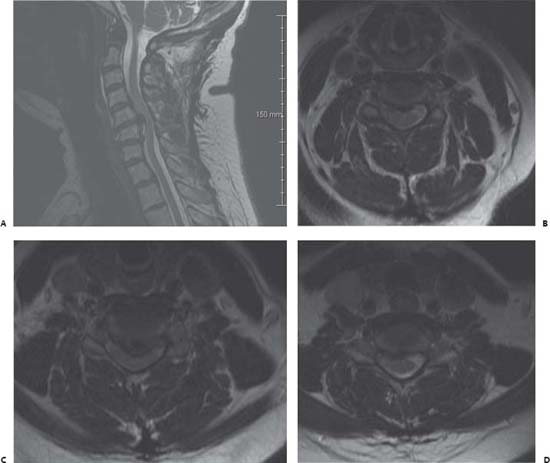
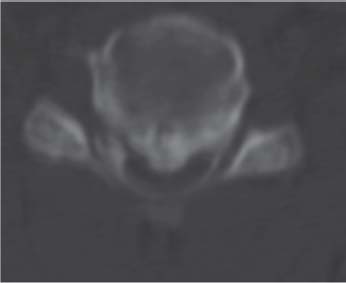
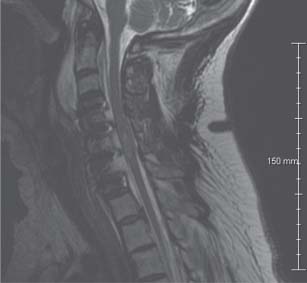
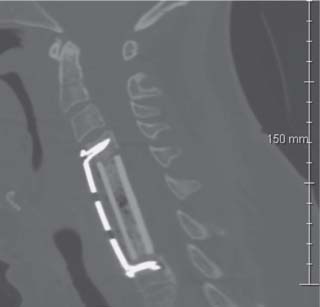
Case 87 Cervical Spondylotic Myelopathy Fig. 87.1 Magnetic resonance imaging of the cervical spine with T2-weighted images: (A) Midsagittal cut and axial cuts through the disk spaces at (B) C4–C5, (C) C5–C6, and (D) C6–C7. Fig. 87.2 Axial computed tomography scan at C5–C6 level. Fig. 87.3 Sagittal T2-weighted magnetic resonance image of cervical spine obtained immediately postoperatively. Fig. 87.4 Computed tomography scan sagittal reconstructed images through cer vical spine. Fig. 87.5 Computed tomography scan sagittal reconstructed images through cervical spine obtained after the second procedure, showing repair of the kyphosis, alignment restoration, and decompression of the spinal cord.
 Clinical Presentation
Clinical Presentation
 Questions
Questions

 Answers
Answers
< div class='tao-gold-member'>
87 Cervical Spondylotic Myelopathy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


