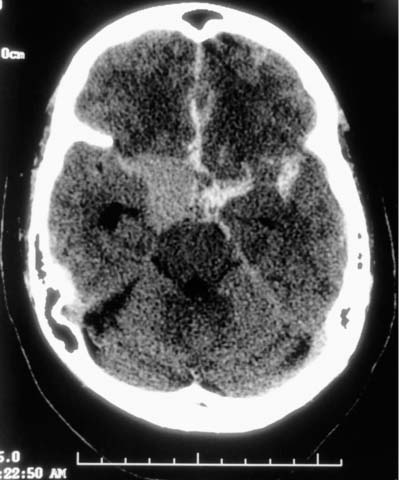
6 Diagnosis Giant ICA–SHA aneurysm Problems and Tactics This patient presented with a severe subarachnoid hemorrhage from a giant internal carotid artery (ICA) aneurysm arising at the origin of the superior hypophyseal artery (SHA).1 We believed surgical treatment would require prolonged temporary occlusion of the parent artery or parent vessel sacrifice if the aneurysm proved to be unclippable. The patient had inadequate collateral circulation to the ipsilateral hemisphere as determined by a balloon test occlusion. The surgical strategy we selected included the creation of a right external carotid artery (ECA) to middle cerebral artery (MCA) radial artery bypass graft to augment collateral circulation during anticipated prolonged temporary carotid occlusion or permanent occlusion of the carotid artery, if necessary. Keywords Superior hypophyseal artery aneurysm, giant aneurysm, extracranial–intracranial bypass graft, anterior clinoid process, dural rings, radial artery This 53-year-old woman experienced the sudden onset of severe headache and obtundation. She was transferred to Emory University Hospital in a Hunt and Hess Grade IV and underwent placement of a right frontal ventriculostomy with some improvement in her clinical condition (Fig. 6–1). Angiography demonstrated a 25 by 28 mm right ICA aneurysm arising at the origin of the SHA (Fig. 6–2). We anticipated that surgical treatment would require prolonged temporary occlusion or perhaps permanent carotid sacrifice because of the complexity of the aneurysm; therefore, we delayed surgical treatment until the patient had improved clinically. During a balloon test occlusion, the patient became confused and hemiplegic on the left within 30 seconds of balloon inflation. The patient was placed in the supine position with the head turned 20 degrees to the left. The right cervical carotid bifurcation was exposed and a right frontotemporal (pterional) craniotomy was created. The right radial artery was exposed from the antecubital fossa to the wrist and small side branches were ligated with 3–0 silk sutures and divided. Once the graft was completely dissected out, it was kept in situ and attention was redirected to the cranial wound. The sylvian fissure was opened widely, exposing the entire MCA, carotid bifurcation, and proximal ICA. The giant aneurysm was exposed, but the anterior clinoid process and dural rings obscured the proximal portion of the aneurysm. The radial artery was harvested and distended forcibly with heparinized saline to prevent vasospasm. The distal end of the graft was fish-mouthed and brought into the cranial wound where a suitable M2 recipient vessel was identified. The patient’s body temperature had been allowed to drop to 33 °C, a barbiturate infusion was begun, and the patient was heparinized. Temporary clips were placed on either side of the planned anastomosis site on the MCA and an arteriotomy was created with an ophthalmic knife. Using an 8–0 monofilament suture, each end of the radial artery was sutured to the MCA and the long arms were used to complete the anastomosis in a running fashion. Prior to removing the temporary clips, the graft was filled with heparinized saline and a temporary clip was placed on the proximal end of the radial artery. Upon removing the temporary clips from the MCA, the graft pulsated spontaneously. The radial artery graft was tunneled from the cranial to the cervical wound superficial to the zygomatic arch using a chest tube. An end-to-side anastomosis of the graft to the ECA was selected to minimize ICA occlusion time. Temporary clips were placed on the ECA just distal to the carotid bifurcation, and an arteriotomy was created. A small ellipse was excised with microscissors. The proximal end of the radial artery graft was anastomosed to the ECA in an endto-side fashion using interrupted 6–0 prolene sutures. FIGURE 6–1 Noncontrast computed tomography demonstrating subarachnoid blood in both the sylvian fissure and the interhemispheric fissure and early evidence of hydrocephalus. Attention was redirected to the cranial wound. Self-retaining retractors were used to maintain exposure of the giant aneurysm. The dura over the anterior clinoid process was opened with a No. 11 knife blade and the anterior clinoid process and optic canal were completely removed to expose the clinoidal segment of the carotid and the extradural portion of the optic nerve. The optic nerve was markedly distorted at the falciform ligament and draped over the giant aneurysm. The distal dural ring was opened sharply, along with the falciform ligament to free the optic nerve and clinoidal segment of the carotid. This exposed the proximal aspect of the neck of the aneurysm and the origin of the ophthalmic artery. The aneurysm was quite large and adherent to all surrounding structures. In its fully inflated state, it could not be clipped. A temporary clip was placed on the cervical ICA and another intracranially just distal to the aneurysm. The cervical ICA was then cannulated with an intravenous catheter attached to tubing and the aneurysm was suction-decompressed. In its collapsed state, the final stages of dissection were completed and multiple fenestrated clips were used to reconstruct the lumen of the ICA and obliterate the neck of the aneurysm. The temporary clips were removed following clip reconstruction and the carotid artery appeared to pulsate nicely. Intraoperative angiography demonstrated excellent filling of the bypass graft and ICA. Although the vast majority of the aneurysm was occluded, there was a small remnant of very proximal aneurysm continuing to fill. Using intraoperative angiography as a guide, the clip array was reconfigured until the aneurysm was completely obliterated and the parent artery reconstructed satisfactorily. During these attempts, two intraoperative angiograms demonstrated occlusion of the ICA but excellent filling through the bypass graft, protecting the brain from ischemia (Fig. 6–3).
Giant Internal Carotid Artery–Superior Hypophyseal Artery Aneurysm
Clinical Presentation
Surgical Procedure
Postoperative Course and Outcome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree