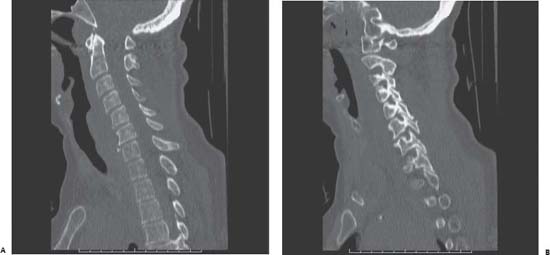
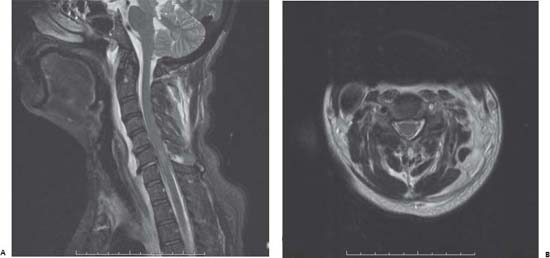
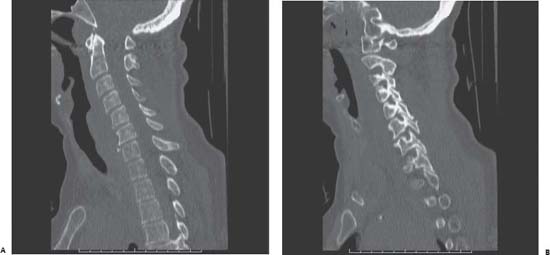
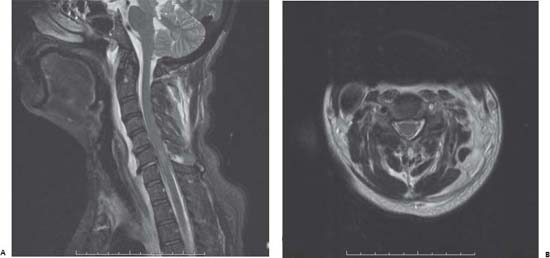
Section II Spinal and Peripheral Nerve Pathology Joseph A. Shehadi and Brian Seaman Fig. 81.1 Computed tomography scan of the cervical spine with (A) midsagittal view and (B) parasagittal view through the left-sided facet joints. Fig. 81.2 Magnetic resonance imaging scan of the cervical spine with (A) sagittal T2-weighted image and (B) axial T2-weighted image at the level of C6. Fig. 81.3 Angiogram of the left vertebral artery demonstrating a marked luminal irregularity and filling defect which begins ~3–4 cm beyond its origin from the subclavian artery and extends cephalad ~3 cm at the level of the patient’s cer vical spine injury. You decide that surgical intervention is indicated for this patient. This would allow for safe and expedient mobilization, as well as preservation of the neural elements. Prior to surgical intervention, an angiogram of the cervical vessels was completed, which demonstrated a dissected left vertebral artery (Fig. 81.3). The patient successfully underwent a combined anterior and posterior cervical fusion. Antiplatelet therapy was initiated to treat the vertebral artery dissection. Gabapentin was initiated for the treatment of the patient’s neuropathic sensory complaints.
Case 81 Lower Cervical Fracture Dislocation
 Clinical Presentation
Clinical Presentation

 Questions
Questions
 Answers
Answers
81 Lower Cervical Fracture Dislocation
Section II Spinal and Peripheral Nerve Pathology Fig. 81.1 Computed tomography scan of the cervical spine with (A) midsagittal view and (B) parasagittal view through the left-sided facet joints. Fig. 81.2 Magnetic resonance imaging scan of the cervical spine with (A) sagittal T2-weighted image and (B) axial T2-weighted image at the level of C6. Fig. 81.3 Angiogram of the left vertebral artery demonstrating a marked luminal irregularity and filling defect which begins ~3–4 cm beyond its origin from the subclavian artery and extends cephalad ~3 cm at the level of the patient’s cer vical spine injury.
Case 81 Lower Cervical Fracture Dislocation
 Clinical Presentation
Clinical Presentation

 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


