes are placed on both sides of the transverse and sigmoid sinuses. 7. Do not dissect across the sinus with a Penfield #3; instead use a kerasin punch or eggshell the bone with a diamond drill. 8. Remove the boomerang-shaped bone flap 9. Drill off the mastoid bone to expose the semicircular canals and the superior petrosal sinus (in the dura at the junction of the tentorium, middle, and posterior fossa) 10. Maximize bony removal to minimize brain retraction 11. Open the presigmoid dura and divide the superior petrosal sinus 12. Locate the trochlear nerve under the tentorium 13. Operative window is between CNs V/VII and VII/IX. 14. The exposure will not reach lesions below the jugular foramen. 15. Close with a fat graft, fibrin glue, and a lumbar drain to prevent CSF leak (as high as 20%). H. Anterior foramen magnum lesions—consider transoral approach (see Rheumatoid Arthritis section), far lateral (transcondylar), or posterior approaches I. Far lateral (transcondylar) approach—for lesions involving the lower ⅓ of clivus to the upper cervical spine (contralateral vertebrobasilar junction aneurysm) 1. Patient positioned supine, head laterally flexed, vertex down, with ipsilateral mastoid as highest point. 2. Incision is made over the spinous processes of C1–C3 and curved laterally over the mastoid bone, or S-shaped incision 2 cm behind mastoid for small lesions. 3. Vertebral artery is identified at the superior C1 transverse arch as it pierces the dura to move up the foramen magnum. 4. Greater occipital nerve may be identified under sternocleiodomastoid muscle and followed down to the C2 nerve root. 5. C1 hemilaminectomy is performed and the foramen magnum is opened. 6. Lateral mass of C1 and posteromedial occipital condyle are drilled off to the hypoglossal canal (if more is removed, an occipitocervical fusion is needed). 7. Vertebral artery is mobilized from the C2 arch to the foramen magnum and retracted medially (Fig. 6.8). 8. Complications—injury to lower CNs (use intraoperative monitoring and consider preop trach and PEG). J. Perforate methylmethacrylate if used as a skull replacement to decrease the fluid accumulation under the bone flap. K. Intraoperative brain swelling—consider edema, blood clot, hydrocephalus, internal jugular vein occlusion, or hypercapnia Fig. 6.8 Far-lateral (transcondylar) incision. (With permission from Citow JS. Neurosurgery Oral Board Review. 1st ed. New York, NY: Thieme Medical Publishers; 2003: 83, Fig. 9.12.) 1. Evaluation—intraoperative ultrasound 2. Treatment—mannitol, Lasix, hyperventilation, and ventricular drainage a. Always consider placement of an occipital Frazier burr hole with posterior fossa surgery Helpful Hints
6: CRANIAL ANATOMY AND APPROACHES
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree