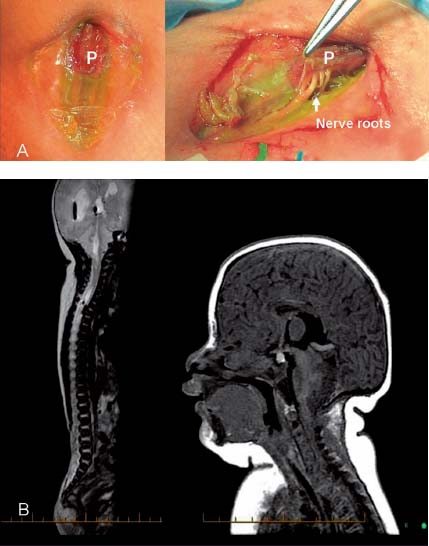
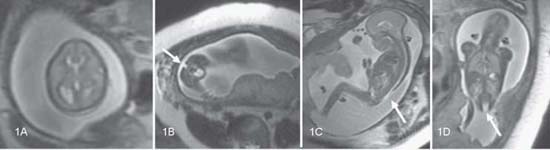
Case 71 Neural Tube Defect Fig. 71.1 Prenatal magnetic resonance imaging scans with (A) T2-weighted axial and (B) sagittal sections of the brain in utero. (C) T2-weighted sagittal and (D) coronal sections of the spine are also shown. Fig. 71.2 (A) Preoperative and intraoperative photograph of the skin defect depicting neural placode (P) and nerve roots. (B) Magnetic resonance imaging scans obtained shortly after birth with sagittal T2-weighted image of the spine and T1-weighted image of the brain.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
71 Neural Tube Defect
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree