Case 83 Type 2 Odontoid Fracture
Joseph A. Shehadi and Brian Seaman
Fig. 83.1 Lateral cervical spine x-ray.
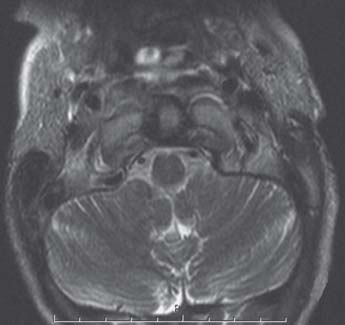
Fig. 83.2 Axial magnetic resonance imaging scan of cervical spine demonstrating transverse ligament.
Fig. 83.3 Postoperative plain lateral cervical spine radiograph demonstrating odontoid screw in place.
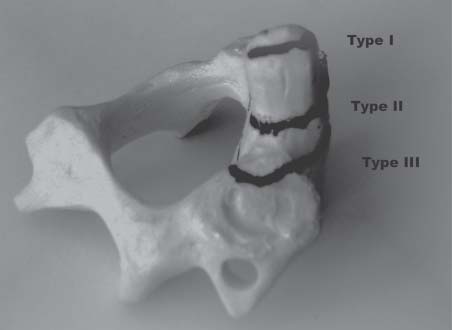
Fig. 83.4 Classification of odontoid fractures.
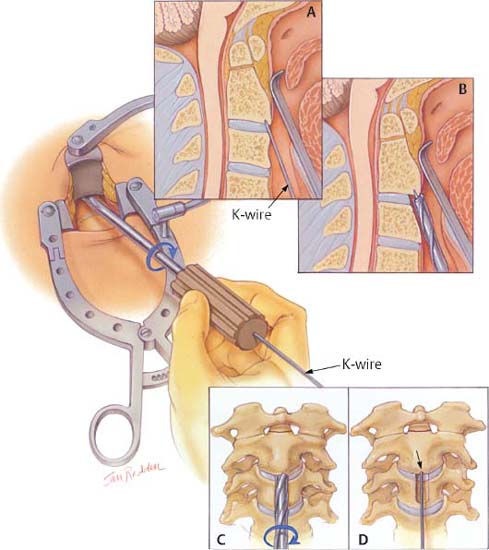
Fig. 83.5 Artist’s rendering of odontoid screw placement technique. (A) K-wire is placed entering at the anteroinferior edge of C2 and aimed toward the odontoid tip under fluoroscopy. (B) This is followed by drilling a hole core over the K-wire. (C,D) Part of the C2–C3 anulus is removed with the coring drill. (From Wolfla CE, Resnick DK. Neurosurgical Operative Atlas. Spine and Peripheral Nerves. New York: Thieme/American Association of Neurological Surgeons; 2006:33. Reprinted with permission.)
- A 76-year-old woman is involved in a motor vehicle accident. She sustained multiple rib fractures and pelvis fractures. She also complains of severe neck pain.
- Her neurologic exam is unremarkable.
- You are asked to consult on this patient regarding a cervical spine fracture seen on radiographs (Fig. 83.1).
< div class='tao-gold-member'>

 Clinical Presentation
Clinical Presentation Questions
Questions Answers
Answers


